Korean Circ J.
2010 Feb;40(2):68-73. 10.4070/kcj.2010.40.2.68.
Periprocedural Hemoglobin Drop and Contrast-Induced Nephropathy in Percutaneous Coronary Intervention Patients
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea. medorche@chonbuk.ac.kr
- 2Division of Nephrology, Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 2297941
- DOI: http://doi.org/10.4070/kcj.2010.40.2.68
Abstract
- BACKGROUND AND OBJECTIVES
The development of contrast-induced nephropathy (CIN) is associated with an increased risk of death and late cardiovascular events after percutaneous coronary intervention (PCI). The relationship between CIN and hemoglobin drop has been controversial. The aim of this study was to evaluate the clinical usefulness of periprocedural hemoglobin drop as a nontraditional risk factor for CIN.
SUBJECTS AND METHODS
Five-hundred thirty-seven patients who underwent PCI were divided into 2 groups: Group I (486 patients: patients who did not develop CIN) and Group II (51 patients: patients who developed CIN). All patients were administered iodixanol as contrast media during coronary angiography. CIN is defined as a rise in serum creatinine of > or =25% or > or =0.5 mg/dL above the baseline value within 48 hours after contrast administration.
RESULTS
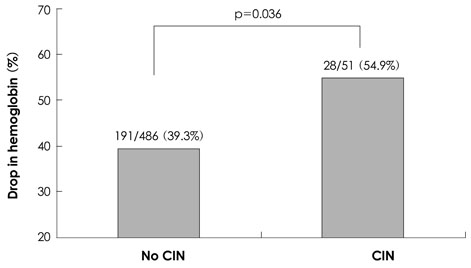
Baseline clinical and cardiovascular risk factors were not significantly different between the two groups, except for low abdominal circumference (Group I : Group II=87.9+/-9.0 cm : 81.2+/-15.1 cm, p=0.024), body weight (Group I : Group II=63.5+/-10.6 kg : 59.7+/-9.2 kg, p=0.008), body mass index (BMI) (Group I : Group II=24.4+/-3.4 kg/m2 : 23.4+/-2.8 kg/m2, p=0.032), pre-PCI hemoglobin (Group I : Group II=13.2+/-2.0 g/dL : 12.3+/-2.0 g/dL, p=0.003), and post-PCI hemoglobin (Group I : Group II=12.4+/-1.9 g/dL : 11.5+/-1.8 g/dL, p=0.001). Multiple logistic regression analysis showed that a periprocedural drop in hemoglobin (>1 g/dL) was an independent predictor of CIN, like other known risk factors.
CONCLUSION
A periprocedural drop in hemoglobin of more than 1 g/dL is another important independent predictor for CIN, even in patients administered the lowest nephrotoxic contrast agent, iodixanol, during PCI.
Keyword
MeSH Terms
Figure
Reference
-
1. Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002. 105:2259–2264.2. Lee SH, Chae JK, Lee KH, et al. Full metal jackets (≥60 mm) of drug-eluting stents: short- and long-term clinical and angiographic outcomes. Korean Circ J. 2008. 38:87–94.3. Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital acquired renal insufficiency: a prospective study. Am J Med. 1983. 74:243–248.4. Marenzi G, Assanelli E, Marana I, et al. N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med. 2006. 354:2773–2782.5. Sadeghi HM, Stone GW, Grines CL, et al. Impact of renal insufficiency in patients undergoing primary angioplasty for acute myocardial infarction. Circulation. 2003. 108:2769–2775.6. Marenzi G, Lauri G, Assanelli E, et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2004. 44:1780–1785.7. Namgung J, Doh JH, Lee SY, Huh WS, Park SW, Lee WR. Effect of N-acetylcysteine in prevention of contrast-induced nephropathy after coronary angiography. Korean Circ J. 2005. 35:696–701.8. Kim U, Kim YJ, Lee WJ, et al. The estimated glomerular filtration rate with using the mayo clinic quadratic equation as a new predictor for developing contrast induced nephropathy in patients with angina pectoris. Korean Circ J. 2008. 38:301–304.9. Thomsen HS. Guidelines for contrast media from the European Society of Urogenital Radiology. AJR Am J Roentgenol. 2003. 181:1463–1471.10. Morcos SK, Thomsen HS. European Society of Urogenital Radiology guidelines on administering contrast media. Abdom Imaging. 2003. 28:187–190.11. Parfrey PS, Griffiths SM, Barrett BJ, et al. Contrast material induced renal failure in patients with diabetes mellitus, renal insufficiency, or both: a prospective controlled study. N Engl J Med. 1989. 320:143–149.12. McCullough PA, Adam A, Becker CR, et al. Risk prediction of contrast-induced nephropathy. Am J Cardiol. 2006. 98:27K–36K.13. Dangas G, Iakovou I, Nikolsky E, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005. 95:13–19.14. Schweiger MJ, Chambers CE, Davidson CJ, et al. Prevention of contrast induced nephropathy: recommendations for the high risk patient undergoing cardiovascular procedures. Catheter Cardiovasc Interv. 2007. 69:135–140.15. Bartholomew BA, Harjai KJ, Dukkipati S, et al. Impact of nephropathy after percutaneous coronary intervention and a method for risk stratification. Am J Cardiol. 2004. 93:1515–1519.16. Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004. 44:1393–1399.17. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction). J Am Coll Cardiol. 2007. 50:e1–e157.18. Ryan TJ, Faxon DP, Gunnar RM, et al. Guidelines for percutaneous transluminal coronary angioplasty: a report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation. 1988. 78:486–502.19. King SB 3rd, Smith SC Jr, Hirshfeld JW Jr, et al. 2007 focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol. 2008. 51:172–209.20. Nikolsky E, Mehran R, Lasic Z, et al. Low hematocrit predicts contrast-induced nephropathy after percutaneous coronary interventions. Kidney Int. 2005. 67:706–713.21. McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol. 2008. 51:1419–1428.22. Toprak O, Cirit M. Risk factors for contrast-induced nephropathy. Kidney Blood Press Res. 2006. 29:84–93.23. Pucelikova T, Dangas G, Mehran R. Contrast-induced nephropathy. Catheter Cardiovasc Interv. 2008. 71:62–72.24. Dangas G, Iakovou I, Nikolsky E, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005. 95:13–19.25. Rich MW, Crecelius CA. Incidence, risk factors, and clinical course of acute renal insufficiency after cardiac catheterization in patients 70 years of age or older: a prospective study. Arch Intern Med. 1990. 150:1237–1242.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Markers of Contrast Induced Nephropathy after the Percutaneous Coronary Intervention
- Successful Treatment of Unprotected Left Main Coronary Bifurcation Lesion Using Minimum Contrast Volume with Intravascular Ultrasound Guidance
- Incidence, Risk factors, and Clinical Outcomes of Contrast Induced Nephropathy After Percutaneous Coronary Intervention in Elderly Patients
- Contrast Induced Nephropathy and 2-Year Outcomes of Iso-Osmolar Compared with Low-Osmolar Contrast Media after Elective Percutaneous Coronary Intervention
- Determination of Safe Contrast Media Dosage to Estimated Glomerular Filtration Rate Ratios to Avoid Contrast-Induced Nephropathy After Elective Percutaneous Coronary Intervention