J Rheum Dis.
2014 Jun;21(3):110-121. 10.4078/jrd.2014.21.3.110.
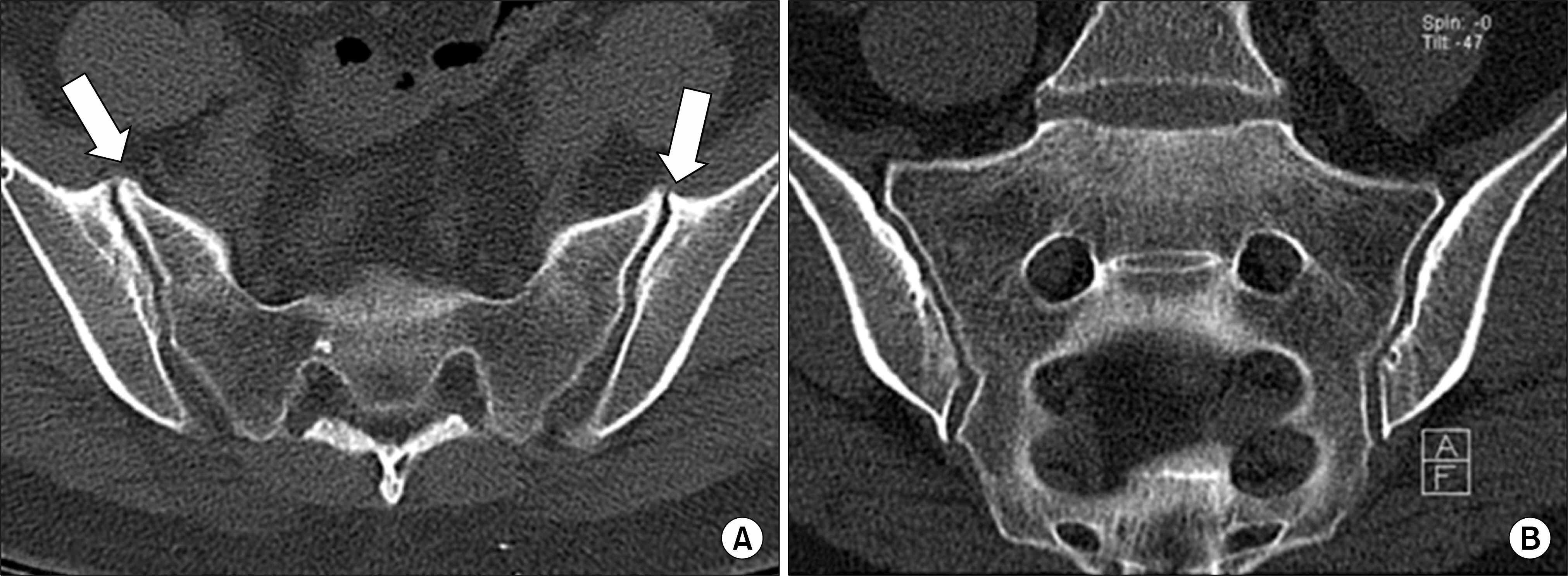
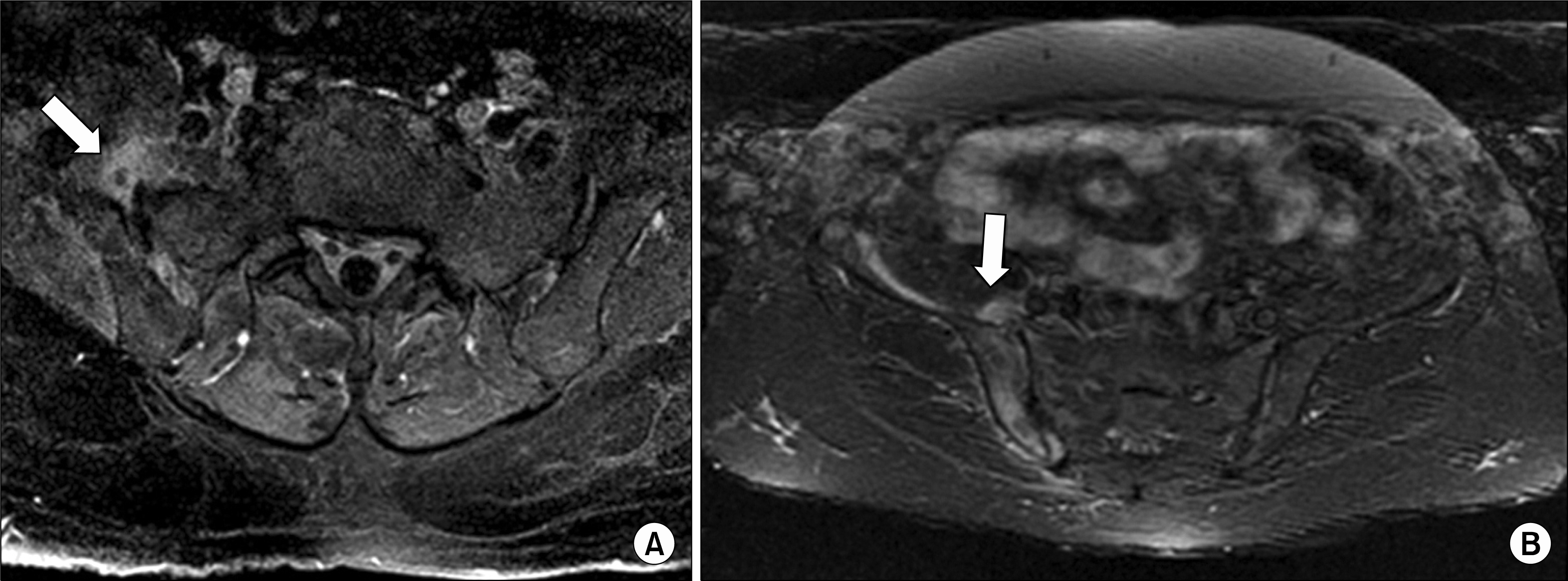
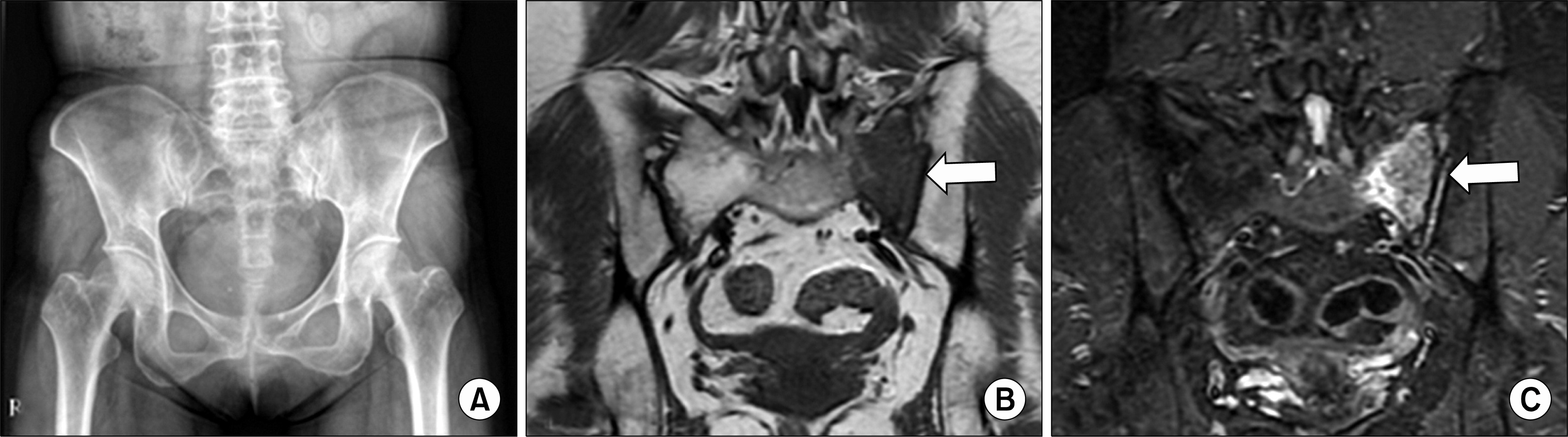
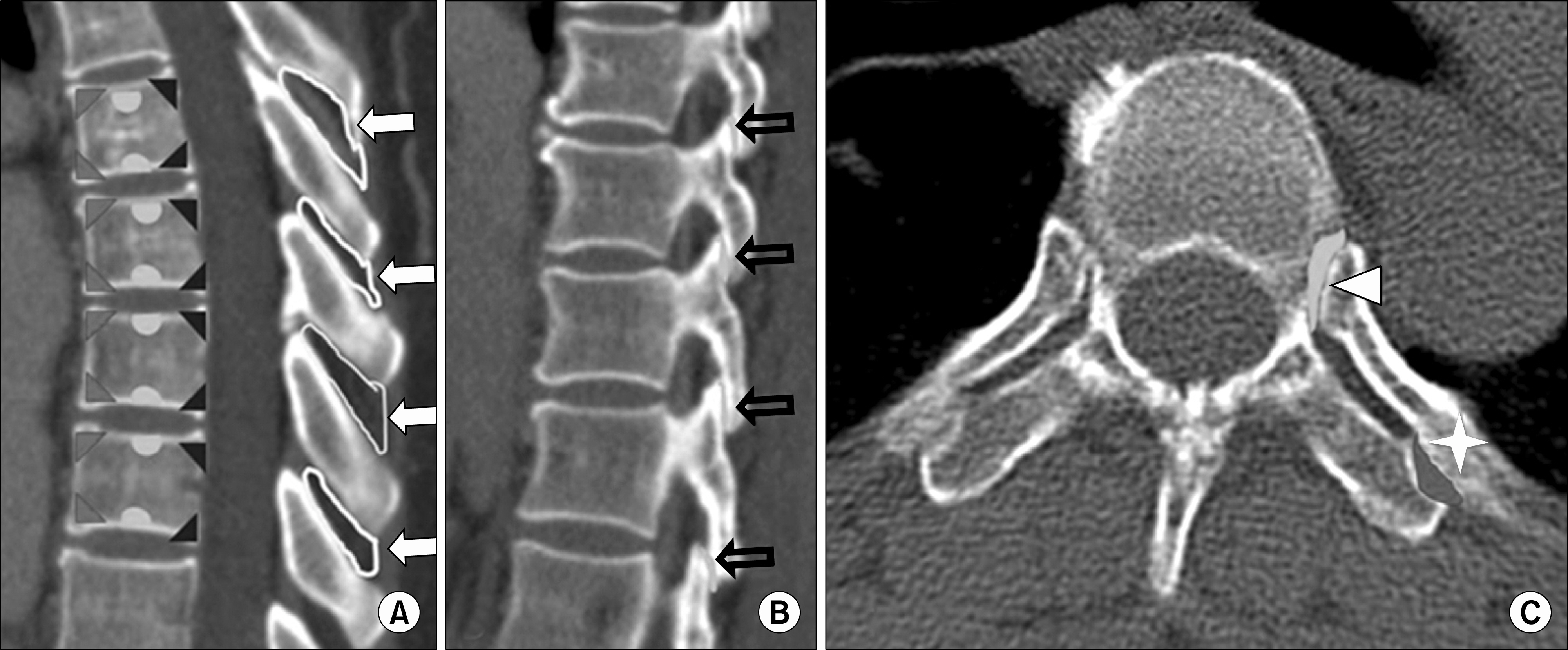
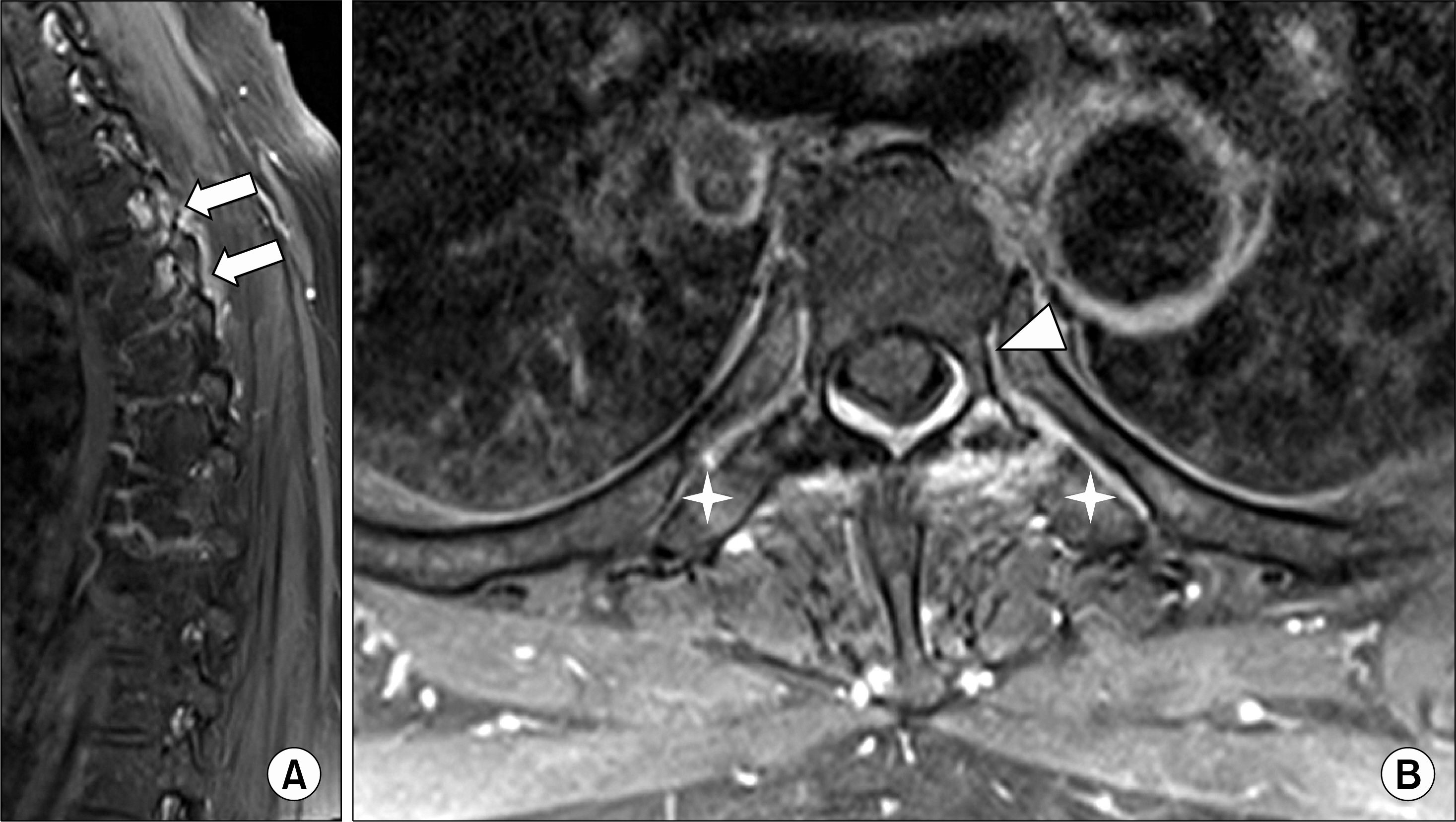
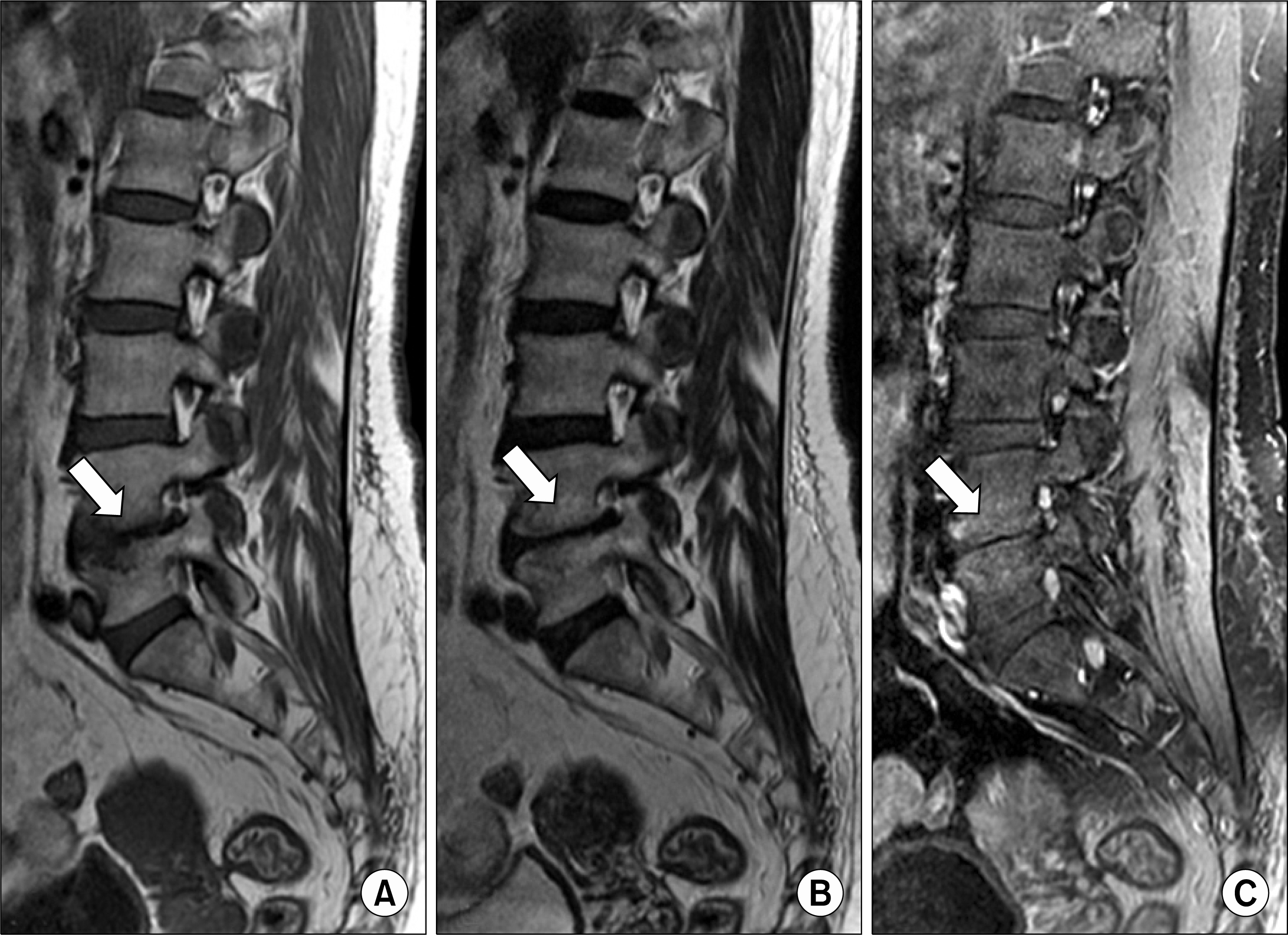
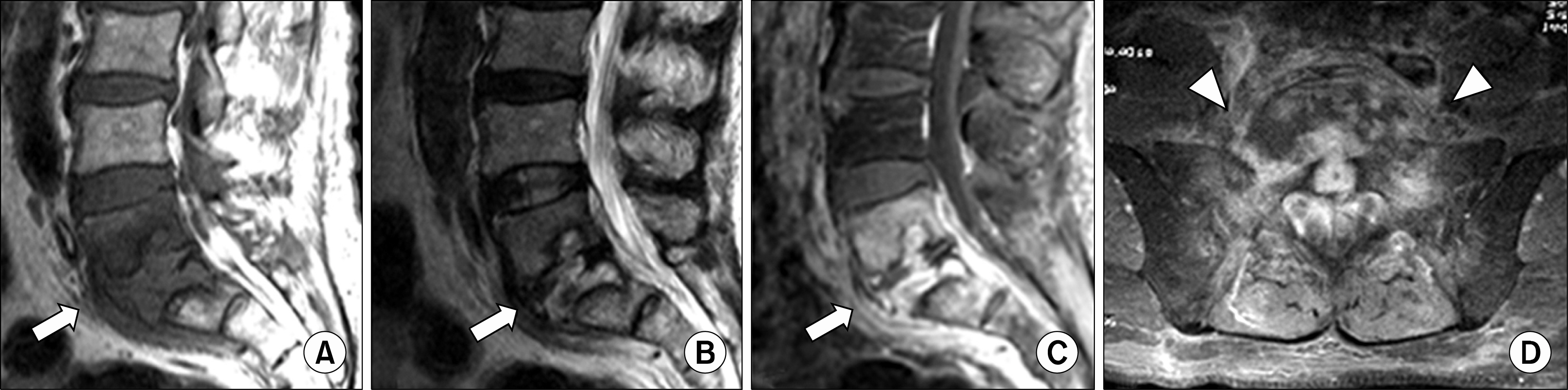
MRI Features of Axial Spondyloarthritis and Differential Diagnosis: Focusing on the Spine and Sacroiliac Joint
- Affiliations
-
- 1Department of Radiology, Hanyang University College of Medicine, Seoul, Korea. radsh@hanyang.ac.kr
- KMID: 2297522
- DOI: http://doi.org/10.4078/jrd.2014.21.3.110
Abstract
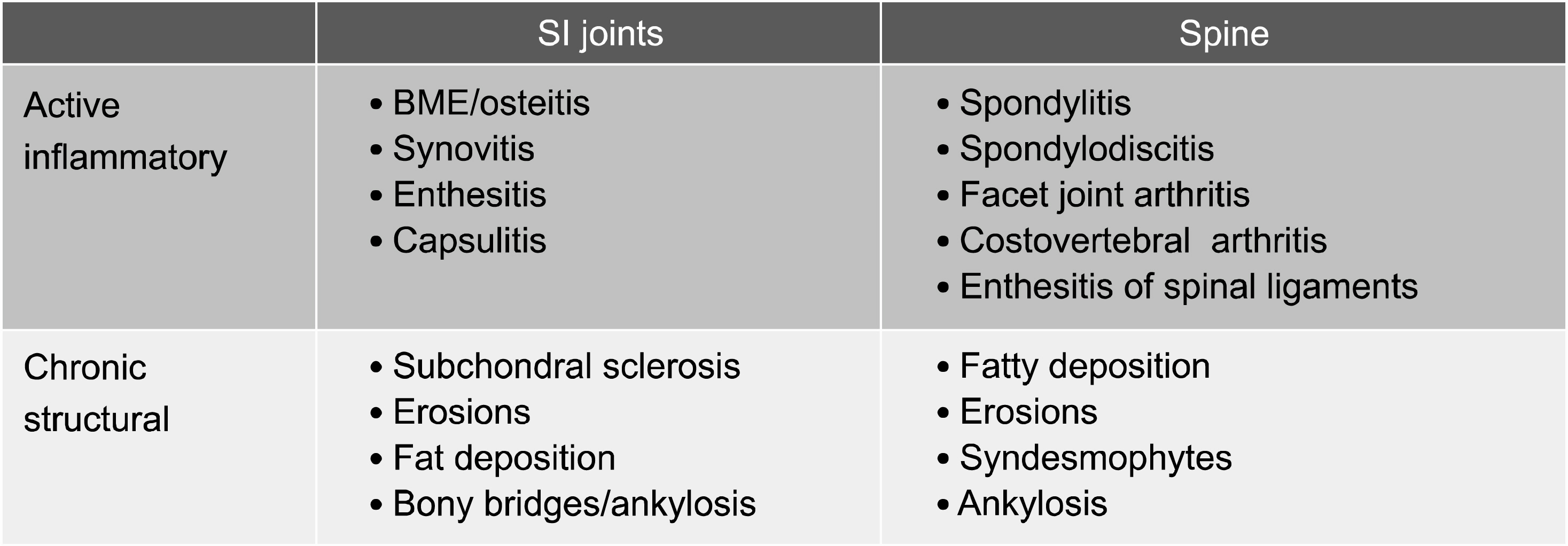
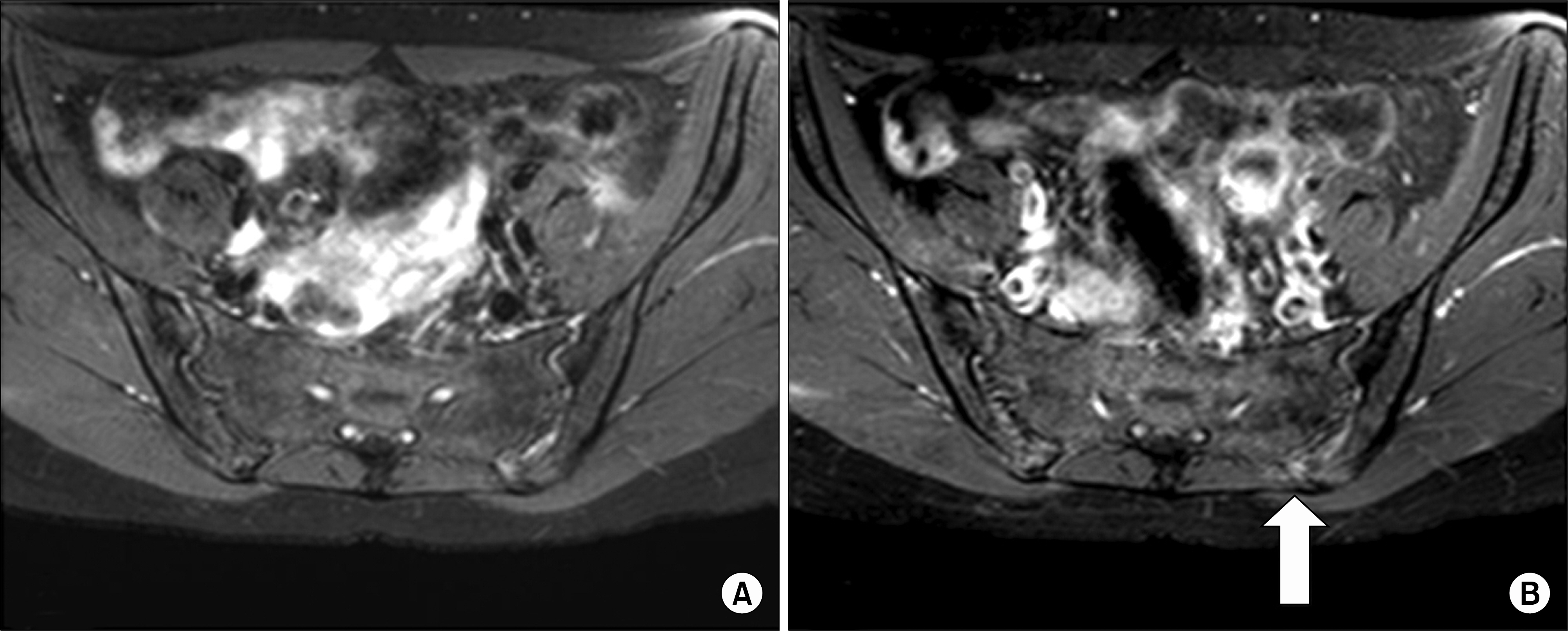
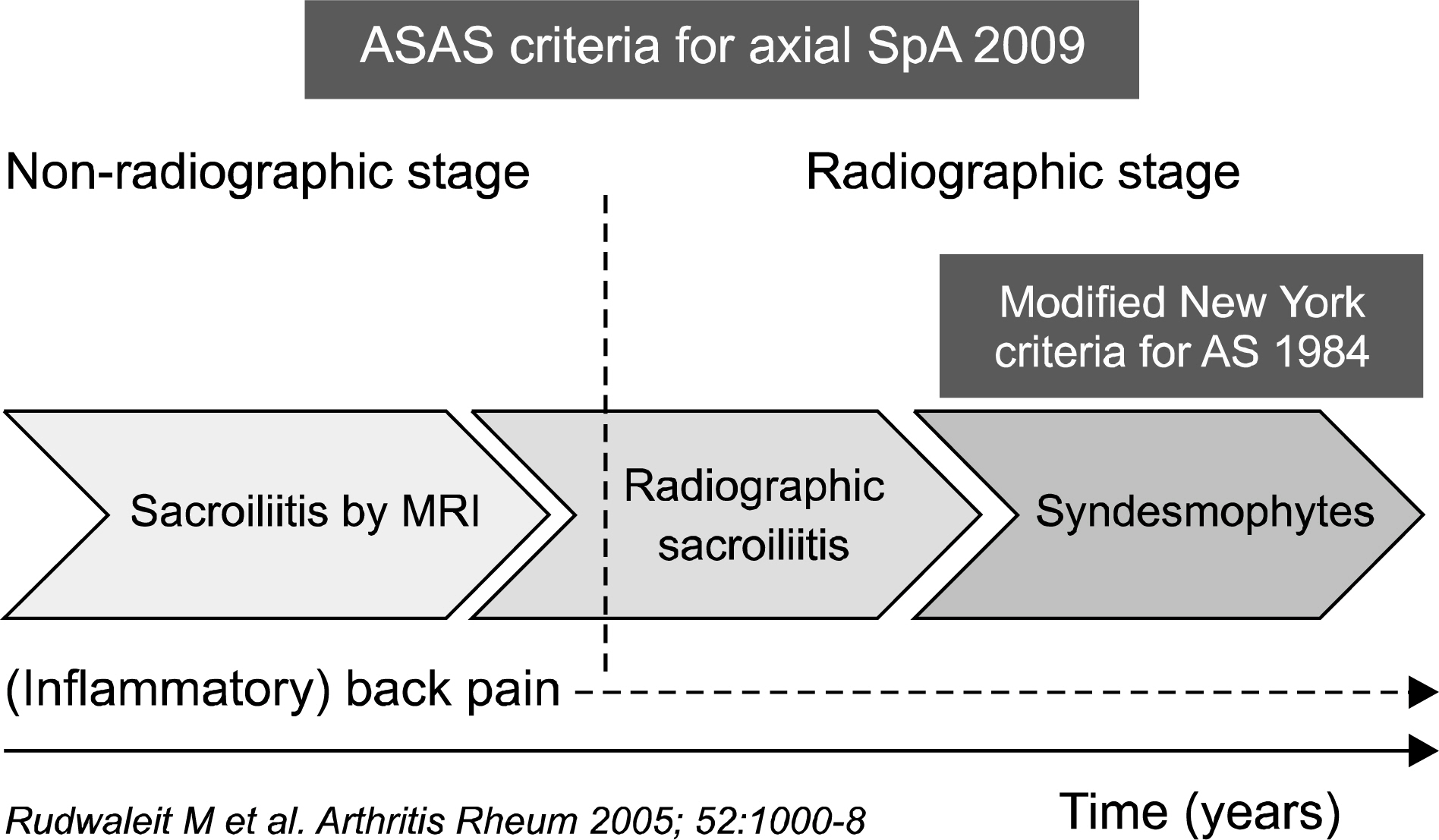
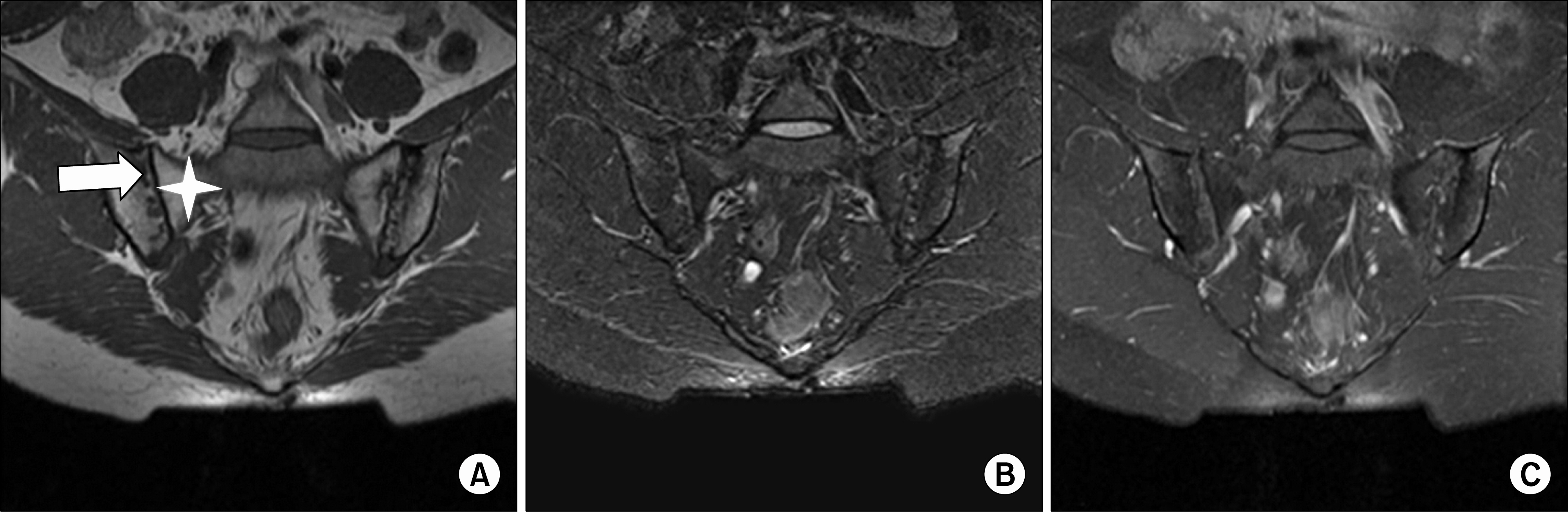
- The spine and sacroiliac joint are involved in most cases of axial spondyloarthritis. Several pathologic findings from a radiography involving the spine and sacroiliac joint are the diagnostic hallmarks of axial spondyloarthritis. However, these radiographic changes reflect structural damage rather than active inflammation, which may delay diagnosis by several years. Nowadays, the Assessment of SpondyloArthritis international Society (ASAS) has focused on the reassessment of existing classification criteria and the development and validation of diagnostic tools to facilitate early diagnosis and assessment of treatment response. Magnetic resonance (MR) findings are the most remarkable changes with respect to the previously established classification criteria. Familiarity with typical MRI findings of axial spondyloarthritis and differential diseases is important in order to correctly interpret the findings and avoid misdiagnosis.
MeSH Terms
Figure
Cited by 1 articles
-
Utility of Magnetic Resonance Imaging and Positron Emission Tomography in Rheumatic Diseases
Eun Hye Park, Chong-Hyeon Yoon, Eun Ha Kang, Han Joo Baek
J Rheum Dis. 2020;27(3):136-151. doi: 10.4078/jrd.2020.27.3..
Reference
-
1. van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984; 27:361–8.2. Dougados M, van der Linden S, Juhlin R, Huitfeldt B, Amor B, Calin A, et al. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991; 34:1218–27.
Article3. Resnick D, Kransdorf MJ. Bone and joint imaging. 3rd ed.p. 267. Philadelphia: Elsevier Saunders;2005.4. Yochum TR, Rowe LJ. Essentials of skeletal radiology. 2nd ed.p. 877. Baltimore: Williams and Wilkins;1996.5. Braun J, Bollow M, Sieper J. Radiologic diagnosis and pathology of the spondyloarthropathies. Rheum Dis Clin North Am. 1998; 24:697–735.
Article6. Jacobson JA, Girish G, Jiang Y, Resnick D. Radiographic evaluation of arthritis: inflammatory conditions. Radiology. 2008; 248:378–89.
Article7. Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009; 68:777–83.
Article8. Jee WH, McCauley TR, Lee SH, Kim SH, Im SA, Ha KY. Sacroiliitis in patients with ankylosing spondylitis: association of MR findings with disease activity. Magn Reson Imaging. 2004; 22:245–50.
Article9. Rudwaleit M, Jurik AG, Hermann KG, Landewé R, van der Heijde D, Baraliakos X, et al. Defining active sacroiliitis on magnetic resonance imaging (MRI) for classification of axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI group. Ann Rheum Dis. 2009; 68:1520–7.
Article10. Bredella MA, Steinbach LS, Morgan S, Ward M, Davis JC. MRI of the sacroiliac joints in patients with moderate to severe ankylosing spondylitis. AJR Am J Roentgenol. 2006; 187:1420–6.
Article11. Lacout A, Rousselin B, Pelage JP. CT and MRI of spine and sacroiliac involvement in spondyloarthropathy. AJR Am J Roentgenol. 2008; 191:1016–23.
Article12. Sieper J, Rudwaleit M, Baraliakos X, Brandt J, Braun J, Burgos-Vargas R, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis. 2009; 68(Suppl 2):ii1–44.
Article13. Jacobson JA, Girish G, Jiang Y, Sabb BJ. Radiographic evaluation of arthritis: degenerative joint disease and variations. Radiology. 2008; 248:737–47.
Article14. Kang HS, Hong SH, Chang HK. Musculoskeletal Radiology. 1st ed.p. 121. Seoul, Korea: Medicalplus;2013.15. Canella C, Schau B, Ribeiro E, Sbaffi B, Marchiori E. MRI in seronegative spondyloarthritis: imaging features and differential diagnosis in the spine and sacroiliac joints. AJR Am J Roentgenol. 2013; 200:149–57.
Article16. Olivieri I, Ferri S, Barozzi L. Osteitis condensans ilii. Br J Rheumatol. 1996; 35:295–7.17. Resnick D, Niwayama G. Osteoporosis. Resnick D, Niwayama G, editors. Diagnosis of bone and joint disorders. 3rd ed.p. 1839. Philadelphia: WB Saunders;1995.18. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988; 166:193–9.
Article19. Resnick D, Niwayama G. Ankylosing spondylitis. Resnick D, editor. Diagnosis of bone and joint disorders. 3rd ed.p. 1008. Philadelphia: WB Saunders;1995.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Piriformis syndrome as an overlooked cause of pain in a patient with axial spondyloarthritis: a case report
- Ewing's Sarcoma of the Sacroiliac Joint Presenting as Tubercular Sacroiliitis: A Diagnostic Dilemma
- Relief of Symptoms by Early Administration of Infliximab in Patients with Suspected Spondyloarthritis: A Case Report
- A Case of the Lumbar Spine Involvement and Sacroiliitis in a Patient with Gout
- Pyogenic Sacroiliac Joint Infection