J Korean Ophthalmol Soc.
2016 Jun;57(6):1012-1017. 10.3341/jkos.2016.57.6.1012.
Bilateral Simultaneous Central Retinal Vein Occlusion in a Patient with Waldenstrom's Macroglobulinemia
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea. ocularimmunity@gmail.com
- KMID: 2290508
- DOI: http://doi.org/10.3341/jkos.2016.57.6.1012
Abstract
- PURPOSE
The authors report a case of bilateral simultaneous central retinal vein occlusion caused by Waldenstrom's macroglobulinemia.
CASE SUMMARY
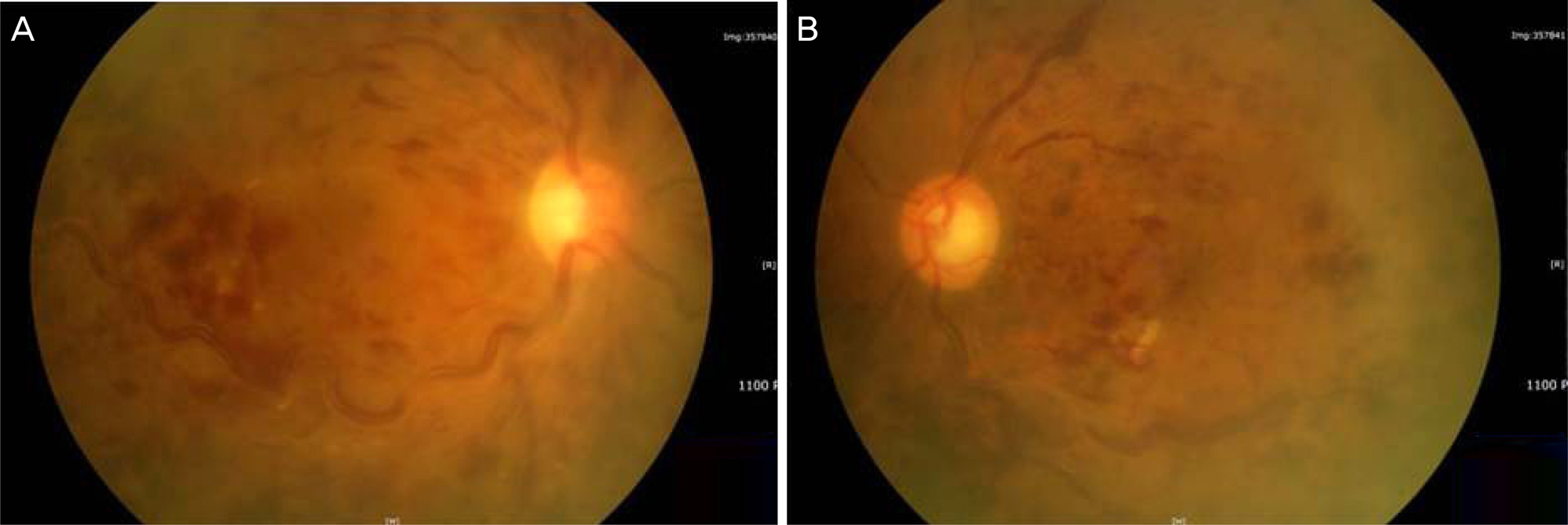
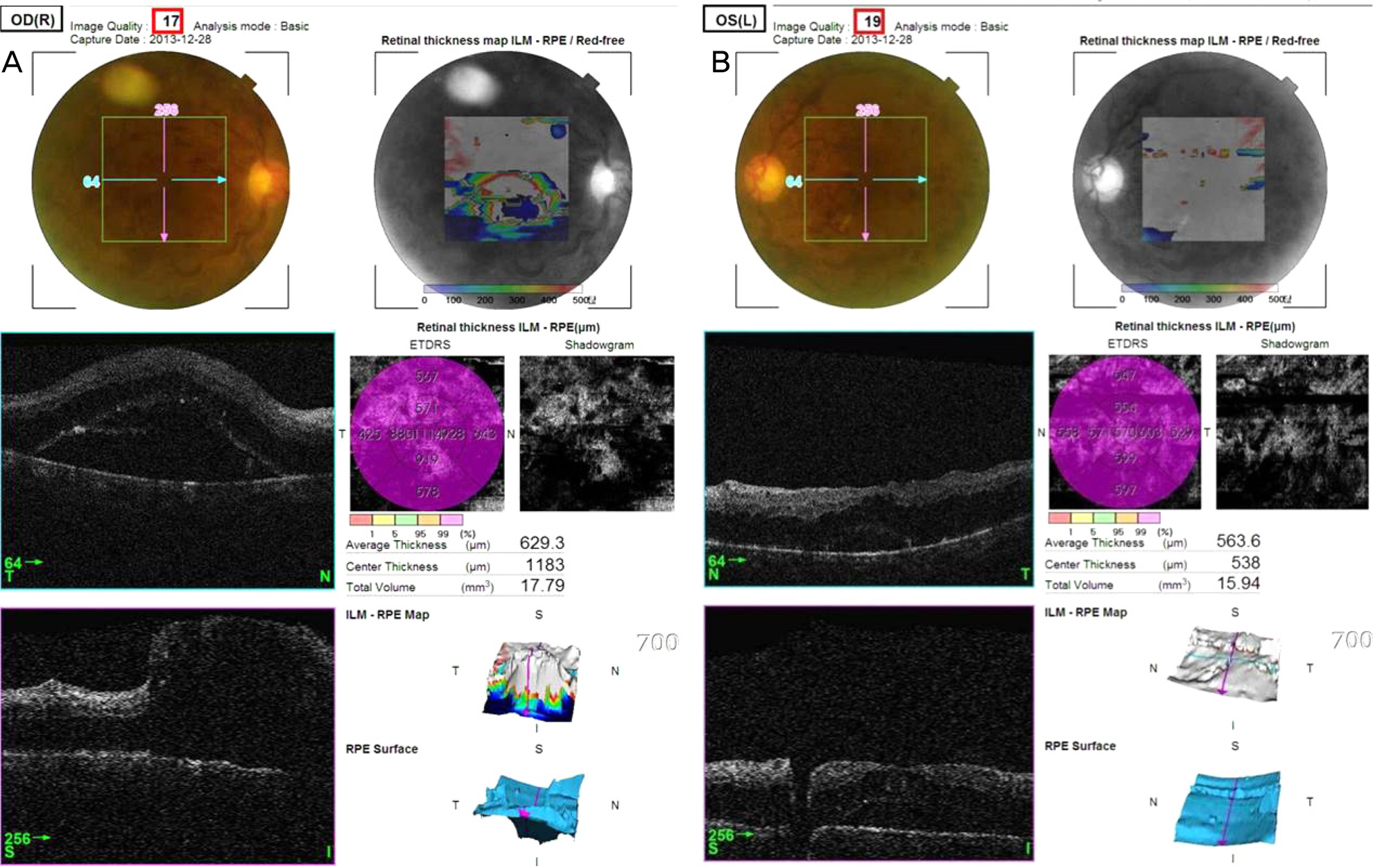
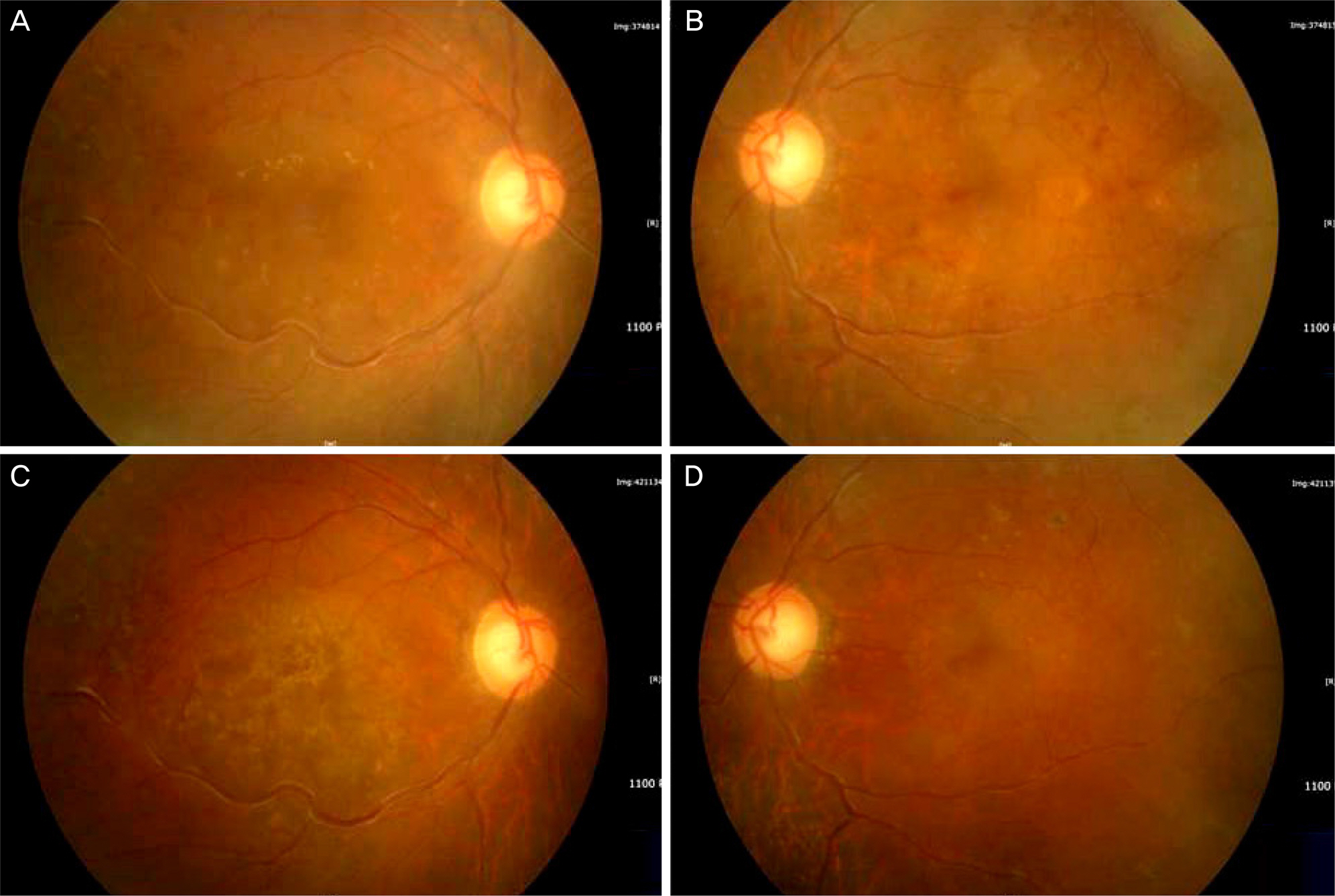
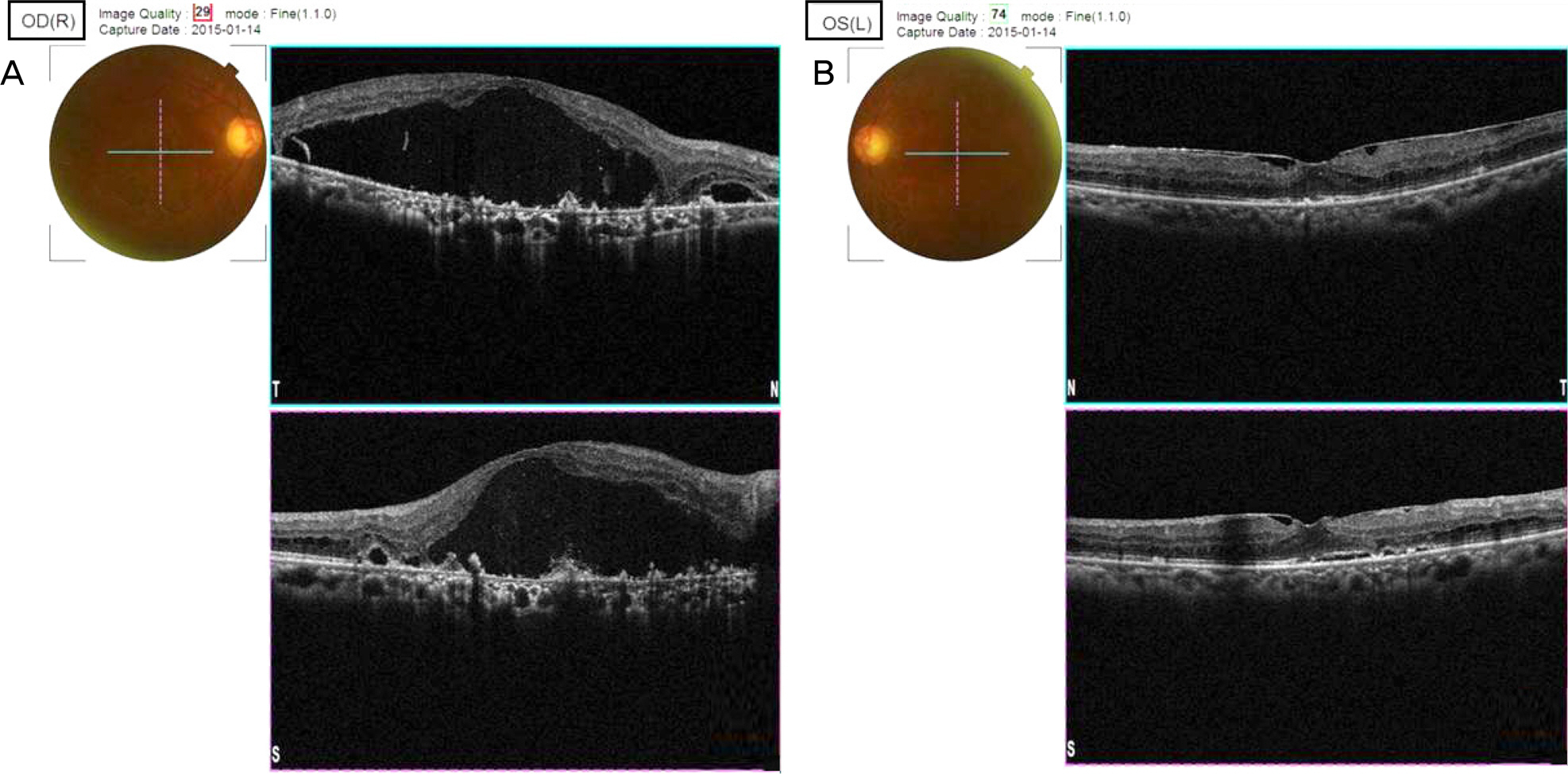
A 65-year-old man presented to our department complaining of decreased visual acuity for the duration of about 6 months. On his initial visit, best-corrected visual acuity was 0.02 in the right eye and 0.06 in the left eye. Based on the findings of a funduscopic examination, the patient had bilateral diffuse retinal hemorrhages, dilated tortuous veins, and macular edema. He had experienced recurrent spontaneous epistaxis 6 months previously and had undergone treatments such as intravitreal bevacizumab injection and intravitreal dexamethasone implantation at another hospital. Laboratory tests at that hospital showed anemia and hyperproteinemia, for which he was referred to our hemato-oncology department. Bone marrow biopsy was consistent with Waldenstrom's macroglobulinemia/lymphoplasmacytoid lymphoma, and he was treated with systemic chemotherapy. One year after the systemic chemotherapy, his best-corrected visual acuity was 0.15 in the right eye and 0.6 in the left eye. Funduscopy showed decreased bilateral retinal hemorrhages and macular edema.
CONCLUSIONS
When simultaneous bilateral central retinal vein occlusion occurs in a patient with no other underlying disease such as hypertension or diabetes, it might be a sign of serum hyperviscosity, and there should be a very high level of suspicion for presence or progression of systemic disease. If such a disease is properly and timely diagnosed, effective early systemic evaluation and therapy can be administered, and it is important to have initial general treatment as well as ophthalmic treatment.
MeSH Terms
Figure
Reference
-
References
1. Lahey JM, Tunç M, Kearney J, et al. Laboratory evaluation of abdominal states in patients with central retinal vein occlusion who are less than 56 years of age. Ophthalmology. 2002; 109:126–31.2. Prisco D, Marcucci R. Retinal vein thrombosis: risk factors, abdominal and therapeutic approach. Pathophysiol Haemost Thromb. 2002; 32:308–11.3. Mehta J, Singhal S. Hyperviscosity syndrome in plasma cell dyscrasias. Semin Thromb Hemost. 2003; 29:467–71.
Article4. Jung KI, Yum HR, Kim IT. Bilateral central retinal vein occlusion in patient with disseminated intravascular coagulation. J Korean Ophthalmol Soc. 2011; 52:1005–8.
Article5. Gertz MA. Waldenström macroglobulinemia: a review of therapy. Am J Hematol. 2005; 79:147–57.
Article6. Waldenström J. Incipient myelomatosis or «essential« hyper-globulinemia with fibrinogenopenia – a new syndrome? Acta Medica Scandinavica. 1944; 117:216–47.7. Casares PZ, Gillet DS, Verity DH, Rowson NR. Bilateral abdominal central retinal vein occlusion (CRVO) caused by waldenstrom's macroglobulinaemia with acquired von willebrand's disease. Br J Haematol. 2002; 118:344–7.8. Alexander P, Flanagan D, Reqe K, et al. Bilateral simultaneous central retinal vein occlusion secondary to hyperviscosity in abdominal's macroglobulinaemia. Eye (Lond). 2008; 22:1089–92.9. Lee YH, Lee JY, Kim YS, et al. Successful anticoagulation for abdominal central retinal vein occlusions accompanied by cerebral abdominal thrombosis. Arch Neurol. 2006; 63:1648–51.10. Baker PS, Garg SJ, Fineman MS, et al. Serous macular detachment in Waldenström macroglobulinemia: a report of four cases. Am J Ophthalmol. 2013; 155:448–55.
Article11. Caimi A, Giani A, Bottoni F, Staurenghi G. Serous macular abdominal in Waldenström macroglobulinemia: a report of 4 cases. Am J Ophthalmol. 2013; 155:955–6.12. Fenicia V, Balestrieri M, Perdicchi A, et al. Intravitreal injection of dexamethasone implant in serous macular detachment associated with Waldenström's disease. Case Rep Ophthalmol. 2013; 4:64–9.
Article13. Besirli CG, Johnson MW. Immunogammopathy maculopathy abdominal with Waldenström macroglobulinemia is refractory to conventional interventions for macular edema. Retin Cases Brief Rep. 2013; 7:319–24.14. Menke MN, Feke GT, McMeel JW, Treon SP. Effect of plasmapheresis on hyperviscosity-related retinopathy and retinal hemodynamics in patients with Waldenstrom's macroglobulinemia. Invest Ophthalmol Vis Sci. 2008; 49:1157–60.
Article15. Ratanam M, Ngim YS, Khalidin N, Subrayan V. Intravitreal abdominal: a viable treatment for bilateral central retinal vein abdominal with serous macular detachment secondary to Waldenström macroglobulinaemia. Br J Haematol. 2015; 170:431–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Waldenström Macroglobulinemia Induced Bilateral Central Retinal Vein Occlusion with Refractory Macular Edema Treated with Systemic Chemotherapy: Case Report
- Hyperviscosity Syndrome-related Retinopathy in a Patient with Waldenström Macroglobulinemia
- Diffuse Large B-cell Lymphoma in Waldenstrom Macroglobulinemia
- A Case of Cilioretinal Artery Occlusion Associated with Central Retinal Vein Occlusion
- Clinical observation of the bilateral branch vein occlusion