Korean J Urol.
2006 Aug;47(8):870-875. 10.4111/kju.2006.47.8.870.
The Relationship between Inflammation or Bacterial Infection according to the Traditional 4-glass Tests or Tc-99m Ciprofloxacin Imaging and the Scores of the National Institute of Health-Chronic Prostatitis Symptom Index in Men with Chronic Prostatitis
- Affiliations
-
- 1Department of Urology, Inha University College of Medicine, Incheon, Korea. jksuh@inha.ac.kr
- 2Department of Social and Preventive Medicine, Inha University College of Medicine, Incheon, Korea.
- 3Department of Laboratory Medicine, Inha University College of Medicine, Incheon, Korea.
- KMID: 2294117
- DOI: http://doi.org/10.4111/kju.2006.47.8.870
Abstract
-
PURPOSE: We wanted to determine whether inflammation and bacterial infection, as tested for by the traditional 4-glass test or Tc-99m ciprofloxacin imaging, correlate with the symptom severity in men with chronic prostatitis.
MATERIALS AND METHODS
The study included 256 patients with symptoms of prostatitis. The Korean version of the National Institute of Health Chronic Prostatitis Symptom Index (NIH-CPSI) was used to measure the symptoms of each patient. To diagnose bacterial infection, four-glass tests were performed that included culture for general bacteria, Mycoplasma hominis and Ureaplasma urealyticum, and polymerase chain reaction was performed for Chlamydia trachomatis. The patients with established uropathogens localized to the expressed prostatic secretion or the voided urine 3 were classified as having chronic bacterial prostatitis (CBP). To further localize the infection, the single photon emission computerized tomography images were obtained 3 hours after intravenous injection of Tc-99m ciprofloxacin. Associations between the symptoms and the inflammation and infection were evaluated.
RESULTS
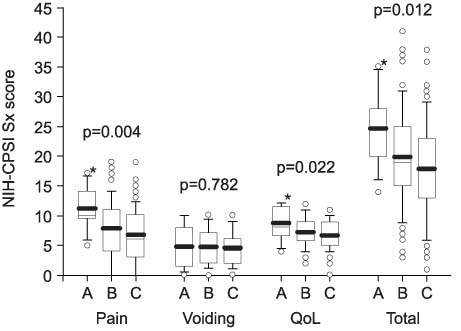
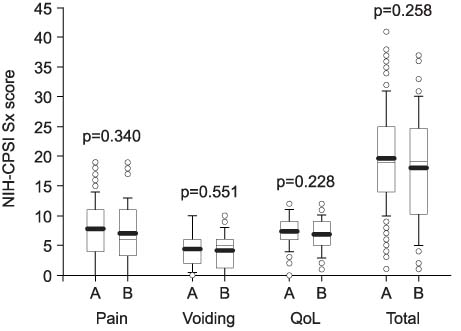
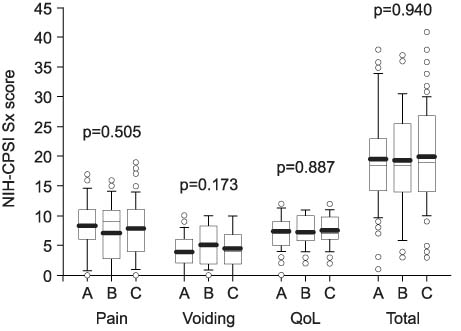
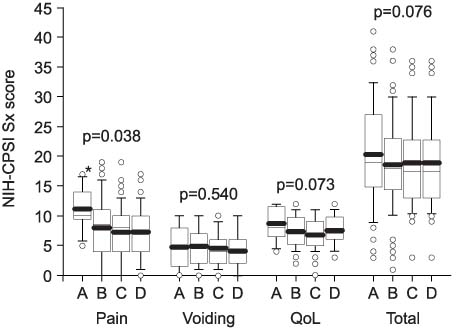
Based on the 4-glass tests, the patients were classified as CBP (n=16) or as chronic pelvis pain syndrome (CCPS) (the inflammatory type, n=94; non-inflammatory type, n=146). The CBP patients had a higher pain score than did the CPPS patients and there were no significant differences in the subscores for voiding symptoms and the quality of life between the groups. No significant differences were found in the total score or the subscores of the NIH-CPSI based on the presence or location of infection on the Tc-99m ciprofloxacin imaging.
CONCLUSIONS
These findings suggest that bacterial infection, not inflammation, as determined by traditional laboratory tests contribute to the symptoms, especially pain, in men with chronic prostatitis.
Keyword
MeSH Terms
-
Bacteria
Bacterial Infections*
Chlamydia trachomatis
Ciprofloxacin*
Humans
Inflammation*
Injections, Intravenous
Male
Mycoplasma hominis
Pelvic Pain
Pelvis
Polymerase Chain Reaction
Prostatitis*
Quality of Life
Surveys and Questionnaires
Radionuclide Imaging
Tomography, Emission-Computed, Single-Photon
Ureaplasma urealyticum
Ciprofloxacin
Figure
Reference
-
1. Lipsky BA. Urinary tract infections in men. Epidemiology, pathophysiology, diagnosis, and treatment. Ann Intern Med. 1989. 110:138–150.2. Litwin MS, McNaughton-Collins M, Fowler FJ Jr, Nickel JC, Calhoun EA, Pontari MA, et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. J Urol. 1999. 162:369–375.3. Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001. 165:842–845.4. Bowers JE, Thomas GB. The clinical significance of abnormal prostatic secretion. J Urol. 1958. 79:976–982.5. Jameson RM. Sexual activity and the variations of the white cell content of the prostatic secretion. Invest Urol. 1967. 5:297–302.6. Schaeffer AJ, Wendel EF, Dunn JK, Grayhack JT. Prevalence and significance of prostatic inflammation. J Urol. 1981. 125:215–219.7. Roberts RO, Lieber MM, Bostwick DG, Jacobsen SJ. A review of clinical and pathological prostatitis syndromes. Urology. 1997. 49:809–821.8. Schaeffer AJ, Knauss JS, Landis JR, Propert KJ, Alexander RB, Litwin MS, et al. Leukocyte and bacterial counts do not correlate with severity of symptoms in men with chronic prostatitis: the National Institutes of Health Chronic Prostatitis Cohort Study. J Urol. 2002. 168:1048–1053.9. Choe W, Chung MH, Kim WH, Kim S, Ryu JK, Kang KJ, et al. Imaging prostatitis with Tc-99m ciprofloxacin. Clin Nucl Med. 2002. 27:527–529.10. Choe W, Ryu JK, Kim WH, Chung MH, Suh JK. Imaging seminal vesiculitis with Tc-99m ciprofloxacin. Clin Nucl Med. 2003. 28:501–502.11. Lee SM, Ryu JK, Suh JK. Role of Tc-99m ciprofloxacin imaging in the diagnosis of bacterial prostatitis. Korean J Urol. 2003. 44:861–865.12. Ryu JK, Lee SM, Seong DW, Suh JK, Kim SG, Choe WS, et al. Tc-99m ciprofloxacin imaging in diagnosis of chronic bacterial prostatitis. Asian J Androl. 2003. 5:179–183.13. Hall AV, Solanki KK, Vinjamuri S, Britton KE, Das SS. Evaluation of the efficacy of 99mTc-Infecton, a novel agent for detecting sites of infection. J Clin Pathol. 1998. 51:215–219.14. Britton KE, Wareham DW, Das SS, Solanki KK, Amaral H, Bhatnagar A, et al. Imaging bacterial infection with 99mTc-ciprofloxacin (infecton). J Clin Pathol. 2002. 55:817–823.15. Meares EM, Stamey TA. Bacteriologic localization patterns in bacterial prostatitis and urethritis. Invest Urol. 1968. 5:492–518.16. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.17. Cho IR, Park SC, Park SS. The prevalence of the symptoms of the prostate syndrome patients under 50. Korean J Urol. 1998. 39:751–756.18. Krieger JN, Egan KJ, Ross SO, Jacobs R, Berger RE. Chronic pelvic pains represent the most prominent urogenital symptoms of "chronic prostatitis". Urology. 1996. 48:715–722.19. Alexander RB, Trissel D. Chronic prostatitis: results of an internet survey. Urology. 1996. 48:568–574.20. Hochreiter WW, Nadler RB, Koch AE, Campbell PL, Ludwig M, Weidner W, et al. Evaluation of the cytokines interleukin 8 and epithelial neutrophil activating peptide 78 as indicators of inflammation in prostatic secretions. Urology. 2000. 56:1025–1029.21. Schneider H, Wilbrandt K, Ludwig M, Beutel M, Weidner W. Prostate-related pain in patients with chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2004. 95:238–243.22. Schaeffer AJ, Datta NS, Fowler JE Jr, Krieger JN, Litwin MS, Nadler RB, et al. Overview summary statement. Diagnosis and management of chronic prostatitis/chronic pelvic pain syndrome. Urology. 2002. 60:6 Suppl. 1–4.23. Takahashi S, Riley DE, Krieger JN. Application of real-time polymerase chain reaction technology to detect prostatic bacteria in patients with chronic prostatitis/chronic pelvic pain syndrome. World J Urol. 2003. 21:100–104.24. Krieger JN, Riley DE. Bacteria in the chronic prostatitis-chronic pelvic pain syndrome: molecular approaches to critical research questions. J Urol. 2002. 167:2574–2583.25. Riley DE, Berger RE, Miner DC, Krieger JN. Diverse and related 16S rRNA-encoding DNA sequences in prostate tissues of men with chronic prostatitis. J Clin Microbiol. 1998. 36:1646–1652.26. Badalyan RR, Fanarjyan SV, Aghajanyan IG. Chlamydial and ureaplasmal infections in patients with nonbacterial chronic prostatitis. Andrologia. 2003. 35:263–265.27. Britton KE, Wareham DW, Das SS. Concerns about 99mTc-labelled ciprofloxacin for infection detection. Eur J Nucl Med. 2001. 28:779–781.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Tc-99m Ciprofloxacin Imaging in the Diagnosis of Bacterial Prostatitis
- Comparison of the Efficacy of Transperineal Intraprostatic Injection and Oral Administration of Fluoroquinolone in Men with Chronic Bacterial Prostatitis-Seminal Vesiculitis
- Chronic Bacterial Prostatitis
- The Concentrations of Zinc in Expressed Prostatic Secretion of Chronic Prostatitis Patients
- Chronic Prostatitis: A Possible Cause of Hematospermia