J Korean Ophthalmol Soc.
2016 Jun;57(6):1004-1011. 10.3341/jkos.2016.57.6.1004.
Systemic Steroid Therapy for Serous Retinal Detachment Caused by Excessive Endolaser during Diabetic Retinopathy Surgery
- Affiliations
-
- 1Department of Ophthalmology, Konyang University College of Medicine, Daejeon, Korea. Astrix001@gmail.com
- KMID: 2290507
- DOI: http://doi.org/10.3341/jkos.2016.57.6.1004
Abstract
- PURPOSE
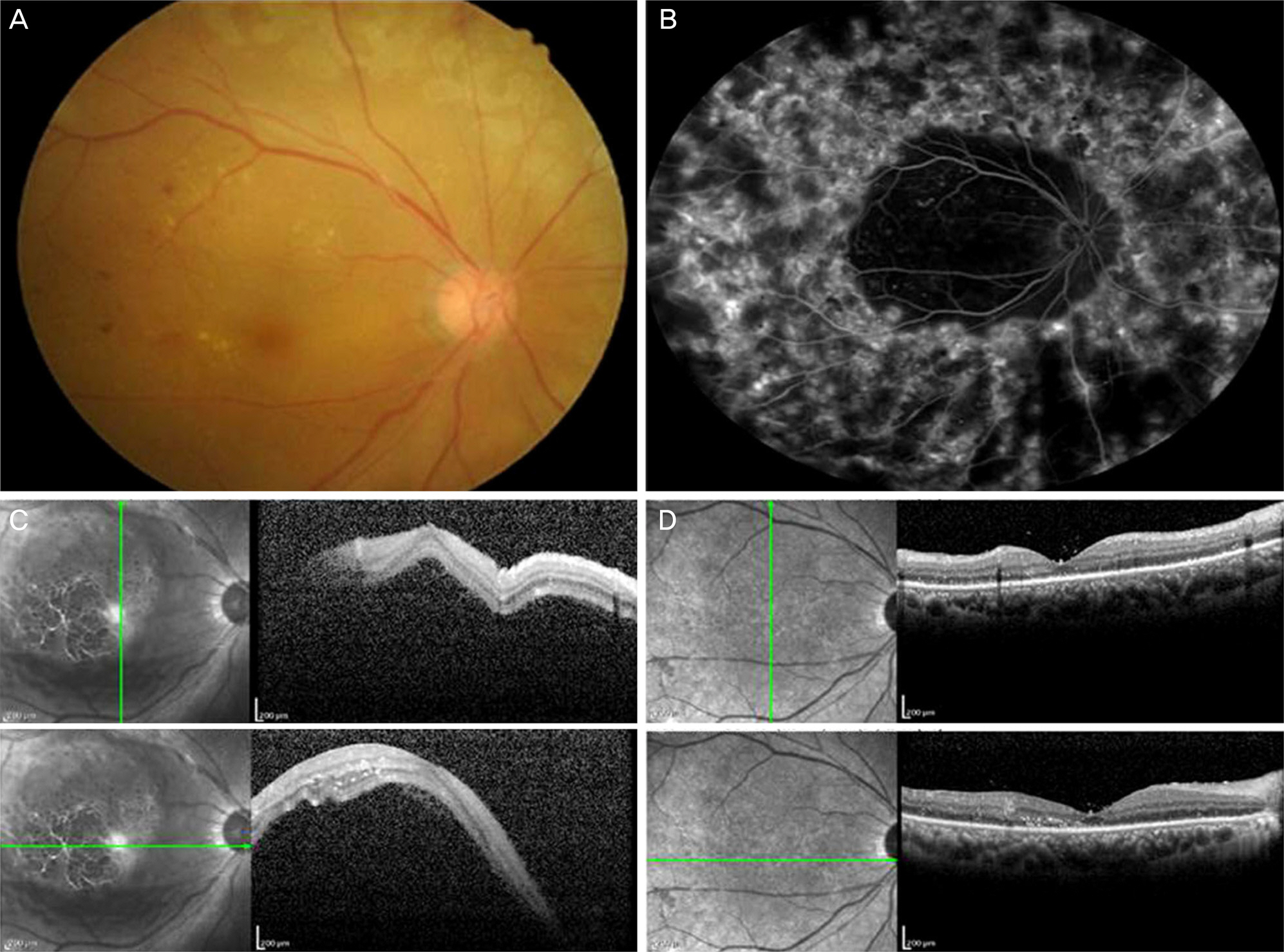
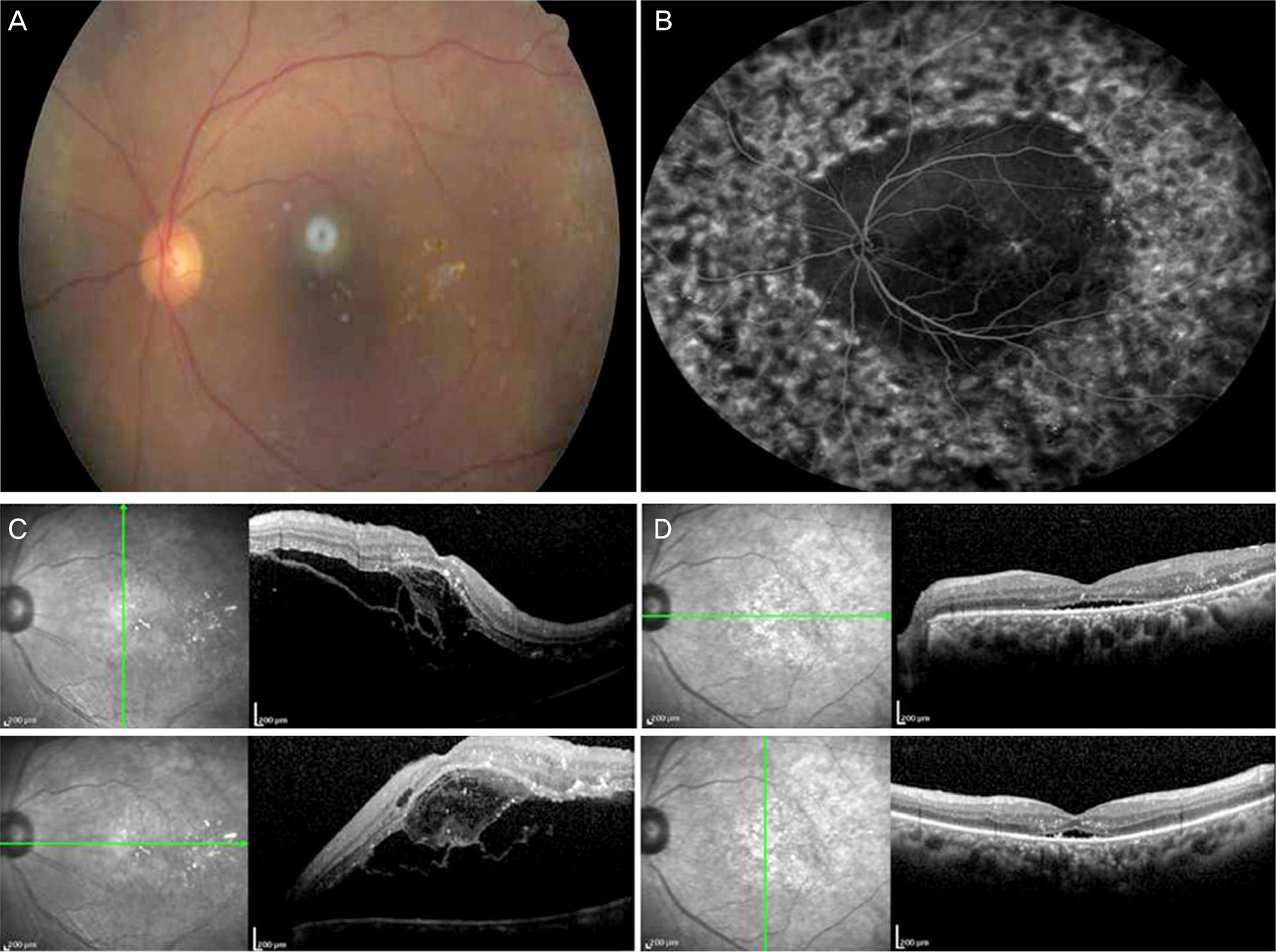
To report cases of macular serous retinal detachment caused by excessive intraoperative endolaser in patients with diabetic vitreous hemorrhage. Macular serous retinal detachment was improved by systemic steroid therapy.
CASE SUMMARY
A 64-year-old male (case 1) and a 67-year-old female (case 2) treated with vitrectomy and endolaser (case 1, 3,184 shots; case 2, 1,734 shots) because of diabetic vitreous hemorrhage visited our out-patient clinic with blurred vision. Best corrected visual acuity (BCVA) in case 1 was hand motion and 0.03 in case 2. Fundus examination and optical coherence tomography (OCT) revealed extensive subretinal fluid accumulation of the posterior pole. With the diagnosis of macular serous retinal detachment caused by excessive intraoperative endoaser, oral steroid (40 mg/qd, 5 days) was administered and then later reduced in case 1. In case 2, we administered intravenous high-dose steroid (250 mg/qid, 3 days). After systemic steroid therapy, BCVA was improved to 20/30 in case 1 and 20/40 in case 2 and OCT showed the subretinal fluid was resolved.
CONCLUSIONS
During diabetic retinopathy surgery, excessive endolaser induced macular serous retinal detachment and systemic steroid therapy was necessary in diabetic patients. Thus, physicians should be well acquainted with this complication.
MeSH Terms
Figure
Cited by 1 articles
-
Two Cases of Serous Retinal Detachment Following Vitrectomy in Patients with Proliferative Diabetic Retinopathy
Jang-Hun Lee, Sa Kang Kim, Sang Beom Han, Seung Jun Lee, Moo Sang Kim
J Korean Ophthalmol Soc. 2017;58(1):98-105. doi: 10.3341/jkos.2017.58.1.98.
Reference
-
References
1. Soubrane G, Coscas G. Pathogenesis of seroud retinal detachment of the retina and pigment epithelium. Stephen JR, editor. Retina. 5th ed.Amsterdam: Amsterdam;2013. 1:chap. 30.2. Kim PS, Choi CW, Yang YS. Outcome and significance of silicone oil tamponade in patients with chronic serous retinal detachment. Korean J Ophthalmol. 2014; 28:26–31.
Article3. Akduman L, Del Priore LV, Kaplan HJ. Spontaneous resolution of retinal detachment occurring after macular hole surgery. Arch Ophthalmol. 1998; 116:465–7.
Article4. Campochiaro PA, Jerdon JA, Glaser BM. The extracellular matrix of human retinal pigment epithelial cells in vivo and its synthesis in vitro. Invest Ophthalmol Vis Sci. 1986; 27:1615–21.5. Negi A, Marmor MF. Experimental serous retinal detachment and focal pigment epithelial damage. Arch Ophthalmol. 1984; 102:445–9.
Article6. Van Buskirk EM, Lessell S, Friedman E. Pigmentary epitheliopathy and erythema nodosum. Arch Ophthalmol. 1971; 85:369–72.
Article7. Marmor MF. New hypotheses on the pathogenesis and treatment of serous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 1988; 226:548–52.
Article8. Messmer EP, Ruggli GH, Apple DJ, Naumann GOH. Special abdominal of the retina. Naumann GOH, editor. special pathologic anatomy. 2nd ed.Berlin: Berlin;1997. chap. 11.9. Aggarwal BB, Puri RK. Human Cytokines: Their Role in Disease and Therapy. United Kingdom: Blackwell science;1995. p. 3–26.10. Aydin A, Cakir A, Unal MH, Ersanli D. Central serous retinal abdominal following glaucoma filtration surgery. J Fr Ophtalmol. 2012; 35:529.e1–5.11. Buyukyildiz HZ, Gulkilik G, Kumcuoglu YZ. Early serous abdominal detachment after phacoemulsification surgery. J Cataract Refract Surg. 2010; 36:1999–2002.12. Nishina S, Suzuki Y, Azuma N. Exudative retinal detachment abdominal cataract surgery in Hallermann-Streiff syndrome. Graefes Arch Clin Exp Ophthalmol. 2008; 246:453–5.13. Kontos A, Mitry D, Althauser S, Jain S. Acute serous macular abdominal and cystoid macular edema after uncomplicated abdominal using standard dose subconjunctival cefuroxime. Cutan Ocul Toxicol. 2014; 33:233–4.14. Gribomont AC. Precocious exudative retinal detachment after abdominal of the macular hole. Bull Soc Belge Ophtalmol. 1997; 267:77–9.15. Gamulescu MA, Roider J, Gabel VP. Exudative retinal detachment in macular hole surgery using platelet concentrates-a case report. Graefes Arch Clin Exp Ophthalmol. 2001; 239:227–9.16. Liggett PE, Lean JS, Barlow WE, Ryan SJ. Intraoperative argon endophotocoagulation for recurrent vitreous hemorrhage after abdominal for diabetic retinopathy. Am J Ophthalmol. 1987; 103:146–9.17. Flynn HW Jr, Chew EY, Simons BD, et al. Pars plana vitrectomy in the Early Treatment Diabetic Retinopathy Study. ETDRS report number 17. The Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1992; 99:1351–7.18. Stenkula S. Photocoagulation in diabetic retinopathy. A abdominal study in Sweden. Acta Ophthalmol Suppl. 1984; 162:1–100.19. Pautler S. Treatment of proliferative diabetic retinopathy. Browning D, editor. Diabetic Retinopathy: Evidence Based Management. 1st ed.New York: New York;2010. chap. 8.
Article20. Little HL. Complications of argon laser retinal photocoagulation: a five-year study. Int Ophthalmol Clin. 1976; 16:145–59.
Article21. Georges A, Benjamin W, Pierr-Loic C, et al. Serous retinal abdominal following panretinal photocoagulation (PRP) using Pattern Scan Laser (PASCAL) photocoagulator. GMS Ophthalmol Cases. 2012; 2:Doc01.22. Doft BH, Blankenship GW. Single versus multiple treatment sessions of argon laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1982; 89:772–9.
Article23. DellaCroce J, Laursen J, Ayyala RS. Serous retinal detachment abdominal glaucoma surgery. Ophthalmic Surg Lasers Imaging. 2007; 38:503–4.24. Roy AK, Padhy D. Serous retinal detachment after trabeculectomy in angle recession glaucoma. GMS Ophthalmol Cases. 2015; 5:Doc15.25. Krishnan R, Hiscott P, Kumar I, Heimann H. Delayed exudative subfoveal retinal detachment following successful macular hole surgery. Jpn J Ophthalmol. 2008; 52:140–2.
Article26. Poon YC, Chen CH, Kuo HK, et al. Clinical implications of serous retinal detachment in branch retinal vein occlusion and response after primary intravitreal bevacizumab injection. J Ocul Pharmacol Ther. 2013; 29:319–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Serous Retinal Detachment Following Vitrectomy in Patients with Proliferative Diabetic Retinopathy
- The Prophylactic Effect of 360 Degree Endolaser Photocoagulation for Prevention of Retinal Detachment
- A Case of Purtscher's Retinopathy with Diffuse Serous Macular Detachment
- Delayed Onset Purtscher's Retinopathy with Serous Retinal Detachment after Trauma in a Retinitis Pigmentosa
- Secondary Giant Retinal Cyst