Allergy Asthma Immunol Res.
2016 Sep;8(5):404-411. 10.4168/aair.2016.8.5.404.
Does Spore Count Matter in Fungal Allergy?: The Role of Allergenic Fungal Species
- Affiliations
-
- 1Department of Life Science, Tunghai University, Taichung, Taiwan. phwang@thu.edu.tw
- 2Division of Allergy, Immunology and Rheumatology, Taichung Veterans General Hospital, Taichung, Taiwan. ysanne@vghtc.gov.tw
- 3Faculty of Medicine, National Yang-Ming University, Taipei, Taiwan.
- 4Department of Medical Research, Taichung Veterans General Hospital, Taichung, Taiwan.
- 5The Environmental Analysis Laboratory, Taoyuan, Taiwan.
- KMID: 2295149
- DOI: http://doi.org/10.4168/aair.2016.8.5.404
Abstract
- PURPOSE
Fungi have been known to be important aeroallergens for hundreds of years. Most studies have focused on total fungal concentration; however, the concentration of specific allergenic fungi may be more important on an individual basis.
METHODS
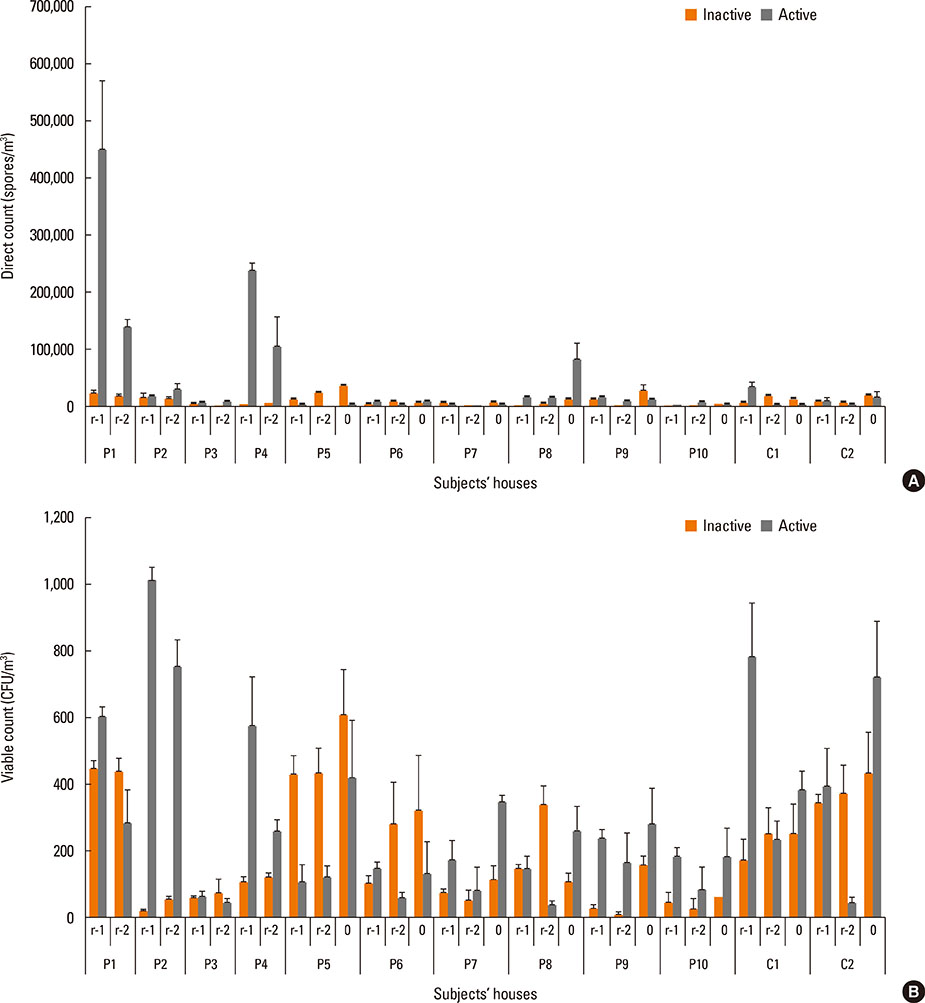
Ten fungal allergic patients and 2 non-fungal allergic patients were enrolled. The patients with a decrease in physician or patient global assessment by more than 50% of their personal best were considered to have an exacerbation of allergic symptoms and to be in the active stage. Those who maintained their physician and patient global assessment scores at their personal best for more than 3 months were considered to be in the inactive stage. The concentrations of dominant fungi in the patients' houses and outdoors were measured by direct and viable counts at active and inactive stages.
RESULTS
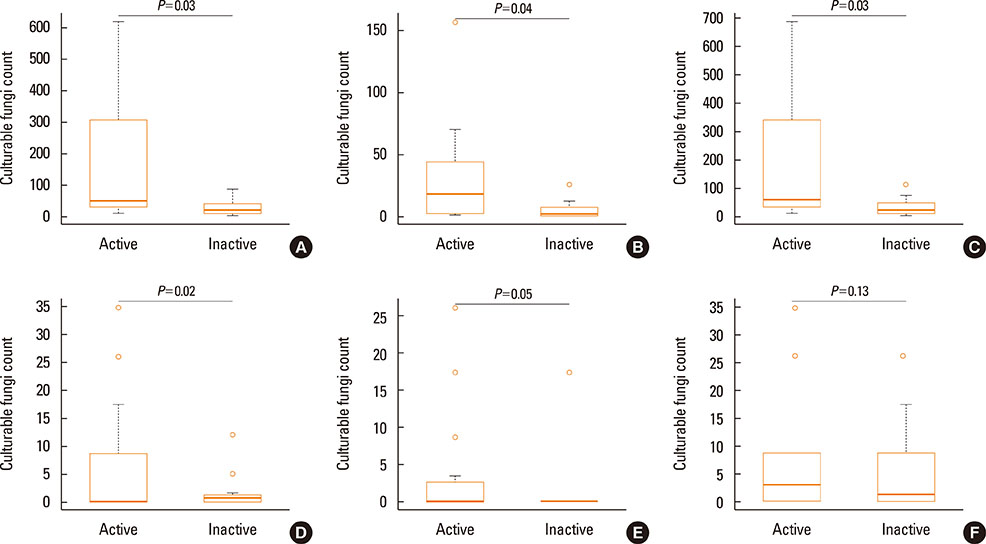
The exacerbation of allergic symptoms was not correlated with total fungal spore concentration or the indoor/outdoor ratio (I/O). Specific fungi, such as Cladosporium oxysporum (C. oxyspurum), C. cladosporioides, and Aspergillus niger (A. niger), were found to be significantly higher concentrations in the active stage than in the inactive stage. Presumed allergenic spore concentration threshold levels were 100 CFU/m3 for C. oxysporum, and 10 CFU/m3 for A. niger, Penicillium brevicompactum and Penicillium oxalicum.
CONCLUSIONS
The major factor causing exacerbation of allergic symptoms in established fungal allergic patients may be the spore concentration of specific allergenic fungi rather than the total fungal concentration. These results may be useful in making recommendations as regards environmental control for fungal allergic patients.
MeSH Terms
Figure
Cited by 2 articles
-
Can Controlling Endoplasmic Reticulum Dysfunction Treat Allergic Inflammation in Severe Asthma With Fungal Sensitization?
Jae Seok Jeong, So Ri Kim, Yong Chul Lee
Allergy Asthma Immunol Res. 2018;10(2):106-120. doi: 10.4168/aair.2018.10.2.106.Sputum Inflammatory Mediators Are Increased in
Aspergillus fumigatus Culture-Positive Asthmatics
Michael A Ghebre, Dhananjay Desai, Amisha Singapuri, Joanne Woods, Laura Rapley, Suzanne Cohen, Athula Herath, Andrew J Wardlaw, Catherine H Pashley, Richard May, Chris E Brightling
Allergy Asthma Immunol Res. 2017;9(2):177-181. doi: 10.4168/aair.2017.9.2.177.
Reference
-
1. Twaroch TE, Curin M, Valenta R, Swoboda I. Mold allergens in respiratory allergy: from structure to therapy. Allergy Asthma Immunol Res. 2015; 7:205–220.2. Tischer CG, Hohmann C, Thiering E, Herbarth O, Müller A, Henderson J, et al. Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy. 2011; 66:1570–1579.3. Tischer C, Chen CM, Heinrich J. Association between domestic mould and mould components, and asthma and allergy in children: a systematic review. Eur Respir J. 2011; 38:812–824.4. Pant H, Schembri MA, Wormald PJ, Macardle PJ. IgE-mediated fungal allergy in allergic fungal sinusitis. Laryngoscope. 2009; 119:1046–1052.5. Simon-Nobbe B, Denk U, Pöll V, Rid R, Breitenbach M. The spectrum of fungal allergy. Int Arch Allergy Immunol. 2008; 145:58–86.6. Orman A, Fiçici SE, Ay A, Ellidokuz H, Sivaci RG, Konuk M. Detection of fungi spectrum in industrial and home bakeries and determinated fungal allergy with skin prick test. Asian Pac J Allergy Immunol. 2005; 23:79–85.7. Zauli D, Grassi A, Vukatana G, Ballardini G, Bianchi FB. Allergy to fungal allergens in northern Italy. Ann Allergy Asthma Immunol. 2004; 92:92.8. Kanny G, Becker S, de Hauteclocque C, Moneret-Vautrin DA. Airborne eczema due to mould allergy. Contact Dermatitis. 1996; 35:378.9. Müller A, Lehmann I, Seiffart A, Diez U, Wetzig H, Borte M, et al. Increased incidence of allergic sensitisation and respiratory diseases due to mould exposure: results of the Leipzig Allergy Risk children Study (LARS). Int J Hyg Environ Health. 2002; 204:363–365.10. Denning DW, Pashley C, Hartl D, Wardlaw A, Godet C, Del Giacco S, et al. Fungal allergy in asthma-state of the art and research needs. Clin Transl Allergy. 2014; 4:14.11. Crameri R, Garbani M, Rhyner C, Huitema C. Fungi: the neglected allergenic sources. Allergy. 2014; 69:176–185.12. Ogawa H, Fujimura M, Ohkura N, Makimura K. Atopic cough and fungal allergy. J Thorac Dis. 2014; 6:S689–S698.13. Shin SH, Ye MK, Kim JK. Effects of fungi and eosinophils on mucin gene expression in rhinovirus-infected nasal epithelial cells. Allergy Asthma Immunol Res. 2014; 6:149–155.14. Bush RK, Portnoy JM, Saxon A, Terr AI, Wood RA. The medical effects of mold exposure. J Allergy Clin Immunol. 2006; 117:326–333.15. Chang FY, Lee JH, Yang YH, Yu HH, Wang LC, Lin YT, et al. Analysis of the serum levels of fungi-specific immunoglobulin E in patients with allergic diseases. Int Arch Allergy Immunol. 2011; 154:49–56.16. Beezhold DH, Green BJ, Blachere FM, Schmechel D, Weissman DN, Velickoff D, et al. Prevalence of allergic sensitization to indoor fungi in West Virginia. Allergy Asthma Proc. 2008; 29:29–34.17. Vijay HM, Kurup VP. Fungal allergens. Clin Allergy Immunol. 2008; 21:141–160.18. Zukiewicz-Sobczak WA. The role of fungi in allergic diseases. Postepy Dermatol Alergol. 2013; 30:42–45.19. Burge HA. Fungus allergens. Clin Rev Allergy. 1985; 3:319–329.20. Su HJ, Wu PC, Chen HL, Lee FC, Lin LL. Exposure assessment of indoor allergens, endotoxin, and airborne fungi for homes in southern Taiwan. Environ Res. 2001; 85:135–144.21. Tsai JJ, Chen WC. Different age of asthmatic patients affected by different aeroallergens. J Microbiol Immunol Infect. 1999; 32:283–288.22. Liang KL, Su MC, Jiang RS. Comparison of the skin test and ImmunoCAP system in the evaluation of mold allergy. J Chin Med Assoc. 2006; 69:3–6.23. Huang HW, Lue KH, Wong RH, Sun HL, Sheu JN, Lu KH. Distribution of allergens in children with different atopic disorders in central Taiwan. Acta Paediatr Taiwan. 2006; 47:127–134.24. Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ Health Perspect. 2011; 119:748–756.25. Doyle JJ, Doyle JL. Isolation of plant DNA from fresh tissue. Focus. 1990; 12:13–15.26. White TJ, Bruns T, Lee S, Taylor J. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In : Innis MA, Gelfand DA, Sninsky JJ, White TJ, editors. PCR protocols: a guide to methods and applications. San Diego (CA): Academic Press;1990. p. 315–322.27. Behbod B, Sordillo JE, Hoffman EB, Datta S, Muilenberg ML, Scott JA, et al. Wheeze in infancy: protection associated with yeasts in house dust contrasts with increased risk associated with yeasts in indoor air and other fungal taxa. Allergy. 2013; 68:1410–1418.28. Behbod B, Sordillo JE, Hoffman EB, Datta S, Webb TE, Kwan DL, et al. Asthma and allergy development: contrasting influences of yeasts and other fungal exposures. Clin Exp Allergy. 2015; 45:154–163.29. Chen C, Zhao B. Review of relationship between indoor and outdoor particles: I/O ratio, infiltration factor and penetration factor. Atmos Environ. 2011; 45:275–288.30. Şakiyan N, İnceoğlu Ö. Atmospheric concentrations of Cladosporium and Alternaria spores in Ankara and the effects of meterological factors. Turk J Bot. 2003; 27:77–81.31. Ross MA, Curtis L, Scheff PA, Hryhorczuk DO, Ramakrishnan V, Wadden RA, et al. Association of asthma symptoms and severity with indoor bioaerosols. Allergy. 2000; 55:705–711.32. Holme J, Hägerhed-Engman L, Mattsson J, Sundell J, Bornehag CG. Culturable mold in indoor air and its association with moisture-related problems and asthma and allergy among Swedish children. Indoor air. 2010; 20:329–340.33. Sharpe RA, Bearman N, Thornton CR, Husk K, Osborne NJ. Indoor fungal diversity and asthma: A meta-analysis and systematic review of risk factors. J Allergy Clin Immunol. 2015; 135:110–122.34. Kasprzyk I, Worek M. Airborne fungal spores in urban and rural environments in Poland. Aerobiologia. 2006; 22:169–176.35. O'Gorman CM, Fuller HT. Prevalence of culturable airborne spores of selected allergenic and pathogenic fungi in outdoor air. Atmos Environ. 2008; 42:4355–4368.36. Oliveira M, Ribeiro H, Delgado JL, Abreu I. The effects of meteorological factors on airborne fungal spore concentration in two areas differing in urbanisation level. Int J Biometeorol. 2009; 53:61–73.37. Chiang CH, Wu KM, Wu CP, Yan HC, Perng WC. Evaluation of risk factors for asthma in Taipei City. J Chin Med Assoc. 2005; 68:204–209.38. Green BJ, Tovey ER, Sercombe JK, Blachere FM, Beezhold DH, Schmechel D. Airborne fungal fragments and allergenicity. Med Mycol. 2006; 44:Suppl 1. S245–S255.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A survey of airborne fungal spores in Seoul, Korea
- Fungal Spores as Allergen
- Molecular Identification of Arbuscular Mycorrhizal Fungal Spores Collected in Korea
- A Case of 73-Year-Old Male with Chronic Invasive Fungal Sinusitis Mimicking Sino-Nasal Malignancy
- Clinical features of mold asthma sensitive to Alternaria spp