J Clin Neurol.
2005 Apr;1(1):50-58. 10.3988/jcn.2005.1.1.50.
Non-cardioembolic Mechanisms in Cryptogenic Stroke: Clinical and Diffusion-weighted Imaging Features
- Affiliations
-
- 1Department of Neurology, Ajou University School of Medicine, Suwon, Korea. nmboy@unitel.co.kr
- KMID: 2287713
- DOI: http://doi.org/10.3988/jcn.2005.1.1.50
Abstract
- BACKGROUND
The role of several cardiogenic risk factors, including patent foramen ovale, in patients with cryptogenic stroke has been extensively studied. However, little attention has been paid to the role of non-cardioembolic causes of cryptogenic stroke. We therefore sought to identify the characteristics of cryptogenic stroke.
METHODS
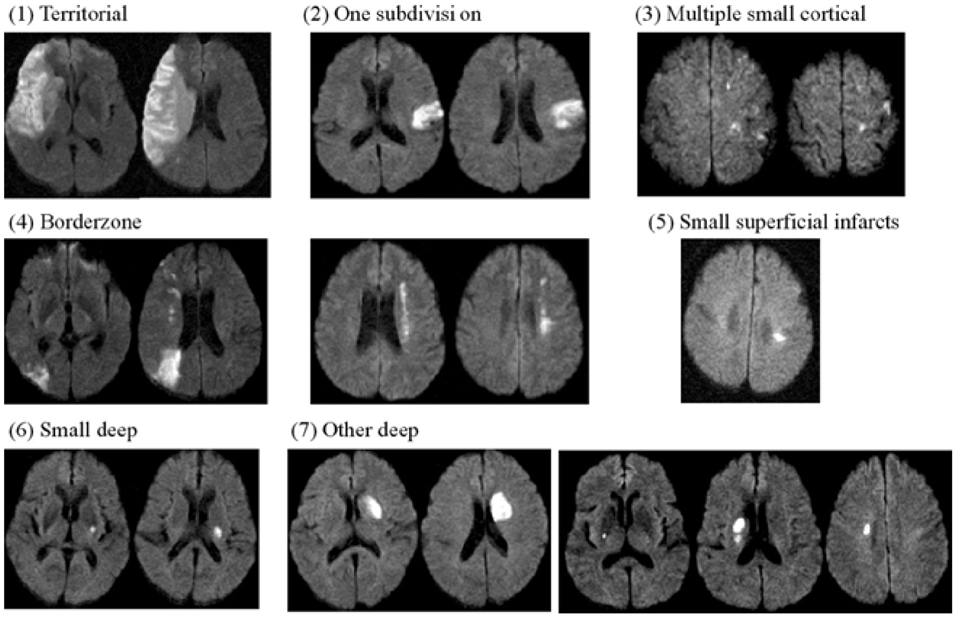
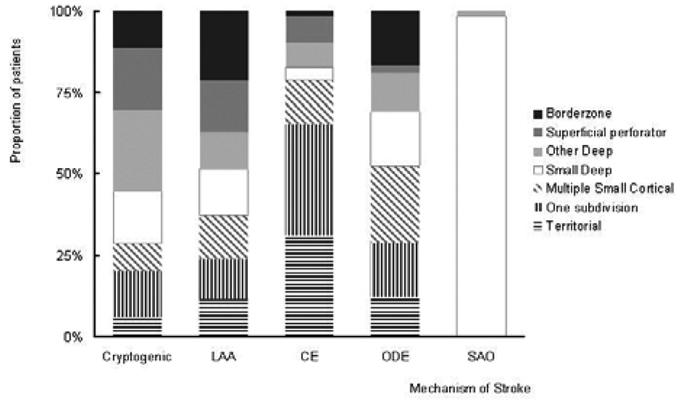
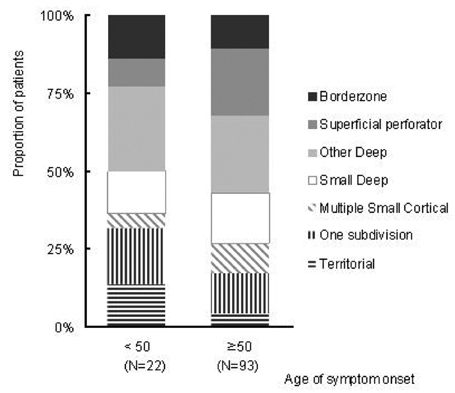
We studied 832 patients with acute infarction in the middle cerebral arterial territory. We divided the patients into four subtypes: 402 with large artery atherosclerosis (LAA), 133 with cardioembolism, 182 with small arterial occlusion (SAO), and 115 with cryptogenic stroke. We compared risk factors and lesion patterns observed by diffusion-weighted imaging (DWI) between patients with cryptogenic stroke and those with stroke of other subtypes.
RESULTS
Both risk factors and DWI lesion patterns differed between the cryptogenic and cardioembolic groups (P<0.05). Risk factors for cryptogenic stroke were similar to those for the LAA and SAO groups. Similarly, DWI lesion patterns for cryptogenic stroke were similar to LAA patients. Large cortical infarcts on DWI were more common in the cardioembolic group than in the LAA or cryptogenic groups (P<0.001). In contrast, deep, non-lacunar (OR 5.02; 95% CI 2.68~9.40; P<0.001) and superficial perforator infarcts (OR 2.23; 95% CI 1.08~4.59; P=0.029) were independently associated with the cryptogenic group.
CONCLUSIONS
Our results indicate that non-cardioembolic causes, such as macro- and microangiopathy, are important mechanisms in the pathogenesis of cryptogenic stroke.
Keyword
MeSH Terms
Figure
Reference
-
1. Sacco RL, Ellenberg JH, Mohr JP, Tatemichi TK, Hier DB, Price TR, et al. Infarcts of undetermined cause: the NINCDS Stroke Data Bank. Ann Neurol. 1989. 25:382–390.
Article2. Baird AE, Lovblad KO, Schlaug G, Edelman RR, Warach S. Multiple acute stroke syndrome: marker of embolic disease? Neurology. 2000. 54:674–678.
Article3. Gandolfo C, Del Sette M, Finocchi C, Calautti C, Loeb C. Internal borderzone infarction in patients with ischemic stroke. Cerebrovasc Dis. 1998. 8:255–258.
Article4. Lee PH, Bang OY, Oh SH, Joo IS, Huh K. Subcortical white matter infarcts: comparison of superficial perforating artery and internal border-zone infarcts using diffusion-weighted magnetic resonance imaging. Stroke. 2003. 34:2630–2635.5. Kang DW, Chalela JA, Ezzeddine MA, Warach S. Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol. 2003. 60:1730–1734.
Article6. Paciaroni M, Silvestrelli G, Caso V, Corea F, Venti M, Milia P, et al. Neurovascular territory involved in different etiological subtypes of ischemic stroke in the Perugia Stroke Registry. Eur J Neurol. 2003. 10:361–365.
Article7. Bang OY, Lee PH, Joo SY, Lee JS, Joo IS, Huh K. Frequency and mechanisms of stroke recurrence after cryptogenic stroke. Ann Neurol. 2003. 54:227–234.
Article8. Heinsius T, Bogousslavsky J, Van Melle G. Large infarcts in the middle cerebral artery territory. Etiology and outcome patterns. Neurology. 1998. 50:341–350.
Article9. Ageno W, Finazzi S, Steidl L, Biotti MG, Mera V, Melzi D'Eril G, et al. Plasma measurement of D-dimer levels for the early diagnosis of ischemic stroke subtypes. Arch Intern Med. 2002. 162:2589–2593.
Article10. Ince B, Bayram C, Harmanci H, Ulutin T. Hemostatic markers in ischemic stroke of undetermined etiology. Thromb Res. 1999. 96:169–174.
Article11. Lamy C, Giannesini C, Zuber M, Arquizan C, Meder JF, Trystram D, et al. Clinical and imaging findings in cryptogenic stroke patients with and without patent foramen ovale: the PFO-ASA Study. Atrial Septal Aneurysm. Stroke. 2002. 33:706–711.
Article12. Mas JL, Arquizan C, Lamy C, Zuber M, Cabanes L, Derumeaux G, et al. Patent Foramen Ovale and Atrial Septal Aneurysm Study Group. Recurrent cerebrovascular events associated with patent foramen ovale, atrial septal aneurysm, or both. N Engl J Med. 2001. 345:1740–1746.
Article13. Hart RG, Pearce LA, Rothbart RM, McAnulty JH, Asinger RW, Halperin JL. Stroke with intermittent atrial fibrillation: incidence and predictors during aspirin therapy. Stroke Prevention in Atrial Fibrillation Investigators. J Am Coll Cardiol. 2000. 35:183–187.
Article14. Amarenco P, Cohen A, Tzourio C, Bertrand B, Hommel M, Besson G, et al. Atherosclerotic disease of the aortic arch and the risk of ischemic stroke. N Engl J Med. 1994. 331:1474–1479.
Article15. Konstadt SN, Louie EK, Black S, Rao TL, Scanlon P. Intraoperative detection of patent foramen ovale by transesophageal echocardiography. Anesthesiology. 1991. 74:212–216.
Article16. Homma S, Sacco RL, Di Tullio MR, Sciacca RR, Mohr JP. PFO in Cryptogenic Stroke Study (PICSS) Investigators. Effect of medical treatment in stroke patients with patent foramen ovale: patent foramen ovale in Cryptogenic Stroke Study. Circulation. 2002. 105:2625–2631.
Article17. Rauh R, Fischereder M, Spengel FA. Transesophageal echocardiography in patients with focal cerebral ischemia of unknown cause. Stroke. 1996. 27:691–694.
Article18. Schaer BA, Zellweger MJ, Cron TA, Kaiser CA, Osswald S. Value of routine holter monitoring for the detection of paroxysmal atrial fibrillation in patients with cerebral ischemic events. Stroke. 2004. 35:e68–e70.
Article19. Cabanes L, Mas JL, Cohen A, Amarenco P, Cabanes PA, Oubary P, et al. Atrial septal aneurysm and patent foramen ovale as risk factors for cryptogenic stroke in patients less than 55 years of age. A study using transesophageal echocardiography. Stroke. 1993. 24:1865–1873.
Article20. Steiner MM, Di Tullio MR, Rundek T, Gan R, Chen X, Liguori C, et al. Patent foramen ovale size and embolic brain imaging findings among patients with ischemic stroke. Stroke. 1998. 29:944–948.
Article21. Barinagarrementeria F, Amaya LE, Cantu C. Causes and mechanisms of cerebellar infarction in young patients. Stroke. 1997. 28:2400–2404.
Article22. Nedeltchev K, Arnold M, Wahl A, Sturzenegger M, Vella EE, Windecker S, et al. Outcome of patients with cryptogenic stroke and patent foramen ovale. J Neurol Neurosurg Psychiatry. 2002. 72:347–350.
Article23. Rodriguez CJ, Homma S, Sacco RL, Di Tullio MR, Sciacca RR, Mohr JP. PICSS Investigators. Race-ethnic differences in patent foramen ovale, atrial septal aneurysm, and right atrial anatomy among ischemic stroke patients. Stroke. 2003. 34:2097–2102.
Article24. Kizer JR, Silvestry FE, Kimmel SE, Kasner SE, Wiegers SE, Erwin MB, et al. Racial differences in the prevalence of cardiac sources of embolism in subjects with unexplained stroke or transient ischemic attack evaluated by transesophageal echocardiography. Am J Cardiol. 2002. 90:395–400.
Article25. Gupta V, Nanda NC, Yesilbursa D, Huang WY, Gupta V, Li Q, et al. Racial differences in thoracic aorta atherosclerosis among ischemic stroke patients. Stroke. 2003. 34:408–412.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Applications of diffusion-weighted imaging in diagnosis, evaluation, and treatment of acute ischemic stroke
- Transient global amnesia associated with multiple lesions in the corpus callosum and hippocampus
- Availability of Classification of Lacunar Syndrome and Diffusion-weighed MR Imaging in Lacunar Stroke
- Comparison of Diffusion-weighted and T2-weighted Magnetic Resonance Imaging for Ischemic Stroke
- RE: Diffusion-Weighted Imaging of Prostate Cancer: How Can We Use It Accurately?