Effects of Age, Sex, and Menopausal Status on Blood Cholesterol Profile in the Korean Population
- Affiliations
-
- 1Department of Public Health, Yonsei University Graduate School, Seoul, Korea.
- 2Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea. hckim@yuhs.ac
- 3Cardiovascular and Metabolic Diseases Etiology Research Center, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2297881
- DOI: http://doi.org/10.4070/kcj.2015.45.2.141
Abstract
- BACKGROUND AND OBJECTIVES
To investigate age-specific and sex-specific distributions of blood cholesterol in the general Korean population.
SUBJECTS AND METHODS
We analyzed data for 8284 men and 9246 women aged > or =10 years who participated in the fifth (2010-2012) Korea National Health and Nutrition Examination Survey. Age-specific means, medians, and selected percentiles were calculated for men, premenopausal women, and postmenopausal women.
RESULTS
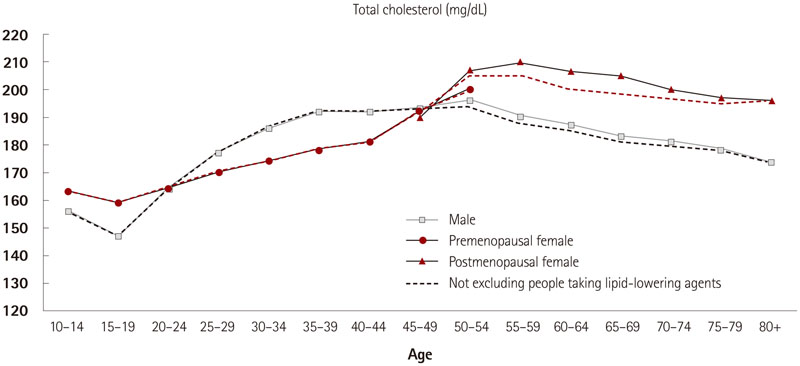
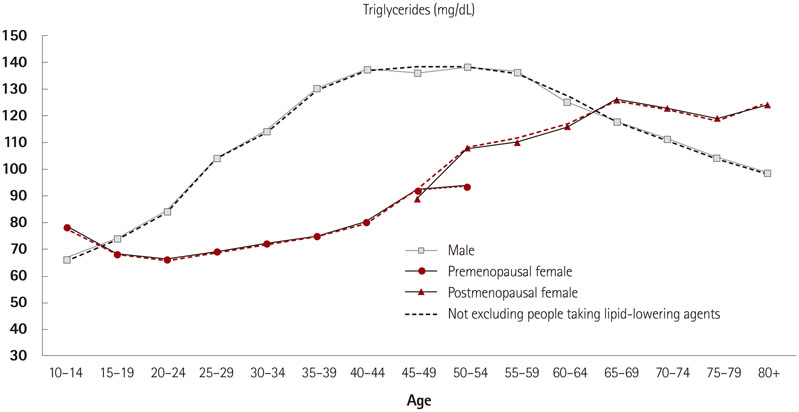
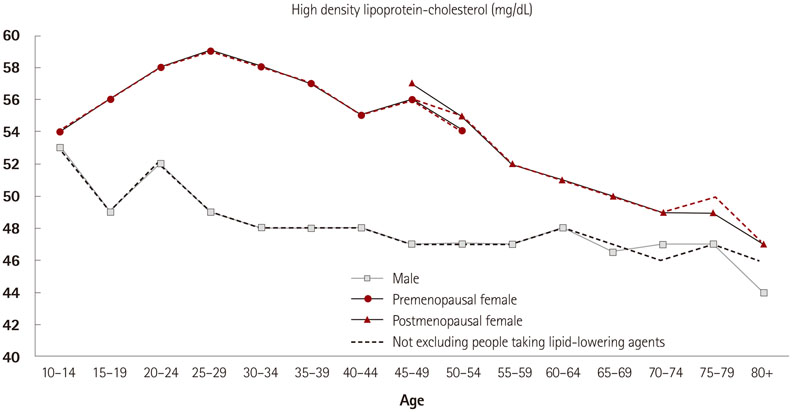
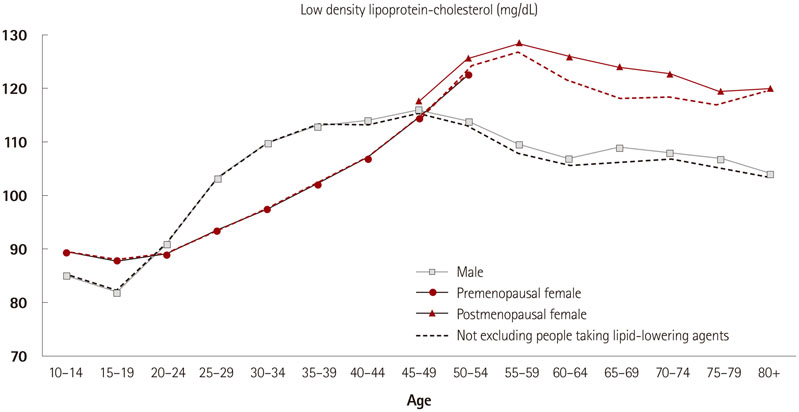
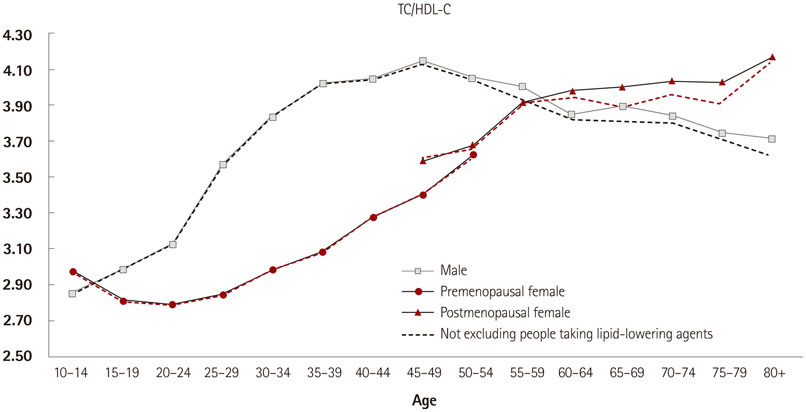
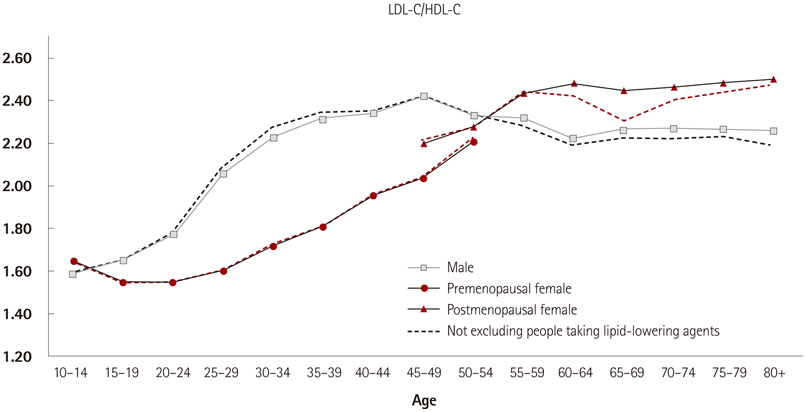
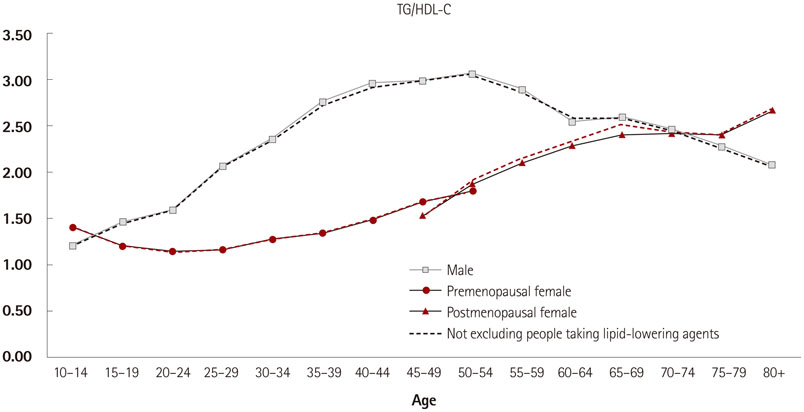
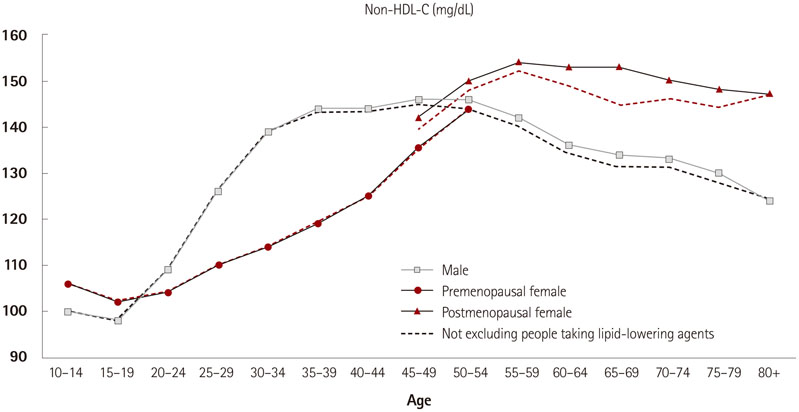
Median total cholesterol (TC) level increased with age across all age groups, from 147 to 196 mg/dL in males and from 159 to 210 mg/dL in females. Triglyceride (TG) levels increased with age in females; however, in males, TG levels rapidly increased during young adulthood, peaked at 50-54 years, and then decreased. High density lipoprotein-cholesterol (HDL-C) levels were higher in females than in males and decreased with increasing age in both males and females. Low density lipoprotein-cholesterol (LDL-C) levels increased with age across all age groups, from 89 to 127 mg/dL in males and from 82 to 113 mg/dL in females. Lipoprotein-cholesterol fraction (TC/HDL-C, LDL-C/HDL-C, TG/HDL-C, non-HDL-C) levels increased with age in females, but increased more rapidly in males during young adulthood and decreased after middle age.
CONCLUSION
Blood cholesterol levels and lipoprotein-cholesterol fractions present different distributions by age, sex, and menopausal status.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Epidemiology of dyslipidemia in Korea
Hyeon Chang Kim
J Korean Med Assoc. 2016;59(5):352-357. doi: 10.5124/jkma.2016.59.5.352.Dyslipidemia in Older Adults and Management of Dyslipidemia in Older Patients
Kwang-il Kim
J Lipid Atheroscler. 2015;4(1):1-6. doi: 10.12997/jla.2015.4.1.1.2018 Guidelines for the Management of Dyslipidemia in Korea
Eun-Jung Rhee, Hyeon Chang Kim, Jae Hyeon Kim, Eun Young Lee, Byung Jin Kim, Eun Mi Kim, YoonJu Song, Jeong Hyun Lim, Hae Jin Kim, Seonghoon Choi, Min Kyong Moon, Jin Oh Na, Kwang-Yeol Park, Mi Sun Oh, Sang Youb Han, Junghyun Noh, Kyung Hee Yi, Sang-Hak Lee, Soon-Cheol Hong, In-Kyung Jeong,
J Lipid Atheroscler. 2019;8(2):78-131. doi: 10.12997/jla.2019.8.2.78.Myocardial Infarction, Stroke, and All-Cause Mortality according to Low-Density Lipoprotein Cholesterol Level in the Elderly, a Nationwide Study
You-Bin Lee, Minji Koo, Eunjin Noh, Soon Young Hwang, Jung A Kim, Eun Roh, So-hyeon Hong, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Diabetes Metab J. 2022;46(5):722-732. doi: 10.4093/dmj.2021.0225.
Reference
-
1. Farzadfar F, Finucane MM, Danaei G, et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. Lancet. 2011; 377:578–586.2. Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 1986; 256:2823–2828.3. Natarajan S, Glick H, Criqui M, Horowitz D, Lipsitz SR, Kinosian B. Cholesterol measures to identify and treat individuals at risk for coronary heart disease. Am J Prev Med. 2003; 25:50–57.4. Gordon DJ, Probstfield JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989; 79:8–15.5. Kinosian B, Glick H, Preiss L, Puder KL. Cholesterol and coronary heart disease: predicting risks in men by changes in levels and ratios. J Investig Med. 1995; 43:443–450.6. Kastelein JJ, van der Steeg WA, Holme I, et al. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation. 2008; 117:3002–3009.7. Anderson KM, Wilson PW, Odell PM, Kannel WB. An updated coronary risk profile. A statement for health professionals. Circulation. 1991; 83:356–362.8. Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk. 1996; 3:213–219.9. Assmann G, Schulte H, Funke H, von Eckardstein A. The emergence of triglycerides as a significant independent risk factor in coronary artery disease. Eur Heart J. 1998; 19:Suppl M. M8–M14.10. Malik S, Wong ND, Franklin SS, et al. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004; 110:1245–1250.11. Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005; 165:2644–2650.12. Gaziano JM, Hennekens CH, O'Donnell CJ, Breslow JL, Buring JE. Fasting triglycerides, high-density lipoprotein, and risk of myocardial infarction. Circulation. 1997; 96:2520–2525.13. Packard CJ, Saito Y. Non-HDL cholesterol as a measure of atherosclerotic risk. J Atheroscler Thromb. 2004; 11:6–14.14. Lee MH, Kim HC, Ahn SV, et al. Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005. Diabetes Metab J. 2012; 36:43–55.15. Roh E, Ko SH, Kwon HS, et al. Prevalence and Management of Dyslipidemia in Korea: Korea National Health and Nutrition Examination Survey during 1998 to 2010. Diabetes Metab J. 2013; 37:433–449.16. Nam GE, Han K, Park YG, et al. Trends in lipid profiles among South Korean adults: 2005, 2008 and 2010 Korea National Health and Nutrition Examination Survey. J Public Health (Oxf). 2014; 02. 25. [Epub]. http://dx.doi.org/10.1093/pubmed/fdu012.17. Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.18. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502.19. Castelli WP. Cholesterol and lipids in the risk of coronary artery disease--the Framingham Heart Study. Can J Cardiol. 1988; 4:Suppl A. 5A–10A.20. Kosmas CE, Christodoulidis G, Cheng JW, Vittorio TJ, Lerakis S. High-density lipoprotein functionality in coronary artery disease. Am J Med Sci. 2014; 347:504–508.21. Assmann G, Schulte H, von Eckardstein A, Huang Y. High-density lipoprotein cholesterol as a predictor of coronary heart disease risk. The PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis. 1996; 124:S11–S20.22. Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988-2010. JAMA. 2012; 308:1545–1554.23. Yano Y, Irie N, Homma Y, et al. High density lipoprotein cholesterol levels in the Japanese. Atherosclerosis. 1980; 36:173–181.24. Turley ML, Skeaff CM, Mann JI, Cox B. The effect of a low-fat, high-carbohydrate diet on serum high density lipoprotein cholesterol and triglyceride. Eur J Clin Nutr. 1998; 52:728–732.25. Feinleib M, Garrison RJ, Fabsitz R, et al. The NHLBI twin study of cardiovascular disease risk factors: methodology and summary of results. Am J Epidemiol. 1977; 106:284–285.26. Schaefer EJ, Levy RI, Ernst ND, Van Sant FD, Brewer HB Jr. The effects of low cholesterol, high polyunsaturated fat, and low fat diets on plasma lipid and lipoprotein cholesterol levels in normal and hypercholesterolemic subjects. Am J Clin Nutr. 1981; 34:1758–1763.27. Sanders K, Johnson L, O'Dea K, Sinclair AJ. The effect of dietary fat level and quality on plasma lipoprotein lipids and plasma fatty acids in normocholesterolemic subjects. Lipids. 1994; 29:129–138.28. Schaefer EJ, Lamon-Fava S, Cohn SD, et al. Effects of age, gender, and menopausal status on plasma low density lipoprotein cholesterol and apolipoprotein B levels in the Framingham Offspring Study. J Lipid Res. 1994; 35:779–792.29. Granfone A, Campos H, McNamara JR, et al. Effects of estrogen replacement on plasma lipoproteins and apolipoproteins in postmenopausal, dyslipidemic women. Metabolism. 1992; 41:1193–1198.30. Hwang YC, Ahn HY, Jeong IK, Ahn KJ, Chung HY. Optimal range of triglyceride values to estimate serum low density lipoprotein cholesterol concentration in Korean adults: the Korea National Health and Nutrition Examination Survey, 2009. J Korean Med Sci. 2012; 27:1530–1535.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differences of Prevalence and Components of Metabolic Syndrome according to Menopausal Status
- Effects of Koryo Hand Therapy on Menopausal Symptoms and Blood Lipid Levels in Middle-aged Women
- Effects of Nutrition Education with Intervention Mapping on Cardiovascular Disease Risk Factors in Women with Borderline Dyslipidemia: Analysis According to Menopausal Status
- Distribution of Blood Cholesterol Profile in Untreated Korean Population
- Quality of Sleep and Serum Lipid Profile in Patients with Restless Legs Syndrome