J Clin Neurol.
2005 Apr;1(1):14-30. 10.3988/jcn.2005.1.1.14.
New England Medical Center Posterior Circulation Stroke Registry: I. Methods, Data Base, Distribution of Brain Lesions, Stroke Mechanisms, and Outcomes
- Affiliations
-
- 1Cerebrovascular Disease Sections of the New England Medical Center, Boston and the Beth Israel Deaconess Medical Center, Boston. lcaplan@bidmc.harvard.edu
- KMID: 2287711
- DOI: http://doi.org/10.3988/jcn.2005.1.1.14
Abstract
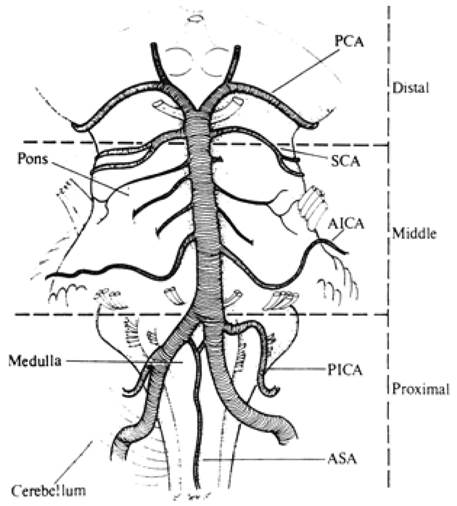
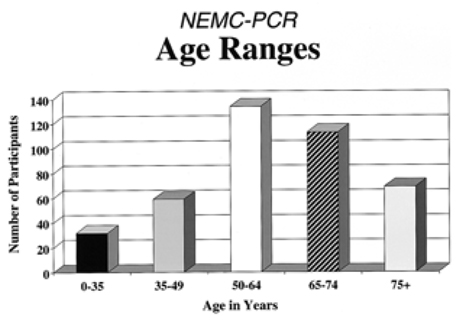
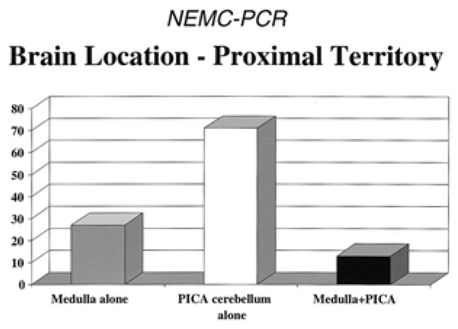
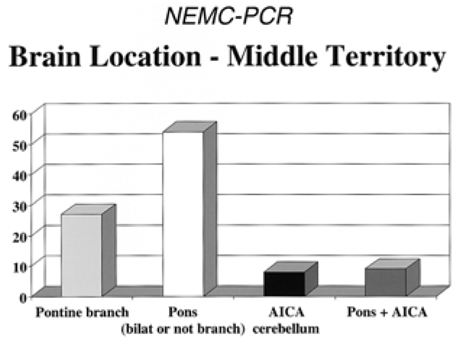
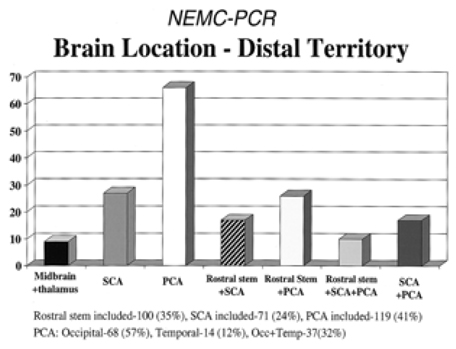
- Among 407 New England Medical Center Posterior Circulation Registry (NEMC-PCR) patients, 59% had strokes without transient ischemic attacks (TIAs), 24% had TIAs before strokes, and 16% had only posterior circulation TIAs. Embolism was the commonest stroke mechanism accounting for 40% of cases (24% cardiac origin, 14% arterial origin, 2% had potential cardiac and arterial sources). In 32%, large artery occlusive lesions caused hemodynamic brain infarction. Stroke mechanisms in the posterior and anterior circulation are very similar. Infarcts most often included the distal posterior circulation territory (rostral brainstem, superior cerebellum and occipital and temporal lobes), while the proximal (medulla and posterior inferior cerebellum) and middle (pons and anterior inferior cerebellum) territories were equally involved. Infarcts that included the distal territory were twice as common as those that included the proximal or middle territories. Most distal territory infarcts were attributable to embolism. Thirty day mortality was low (3.6%). Embolic stroke mechanism, distal territory location, and basilar artery occlusive disease conveyed the worst prognosis.
MeSH Terms
Figure
Cited by 2 articles
-
A Review of Endovascular Treatment for Posterior Circulation Strokes
Sung Hyun Baik, Jun Yup Kim, Cheolkyu Jung
Neurointervention. 2023;18(2):90-106. doi: 10.5469/neuroint.2023.00213.Rescue Endovascular Treatment to Prevent Neurological Deterioration in Acute Symptomatic Bilateral Vertebral Artery Occlusion
Byoung Wook Hwang, Min A Lee, Sang Woo Ha, Jae Ho Kim, Hak Sung Kim, Seong Hwan Ahn
Neurointervention. 2023;18(3):182-189. doi: 10.5469/neuroint.2023.00381.
Reference
-
1. Barnett HJM. A modern approach to posterior circulation ischemic stroke. Arch Neurol. 2002. 59:359–360.
Article2. Caplan LR. Posterior circulation disease: clinical features, diagnosis, and management. 1996. Boston: Blackwell Science.3. Caplan LR. Posterior circulation ischemia: then, now, and tomorrow. The Thomas Willis Lecture 2000. Stroke. 2000. 31:2011–2023.
Article4. Glass TA, Hennessey PM, Pazdera L, Chang H-M, Wityk RJ, DeWitt LD, et al. Outcome at 30 days in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2002. 59:369–376.
Article5. Caplan LR, Wityk RJ, Glass TA. The New England Medical Center Posterior Circulation Registry. Ann Neurol. 2004. 56:389–398.6. Georgiadis AI, Yamamoto Y, Kwan ES, Pessin MS, Caplan LR. Anatomy of sensory findings in patients with Posterior Cerebral Artery Territory Infarction. Arch Neurol. 1999. 56:835–838.
Article7. Graf KJ, Pessin MS, DeWitt LD, Caplan LR. Proximal intracranial territory posterior circulation infarcts in the New England Medical Center Posterior Circulation Registry. Eur Neurol. 1997. 37:157–168.
Article8. Muller-Kuppers M, Graf KJ, Pessin MS, DeWitt LD, Caplan LR. Intracranial vertebral artery disease in the New England Medical Center Posterior Circulation Registry. Eur Neurol. 1997. 37:146–156.
Article9. Shin H-K, Yoo K-M, Chang H-M, Caplan LR. Bilateral intracranial vertebral artery disease in the New England medical Center Posterior Circulation Registry. Arch Neurol. 1999. 56:1353–1358.
Article10. Wityk RJ, Chang H-M, Rosengart A, Han W-C, DeWitt LD, Pessin MS, Caplan LR. Proximal extracranial vertebral artery disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 1998. 55:470–478.
Article11. Yamamoto Y, Georgiadis AI, Chang H-M, Caplan LR. Posterior Cerebral Artery territory Infarcts in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 1999. 56:824–832.
Article12. Benedikt M. Tremblement avec paralysie croisee du moteur oculaire commun. Bull Med Paris. 1889. 3:547–548.13. Claude H. Syndrome pedonculaire de la region du noyau rouge. Rev Neurol. 1912. 23:311–313.14. Claude H, Levy-Valensi J. Maladies des pedoncules cerebraux in Maladies du cervelet et de l'isthme de l'encephale (pedoncule, protuberance, bulbe). 1922. Paris: Bailliere;184–211.15. Babinski J, Nageotte J. Hemiasynergie, lateropulsion et myosis bulbaires avec hemianesthesie et hemiplegie croisees. Rev Neurol. 1902. 10:358–365.16. Foville A. Note sur une paralysie peu connue de certains muscles de l'oeil. Bull Soc Anat Paris. 1858. 3:393–405.17. Wallenberg A. Anatomischer befund in einern als akute bulbaraffection (Embolie der arteria cerebelli inferior posterior sinistra) bescriebenen falle. Arch fur Psychiatrie. 1901. 34:923–959.
Article18. Wallenberg A. Verschluss der arteria cerebelli inferior posterior dextra (mit Sektion befund). Deutsche Zeitschrift fur Nervenheilkunde. 1922. 73:189–212.
Article19. Weber H. A contribution to the pathology of the crura cerebri. Medico Chirurg Trans. 1863. 46:121–139.
Article20. Wolfe JK. The classical brainstem syndromes. 1971. Springfield, Illinois: Charles C Thomas Publ.21. Liu GT, Crenner CW, Logoigian EL, Charness ME, Samuels MA. Midbrain syndromes of Benedikt, Claude, and Nothnagel. Setting the record straight. Neurology. 1992. 42:1820–1822.
Article22. Dejerine J. Serniologie des affections du systeme nerveux. 1926. Paris: Masson et cie.23. Foix C, Hillemand P, Schalit 1. Sur le syndrome lateral du bulbe et irrigation du bulbe superieur. Rev Neurol. 1925. 41:160–179.24. Dana CL. Acute bulbar paralysis due to hemorrhage and softening of the pons and medulla with reports of cases and autopsies. Medical Record. 1903. 64:361–374.25. Kubik CS, Adams RD. Occlusion of the basilar artery a clinical and pathological study. Brain. 1946. 69:73–121.
Article26. Dejerine J, Roussy G. Le syndrome thalamique. Rev Neurol. 1906. 14:521–532.27. Foix C, Hillemand P. Les arteres de I'axe encephalique jusqu'au diencephale inclusivement. Rev Neurol. 1925. 41:705–739.28. Foix C, Hillemand P. Les syndromes de la region thalamique. Presse Med. 1925. 33:113–117.29. Foix C, Masson A. Le syndrome de l'artere cerebrale posterieure. Presse Med. 31923. 31:361–365.30. Duret H. Sur la distribution des arteres nourricieres du bulbe rachidien. Arch Physiol Norm Pathol. 1873. 2:97–113.31. Duret H. Reserches anatomiques sur la circulation de 1'encephale. Arch Physiol Norm Pathol. 1874. 3:6091316–353. 664–693. 919–957.32. Foix C, Hillemand P. Contribution a 1'etude des ramollissements protuberantiels. Rev Med. 1926. 43:287–305.33. Stopford JSB. The arteries of the pons and medulla oblongata. J Anat Physiol (London). 1916. 50:131–164. 225–280.34. Foix C, Hillemand P, Ley J. Relativement au ramollissement cerebral a sa frequence et a son siege et a l'importance relative des obliterations arterielles, completes ou incompletes dans sa pathogenie. Rev Neurol. 1927. 43:217–218.35. Fisher CM. Occlusion of the internal carotid artery. Arch Neurol Psychiatr. 1951. 65:346–377.
Article36. Fisher CM. Occlusion of the internal carotid arteries: further experiences. Arch Neurol Psychiat. 1954. 72:187–204.37. Hutchinson EC, Yates PO. The cervical portion of the vertebral artery: clincopathological study. Brain. 1956. 79:319–331.
Article38. Hutchinson EC, Yates PO. Caroticovertebral stenosis. Lancet. 1957. 1:28.39. Bradshaw P, McQuaid P. The syndrome of vertebrobasilar insufficiency. Quarterly J Med. 1963. 32:279–296.40. Williams D. Vertebrobasilar ischaemia. Brit Med J. 1964. 1:84–86.
Article41. Williams D, Wilson TG. The diagnosis of the major and minor syndromes of basilar insufficiency. Brain. 1962. 85:741–774.
Article42. DennyBrown D. Basilar artery syndromes. Bull N Engl Med Center. 1953. 15:53–60.43. Fang HC, Palmer JL. Vascular phenomena involving brainstern structures: a clinical and pathological correlation study. Neurology. 1956. 6:402–419.
Article44. Millikan CH, Siekert RG. Studies in cerebrovascular disease; I The syndrome of intermittent insufficiency of the basilar arterial system. Proc Staff Meet Mayo Clin. 1955. 30:61–68.45. Millikan CH, Siekert RG, Shick R. Studies in cerebrovascular disease. 3. The use of anticoagulant drugs in the treatment of insufficiency or thrombosis within the basilar arterial system. Proc Staff Meet Mayo Clin. 1955. 30:111–126.46. Fisher CM. The use of anticoagulants in cerebral thrombosis. Neurology. 1958. 8:311–332.
Article47. Millikan CH, Siekert RG, Whisnant JP. Anticoagulant therapy in cerebrovascular disease: current status. JAMA. 1958. 166:587–592.
Article48. Rosengart A, DeWitt LD, Caplan LR, et al. Noninvasive tests in vertebrobasilar occlusive disease. Ann Neurol. 1992. 32:265.49. Bogousslavsky J, Regli F, Maeder P, Meuli R, Nader J. The etiology of posterior circulation infarcts: a prospective study using magnetic resonance angiography. Neurology. 1993. 43:1528–1533.
Article50. Wentz KU, Rother J, Schwartz A. Intracranial vertebrobasilar system: MR angiography. Radiology. 1994. 190:105–110.
Article51. Fisher CM. Pure sensory stroke involving face, arm, and leg. Neurology. 1965. 15:76–80.
Article52. Fisher CM. A lacunar stroke: the dysarthria clumsy hand syndrome. Neurology. 1967. 17:614–617.
Article53. Fisher CM. Ataxic hemiparesis. Arch Neurol. 1978. 35:126–128.
Article54. Fisher CM. Thalamic pure sensory stroke: a pathological study. Neurology. 1978. 28:1141–1144.55. Mohr JP. Lacunes. Stroke. 1982. 13:311.
Article56. Caplan LR. lntracranial branch atheromatous disease; a neglected, understudied, and underused concept. Neurology. 1989. 39:1246–1250.
Article57. Fisher CM, Caplan LR. Basilar artery branch occlusion: a cause of pontine infarction. Neurology. 1971. 21:900–905.
Article58. Fisher CM. Bilateral occlusion of basilar artery branches. J Neurol Neurosurg Psychiatry. 1977. 40:1182–1189.
Article59. Hauw JJ, Der Agopian P, Trelles L, Escourolle R. Bulbar infarcts. Systematic study of lesion topography in 49 cases. J Neurol Sci. 1976. 28:83–102.60. Escourolle R, Hauw JJ, Agopian PD, Trelles L. Bulbar infarcts. Vascular lesions in 26 observations. J Neurol Sci. 1976. 28:103–113.61. Fisher CM, Karnes W, Kubik CS. Lateral medullary infarction. The pattern of vascular occlusion. J Neuropath Exp Neurol. 1961. 20:323–379.62. Sypert GW, Alvord EC. Cerebellar infarction: a clinicopathological study. Arch Neurol. 1975. 32:357–363.63. Amarenco P. Bogousslavsky J, Caplan LR, editors. Cerebellar stroke syndromes. Stroke syndromes. 2001. 2nd edition. Cambridge University Press;540–556.
Article64. Amarenco P, Caplan LR. Vertebrobasilar occlusive disease: review of selected aspects. 3. Mechanisms of cerebellar infarctions. Cerebrovasc Dis. 1993. 3:66–73.
Article65. Amarenco P, Hauw JJ. Cerebellar infarction in the territory of the anterior and inferior cerebellar artery. Brain. 1990. 113:139–155.
Article66. Amarenco P, Hauw JJ. Cerebellar infarction in the territory of the superior cerebellar artery: a clinicopathologic study of 33 cases. Neurology. 1990. 40:1383–1390.
Article67. Amarenco P, Hauw JJ, Henin D, et al. Les infarctus du territoire de artere cerebelleuse posteroinferieure, etude clinicopathologique de 28 cas. Rev Neurol. 1989. 145:277–286.68. Amarenco P, Hauw JJ, Gautier JC. Arterial pathology in cerebellar infarction. Stroke. 1990. 21:1299–1305.
Article69. Amarenco P, Levy C, Cohen A, et al. Causes and mechanisms of territorial and nonterritorial cerebellar infarcts in 115 consecutive patients. Stroke. 1994. 25:105–112.
Article70. Amarenco P, Rosengart A, DeWitt LD, Pessin MS, Caplan LR. Anterior inferior cerebellar artery territory infarcts. Mechanisms and clinical features. Arch Neurol. 1993. 50:154–161.
Article71. Castaigne P, Lhermitte F, Buge A, Escourolle R, Hauw JJ, Lyon-Caen D. Paramedian thalamic and midbrain infarcts: clinical and neuropathological study. Ann Neurol. 1981. 10:127–148.
Article72. Caplan LR. The 1991 E Graeme Robertson lecture: Vertebrobasilar embolism. Clin Exp Neurol. 1991. 28:123.73. Caplan LR. Caplan LR, Hurst JW, Chimowitz M, editors. Brain embolism. Clinical Neurocardiology. 1999. New York: Marcel Decker;35–185.
Article74. Caplan LR, Tettenborn B. Vertebrobasilar occlusive disease: review of selected aspects. 2: Posterior circulation embolism. Cerebrovasc Dis. 1992. 2:320–326.
Article75. Caplan LR, Amarenco P, Rosengart A, Lafranchise EF, Teal PA, Belkin M, et al. Embolism from vertebral artery origin occlusive disease. Neurology. 1992. 42:1505–1512.
Article76. Caplan LR, Tettenborn B. Vertebrobasilar occlusive disease: review of selected aspects. 1. Spontaneous dissection of extracranial and intracranial posterior circulation arteries. Cerebrovasc Dis. 1992. 2:256–265.
Article77. Caplan LR, Zarins C, Hemmatti M. Spontaneous dissection of the extracranial vertebral artery. Stroke. 1985. 16:1030–1038.
Article78. Caplan LR, Baquis G, Pessin MS, D'Alton J, Adelman LS, DeWitt LD, et al. Dissection of the intracranial vertebral artery. Neurology. 1988. 38:867–877.
Article79. Mas JL, Bousser MG, Hasboun D, Laplane D. Extracranial vertebral artery dissection. A review of 13 cases. Stroke. 1987. 18:1037–1047.
Article80. Mokri B, Houser OW, Sandok BA, Piepgras DG. Spontaneous dissections of the vertebral arteries. Neurology. 1988. 38:880–885.
Article81. Moseley IP, Holland IM. Ectasia of the basilar artery: the breadth of the clinical spectrum and the diagnostic value of computed tomography. Neuroradiolgy. 1979. 18:83–91.
Article82. Nishizaki T, Tamaki N, Takeda N, et al. Dolichoectatic basilar artery: a review of 23 cases. Stroke. 1986. 17:1277–1281.
Article83. Pessin MS, Chimowitz MI, Levine SR, Kwan ES, Adelman LS, Earnest MP, et al. Stroke in patients with fusiform vertebrobasilar aneurysms. Neurology. 1989. 39:16–21.
Article84. Schwartz A, Rautenberg W, Hennerici M. Dolichoectatic intracranial arteries: review of selected aspects. Cerebrovasc Dis. 1993. 3:273–279.
Article85. Caplan LR. Top of the basilar syndrome: selected clinical aspects. Neurology. 1980. 30:72–79.86. Mehler MF. The rostral basilar artery syndrome: diagnosis, etiology, prognosis. Neurology. 1989. 39:916.
Article87. Pessin MS, Kwan ES, DeWitt LD, Gale D, Caplan LR. Posterior cerebral artery stenosis. Ann Neurol. 1987. 21:85–89.
Article88. Pessin MS, Lathi E, Cohen MB, Kwan ES, Hedges TR 3rd, Caplan LR. Clinical features and mechanisms of occipital infarction in the posterior cerebral artery territory. Ann Neurol. 1987. 21:290–299.89. Mohr JP, Caplan LR, Melski JW. The Harvard Cooperative Stroke Registry: a prospective registry. Neurology. 1978. 28:754–762.
Article90. Caplan LR, Hier DB, D'Cruz 1. Cerebral embolism in the Michael Reese Stroke Registry. Stroke. 1983. 14:530–536.
Article91. Foulkes MA, Wolf PA, Price TR, et al. The Stroke Data Bank: design, methods, and baseline data. Stroke. 1988. 19:547–554.
Article92. Bogousslavsky J, Van Melle G, Regli F. The Lausanne Stroke Registry: analysis of 1000 consecutive patients with first stroke. Stroke. 1988. 19:1083–1092.
Article93. Bogousslavsky J, Cachin C, Regli F, Despland P-A, Van Melle G, Kappenberger L. Lausanne Stroke registry Group. Cardiac sources of embolism and cerebral infarction- clinical consequences and vascular concomitants: the Lausanne Stroke Registry. Neurology. 1991. 41:855–859.
Article94. Moulin T, Tatu L, Crepin-Leblond T, Chavot D, Berges S, Rumbach L. The Besancon Stroke Registry: an acute stroke registry of 2500 consecutive patients. Eur Neurol. 1997. 38:10–20.
Article95. Vemmos K, Takis C, Georgilis K, Zakopoulos N, Lekakis J, Papamichael CM, et al. The Athens Stroke Registry: results of a five-year hospital-based study. Cerebrovasc Dis. 2000. 10:133–141.
Article96. Kittner SJ, Sharkness CM, Price TR, et al. Infarcts with a cardiac source of embolism in the NINCDS Stroke Data Bank; historical features. Neurology. 1990. 40:281–284.
Article97. Caplan LR. Clinical diagnosis of brain embolism. Cerebrovasc Dis. 1995. 5:79–88.98. Caplan LR, Hennerici M. Hypothesis: Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol. 1998. 55:1475–1482.
Article99. Kunitz S, Gross CR, Heyman A, Kase CS, Mohr JP, Price TR, et al. The Pilot Stroke Data Bank: definition, design, and data. Stroke. 1984. 15:740–746.
Article100. Moulin T, Tatu L, Vuillier F, Berger E, Chavot D, Rumbach L. Role of a stroke data bank in evaluating cerebral infarction subtypes: patterns and outcome of 1776 consecutive patients from the Besancon Stroke Registry. Cerebrovasc Dis. 2000. 10:261–271.
Article101. Vemmos K, Bots M, Tsibouris P, Zis V, Grobbee D, Stranjalis G, et al. Stroke incidence and case fatality in Southern Greece. The Arcadia Stroke Registry. Stroke. 1999. 30:363–370.
Article102. Grau AJ, Weimar C, Buggle F, Heinrich A, Goertler M, Neumaier S, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German Stroke Data Bank. Stroke. 2001. 32:2559–2566.
Article103. Publications Committee for the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) investigators. Low molecular weight heparinoid, ORG 10172 (danaparoid), and outcome after acute ischemic stroke. A randomized controlled trial. JAMA. 1998. 279:1265–1272.104. Libman RB, Kwiatkowski TG, Hansen MD, Clarke WR, Woolson RF, Adams HP. Differences between anterior and posterior circulation stroke in TOAST. Cerebrovasc Dis. 2001. 11:311–316.
Article105. Boyajian RA, Schwend RB, Wolfe MM, Bickerton RE, Otis SM. Measurement of anterior and posterior circulation flow contributions to cerebral blood flow. J Neuroimag. 1995. 5:1–3.
Article106. Hornig CR, Buttner T, Hoffman O, Dorndorf W. Short term prognosis of Vertebrobasilar ischemic stroke. Cerebrovasc Dis. 1992. 2:273–281.
Article107. Archer C, Horenstein S. Basilar artery occlusion: clinical and radiologic correlation. Stroke. 1977. 8:383–390.
Article108. Hacke W, Zeumer H, Ferbert A, Bruckmann H, del Zoppo G. Intraarterial therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988. 19:1216–1222.
Article109. Petty GW, Brown RD, Whisnant JP, Sicks JD, O'Falon WM, Wiebers DO. Ischemic stroke subtypes. A population-based study of functional outcome, survival, and recurrence. Stroke. 2000. 31:1062–1068.110. Broderick JP, Phillips SJ, O'Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1992. 23:1250–1256.111. Nadeau S, Jordan J, Mishra S. Clinical presentation as a guide to early prognosis in vertebrobasilar stroke. Stroke. 1992. 23:165–170.
Article112. Bernasconi A, Bogousslavsky J, Bassetti C, Regli F. Multiple acute infarcts in the posterior circulation. J Neurology Neurosurg Psychiatry. 1996. 60:289–296.
Article113. Wijdicks EF, Nichols DA, Thielen KR, Fulgham JR, Brown RD, Meissner I, et al. Intra-arterial thrombolysis in acute basilar artery thromboembolism: the initial Mayo Clinic experience. Mayo Clin Proc. 1997. 72:1005–1013.
Article114. Brandt T, von Kummer R, Muller-Kuppers M, Hacke W. Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke. 1996. 27:875–881.
Article115. Caplan LR. Caplan's Stroke, a clinical approach. 2000. 3rd ed. Boston: ButterworthHeinemann.116. Chambers BR, Donnan GA, Bladin PF. Patterns of stroke. An analysis of the first 700 consecutive admissions to the Austin Hospital stroke unit. Aust NZ J Med. 1983. 13–64.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New England Medical Center Posterior Circulation Stroke Registry II. Vascular Lesions
- Resurrection of Endovascular Thrombectomy for Posterior Circulation Stroke
- Posterior Circulation Stroke: Advances in Understanding and Management
- Collateral Circulation in Ischemic Stroke: An Updated Review
- Functional Outcome of Patients with Posterior Circulation Stroke