J Rheum Dis.
2014 Jun;21(3):156-161. 10.4078/jrd.2014.21.3.156.
An Unusual Case of Severe Neonatal Lupus Mimicking Neonatal Sepsis and Literature Review
- Affiliations
-
- 1Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. jsoh@uuh.ulsan.kr
- 2Department of Pediatrics, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2297529
- DOI: http://doi.org/10.4078/jrd.2014.21.3.156
Abstract
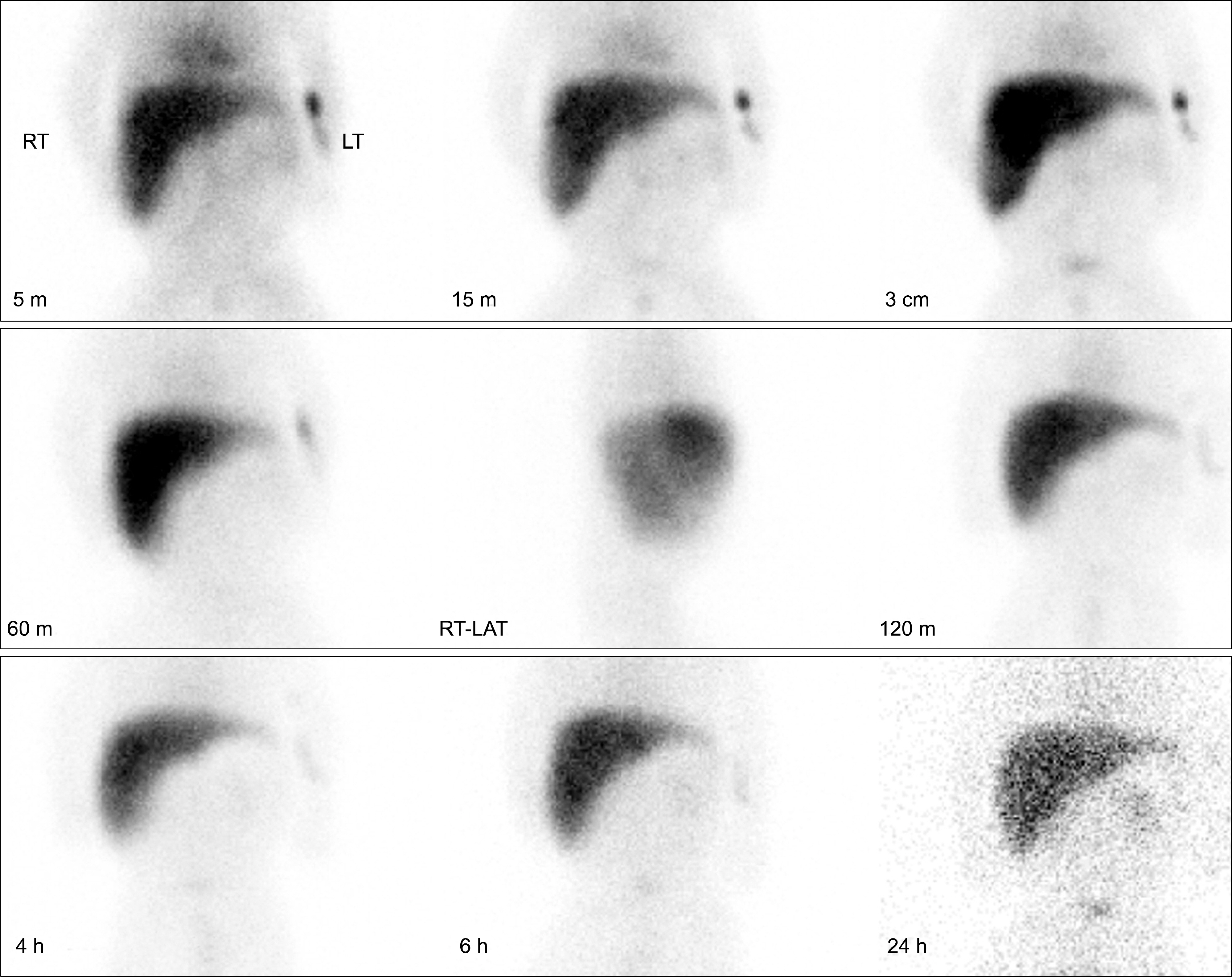
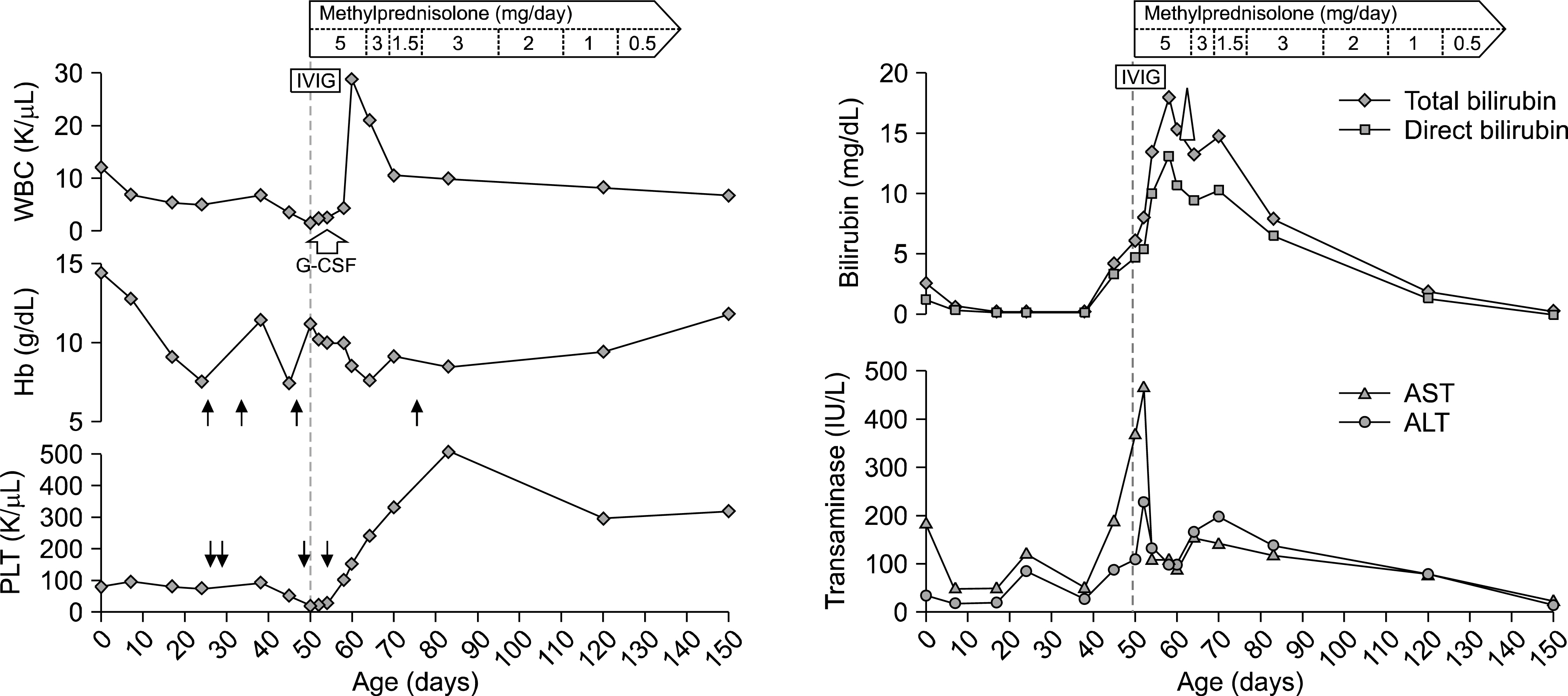
- Neonatal lupus is an uncommon autoimmune disease that results from transplacental passage of the maternal anti-SSA/Ro and/or anti-SSB/La antibodies. Pancytopenia or severe jaundice is a rare manifestation of neonatal lupus, respectively, and could be misdiagnosed with other neonatal illnesses, such as infection, hematologic disease, or hepatobiliary disease. Here, we report an unusual case of a premature newborn with severe neonatal lupus manifested with skin rash, fever, pancytopenia, and severe jaundice with abnormal liver function tests. His mother had been clinically asymptomatic before delivery; however, she revealed peripheral edema, bilateral pleural effusion, and ascites after delivery and diagnosed with systemic lupus erythematosus based on positive anti-nuclear and anti-cardiolipin antibodies, proteinuria, and serositis. The newborn and his mother had anti-SSA/Ro and anti-SSB/La antibodies. His pancytopenia and jaundice were progressively aggravated, and his illness was confused with neonatal sepsis or biliary obstruction. We decided to treat with high dose of corticosteroid and intravenous immunoglobulin, and he gradually recovered completely with the treatment. His corticosteroid was stopped at 5 months of age without relapse or complication.
Keyword
MeSH Terms
Figure
Reference
-
1. Lin SC, Shyur SD, Huang LH, Wu JY, Chuo HT, Lee HC. Neonatal lupus erythematosus with cholestatic hepatitis. J Microbiol Immunol Infect. 2004; 37:131–4.2. Cimaz R, Spence DL, Hornberger L, Silverman ED. Incidence and spectrum of neonatal lupus erythematosus: a prospective study of infants born to mothers with an-ti-Ro autoantibodies. J Pediatr. 2003; 142:678–83.
Article3. Lee LA, Sokol RJ, Buyon JP. Hepatobiliary disease in neonatal lupus: prevalence and clinical characteristics in cases enrolled in a national registry. Pediatrics. 2002; 109:E11.
Article4. Kobayashi R, Mii S, Nakano T, Harada H, Eto H. Neonatal lupus erythematosus in Japan: a review of the literature. Autoimmun Rev. 2009; 8:462–6.
Article5. Lee LA. Neonatal lupus erythematosus. J Invest Dermatol. 1993; 100:9S–13S.
Article6. Chang C. Neonatal autoimmune diseases: a critical review. J Autoimmun. 2012; 38:J223–38.
Article7. Friedman DM, Kim MY, Copel JA, Davis C, Phoon CK, Glickstein JS, et al. PRIDE Investigators. Utility of cardiac monitoring in fetuses at risk for congenital heart block: the PR Interval and Dexamethasone Evaluation (PRIDE) prospective study. Circulation. 2008; 117:485–93.8. Izmirly PM, Llanos C, Lee LA, Askanase A, Kim MY, Buyon JP. Cutaneous manifestations of neonatal lupus and risk of subsequent congenital heart block. Arthritis Rheum. 2010; 62:1153–7.
Article9. Brucato A, Frassi M, Franceschini F, Cimaz R, Faden D, Pisoni MP, et al. Risk of congenital complete heart block in newborns of mothers with anti-Ro/SSA antibodies detected by counterimmunoelectrophoresis: a prospective study of 100 women. Arthritis Rheum. 2001; 44:1832–5.
Article10. Buyon JP, Hiebert R, Copel J, Craft J, Friedman D, Katholi M, et al. Autoimmune-associated congenital heart block: demographics, mortality, morbidity and recurrence rates obtained from a national neonatal lupus registry. J Am Coll Cardiol. 1998; 31:1658–66.
Article11. Llanos C, Izmirly PM, Katholi M, Clancy RM, Friedman DM, Kim MY, et al. Recurrence rates of cardiac manifestations associated with neonatal lupus and maternal/fetal risk factors. Arthritis Rheum. 2009; 60:3091–7.
Article12. Julkunen H, Eronen M. The rate of recurrence of isolated congenital heart block: a population-based study. Arthritis Rheum. 2001; 44:487–8.
Article13. Hochberg MC. Rheumatology. 5th ed.Philadelphia: Mosby;2011.14. Kang HS, Song SE, Ma JS, Choi YY, Song TB. The Clinical Characteristics and Outcome of Neonates born to Systemic Lupus Erythematosus Mothers. J Korean Soc Neonatol. 2006; 13:139–48.15. Baek HS, Choi JH, Kim NS, Kim CR, Moon SJ. Outcome of pregnant mothers with systemic lupus erythematosus (focusing on congenital heart block). Korean J Pediatr. 2006; 49:381–7.
Article16. Lee LA, Weston WL. Cutaneous lupus erythematosus during the neonatal and childhood periods. Lupus. 1997; 6:132–8.
Article17. Silverman E, Jaeggi E. Non-cardiac manifestations of neonatal lupus erythematosus. Scand J Immunol. 2010; 72:223–5.
Article18. Neiman AR, Lee LA, Weston WL, Buyon JP. Cutaneous manifestations of neonatal lupus without heart block: characteristics of mothers and children enrolled in a national registry. J Pediatr. 2000; 137:674–80.
Article19. Watson R, Kang JE, May M, Hudak M, Kickler T, Provost TT. Thrombocytopenia in the neonatal lupus syndrome. Arch Dermatol. 1988; 124:560–3.
Article20. Lockshin MD, Bonfa E, Elkon K, Druzin ML. Neonatal lupus risk to newborns of mothers with systemic lupus erythematosus. Arthritis Rheum. 1988; 31:697–701.
Article21. Wolach B, Choc L, Pomeranz A, Ben Ari Y, Douer D, Metzker A. Aplastic anemia in neonatal lupus erythematosus. Am J Dis Child. 1993; 147:941–4.
Article22. Lee LA. Neonatal lupus: clinical features and management. Paediatr Drugs. 2004; 6:71–8.23. Kanitkar M, Rohini KP, Puri B, Nair MN. Neonatal lupus mimicking extra hepatic biliary atresia. Indian Pediatr. 2004; 41:1252–4.24. Lee SM, Ham SS, Jeon IS, Son DW. Neonatal Lupus Erythematosus Manifests as Pancytopenia and Mildly Abnormal Liver Functions. Korean J Perinatol. 2005; 16:317–21.25. Boh EE. Neonatal lupus erythematosus. Clin Dermatol. 2004; 22:125–8.
Article26. Korkij W, Soltani K. Neonatal lupus erythematosus: a review. Pediatr Dermatol. 1984; 1:189–95.
Article