J Clin Neurol.
2014 Oct;10(4):354-357. 10.3988/jcn.2014.10.4.354.
Fulminant Subacute Sclerosing Panencephalitis Presenting with Acute Ataxia and Hemiparesis in a 15-Year-Old Boy
- Affiliations
-
- 1Department of Neurology, Nizam's Institute of Medical Sciences, Hyderabad, India. rukminimridula@gmail.com
- 2Department of Pathology, Nizam's Institute of Medical Sciences, Hyderabad, India.
- 3Department of Neurology, Medical College Hospital, Trivandrum, Kerala, India.
- KMID: 2287516
- DOI: http://doi.org/10.3988/jcn.2014.10.4.354
Abstract
- BACKGROUND
Subacute sclerosing panencephalitis (SSPE) is a delayed and fatal manifestation of measles infection. Fulminant SSPE is a rare presentation in which the disease progresses to death over a period of 6 months. The clinical features are atypical and can be misleading.
CASE REPORT
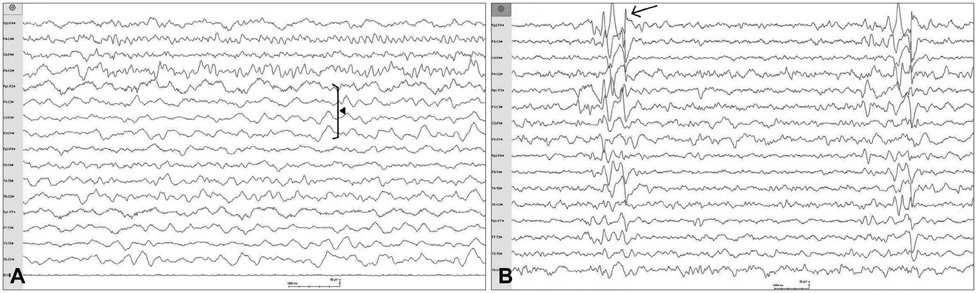
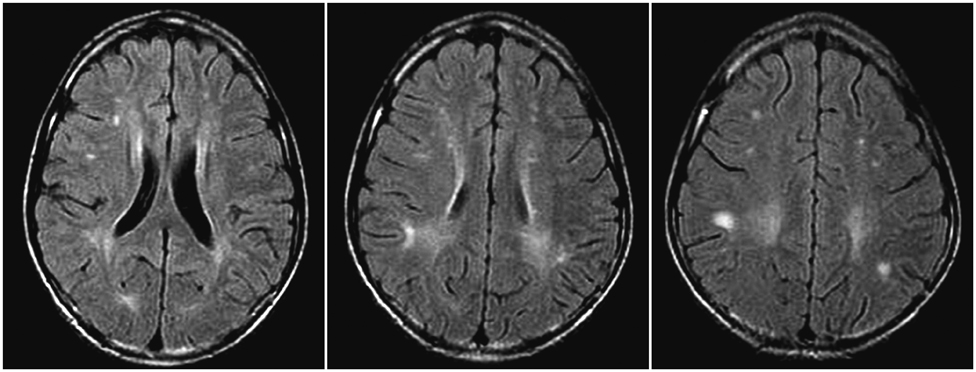
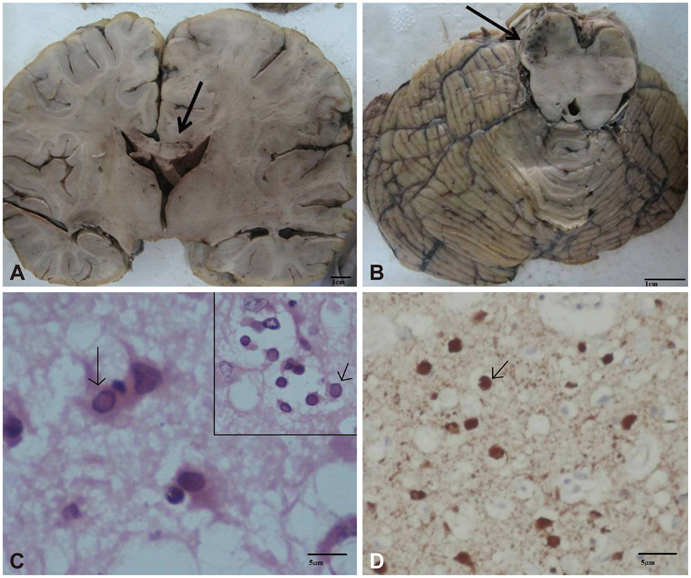
We report herein a teenage boy who presented with acute-onset gait ataxia followed by right hemiparesis that evolved over 1 month, with left-hemispheric, delta-range slowing on the electroencephalogram (EEG). Magnetic resonance imaging disclosed multiple white-matter hyperintensities, suggesting a diagnosis of acute disseminated encephalomyelitis. He received intravenous steroids, and within 4 days of hospital admission he developed unilateral slow myoclonic jerks. Repeat EEG revealed Rademecker complexes, pathognomonic of SSPE, and an elevated titer of IgG antimeasles antibodies was detected in his cerebrospinal fluid. The disease progressed rapidly and the patient succumbed within 15 days of hospitalization. The diagnosis of SSPE was confirmed by autopsy.
CONCLUSIONS
This case illustrates the difficulty of recognizing fulminant SSPE when it manifests with asymmetric clinical and EEG abnormalities.
Keyword
MeSH Terms
-
Adolescent*
Antibodies
Ataxia*
Autopsy
Cerebrospinal Fluid
Diagnosis
Electroencephalography
Encephalomyelitis, Acute Disseminated
Gait Ataxia
Hospitalization
Humans
Immunoglobulin G
Magnetic Resonance Imaging
Male
Measles
Myoclonus
Paresis*
Steroids
Subacute Sclerosing Panencephalitis*
Antibodies
Immunoglobulin G
Steroids
Figure
Reference
-
1. Gutierrez J, Issacson RS, Koppel BS. Subacute sclerosing panencephalitis: an update. Dev Med Child Neurol. 2010; 52:901–907.
Article2. Mahadevan A, Vaidya SR, Wairagkar NS, Khedekar D, Kovoor JM, Santosh V, et al. Case of fulminant-SSPE associated with measles genotype D7 from India: an autopsy study. Neuropathology. 2008; 28:621–626.
Article3. Sarkar N, Gulati S, Dar L, Broor S, Kalra V. Diagnostic dilemmas in fulminant subacute sclerosing panencephalitis (SSPE). Indian J Pediatr. 2004; 71:365–367.
Article4. Ekici B, Calişkan M, Tatli B, Aydinli N, Ozmen M. Rapidly progressive subacute sclerosing panencephalitis presenting with acute loss of vision. Acta Neurol Belg. 2011; 111:325–327.5. Hergüner MO, Altunbaşak S, Baytok V. Patients with acute, fulminant form of SSPE. Turk J Pediatr. 2007; 49:422–425.6. Katrak SM, Mahadevan A, Taly AB, Sinha S, Shankar SK. A 16-year old male with cortical blindness and focal motor seizures. Ann Indian Acad Neurol. 2010; 13:225–232.
Article7. Tuncel D, Ozbek AE, Demirpolat G, Karabiber H. Subacute sclerosing panencephalitis with generalized seizure as a first symptom: a case report. Jpn J Infect Dis. 2006; 59:317–319.8. Kravljanac R, Jovic N, Djuric M, Nikolic L. Epilepsia partialis continua in children with fulminant subacute sclerosing panencephalitis. Neurol Sci. 2011; 32:1007–1012.
Article9. Komur M, Arslankoylu AE, Okuyaz C, Kuyucu N. Atypical clinical course subacute sclerosing panencephalitis presenting as acute Encephalitis. J Pediatr Neurosci. 2012; 7:120–122.
Article10. Cherian A, Sreedharan S, Raghavendra S, Nayak D, Radhakrishnan A. Periodic lateralized epileptiform discharges in fulminant form of SSPE. Can J Neurol Sci. 2009; 36:524–526.
Article11. Ozyürek H, Değerliyurt A, Turanli G. Subacute sclerosing panencephalitis presenting with hemiparesis in childhood: case report. J Child Neurol. 2003; 18:363–365.
Article12. Dyken PR. Subacute sclerosing panencephalitis. Current status. Neurol Clin. 1985; 3:179–196.13. Yaramiş A, Taşkesen M. Brainstem involvement in subacute sclerosing panencephalitis. Turk J Pediatr. 2010; 52:542–545.14. Sharma P, Singh D, Singh MK, Garg RK, Kohli N. Brainstem involvement in subacute sclerosing panencephalitis. Neurol India. 2011; 59:273–275.
Article15. Prashanth LK, Taly AB, Ravi V, Sinha S, Rao S. Long term survival in subacute sclerosing panencephalitis: an enigma. Brain Dev. 2006; 28:447–452.
Article16. Serdaroglu G, Kutlu A, Tekgul H, Tutuncuoglu S. Subacute sclerosing panencephalitis: a case with fulminant course after ACTH. Pediatr Neurol. 2004; 31:67–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Subacute Sclerosing Panencephalitis
- A long-term subacute sclerosing panencephalitis survivor treated with intraventricular interferon-alpha for 13 years
- Subacute Sclerosing Panencephalitis: Clinical Experience of 6 Cases
- Clinical Experience of Subacute Sclerosing Panencephalitis treated with Alpha-interferon and Ionsiplex
- Subacute sclerosing panencephalitis presenting as young adult onset parkinsonism