J Breast Cancer.
2010 Jun;13(2):167-173. 10.4048/jbc.2010.13.2.167.
Predictors of 4 or More Positive Axillary Nodes in Patients with Node-positive T1-2 Breast Carcinoma: The Indications for Adjuvant Irradiation of the Level III Axilla and Supraclavicular Fossa
- Affiliations
-
- 1Department of Radiation Oncology, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea. kimandre@catholic.ac.kr
- 2Department of Surgery, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
- 3Department of Internal Medicine, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
- KMID: 2286542
- DOI: http://doi.org/10.4048/jbc.2010.13.2.167
Abstract
- PURPOSE
We evaluate the predictors of 4 or more involved axillary nodes in patients with node-positive T1-2 breast carcinoma to select a group of patients who are indicated for adjuvant irradiation of the level III axilla and supraclavicular fossa (SCF).
METHODS
We analyzed 286 patients with positive axillary nodes and who were without distant metastases and who underwent breast conserving surgery and axillary lymph node dissection or modified radical mastectomy. We investigated the relationship between the patients and the tumor factors and 4 or more positive axillary nodes.
RESULTS
On the multivariate logistic-regression analysis, an increased tumor size (p=0.002), the presence of lymphovascular space invasion (LVSI) (p<0.001) and a palpable mass p<0.001) were positively associated with involvement of 4 or more axillary lymph nodes. In our study, 86.1% of the patients with all the unfavorable factors had involvement of 4 or more nodal metastases.
CONCLUSION
Our data suggest that for patients with node-positive T1-2 breast cancer, the presence of 4 or more involved nodes is frequently observed for the patients with an increased tumor size, the presence of LVSI and a palpable mass at the time of diagnosis, and we recommend that they undergo irradiation of the high axilla and SCF for adjuvant care, if they do not undergo complete axillary dissection.
Keyword
MeSH Terms
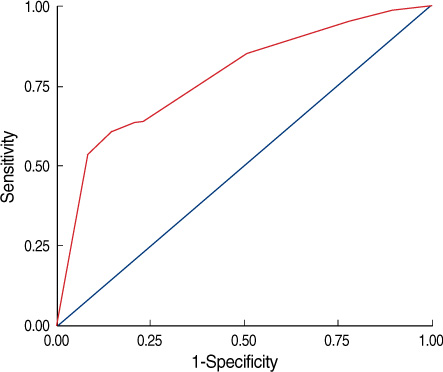
Figure
Reference
-
1. Moran MS, Haffty BG. Local-regional breast cancer recurrence: prognostic groups based on patterns of failure. Breast J. 2002; 8:81–87.
Article2. Recht A, Gray R, Davidson NE, Fowble BL, Solin LJ, Cummings FJ, et al. Locoregional failure ten years after mastectomy and adjuvant chemotherapy with or without tamoxifen without radiation: experience of the Eastern Cooperative Oncology Group. J Clin Oncol. 1999; 17:1689–1700.3. Shim SJ, Kim YB, Keum KC, Lee IJ, Lee HD, Suh CO. Validation of radiation volume by analysis of recurrence pattern in breast-conserving treatment for early breast cancer. J Breast Cancer. 2009; 4:257–264.
Article4. Galper S, Recht A, Silver B, Manola J, Gelman R, Schnitt SJ, et al. Factors associated with regional nodal failure in patients with early stage breast cancer with 0-3 positive axillary nodes following tangential irradiation alone. Int J Radiat Oncol Biol Phys. 1999; 45:1157–1166.
Article5. Halverson KJ, Taylor ME, Perez CA, Garcia DM, Myerson R, Philpott G, et al. Regional nodal management patterns of failure following conservative surgery and radiation therapy for stage I and II breast cancer. Int J Radiat Oncol Biol Phys. 1993; 26:593–599.6. Grills IS, Kestin LL, Goldstein N, Mitchell C, Martinez A, Ingold J, et al. Risk factors for regional nodal failure after breast conserving therapy: regional nodal irradiation reduces rate of axillary failure in patients with four or more positive lymph nodes. Int J Radiat Oncol Biol Phys. 2003; 56:658–670.7. Schlembach PJ, Buchholz TA, Ross MI, Kirsner SM, Salas GJ, Strom EA, et al. Relationship of sentinel and axillary level I-II lymph nodes to tangential fields used in breast irradiation. Int J Radiat Oncol Biol Phys. 2001; 51:671–678.
Article8. Coen JJ, Taghian AG, Kachnic LA, Assaad SI, Powell SN. Risk of lymphedema after regional nodal irradiation with breast conservation therapy. Int J Radiat Oncol Biol Phys. 2003; 55:1209–1215.9. Kim HJ, Jang WI, Kim TJ, Kim JH, Kim SW, Moon SH, et al. Radiation-induced pulmonary toxicity and related risk factors in breast cancer. J Breast Cancer. 2009; 2:67–72.
Article10. Johansson S, Svensson H, Denekamp J. Dose response and latency for radiation-induced fibrosis, edema, and neuropathy in breast cancer patients. Int J Radiat Oncol Biol Phys. 2002; 52:1207–1219.
Article11. Frederick LG, David LP, Irvin DF, April F, Charles MB, Daniel GH, et al. In: AJCC Cancer Staging Manual/American Joint Committee on Cancer. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2002. pp. 223-240.12. Kambouris AA. Axillary node metastases in relation to size and location of breast cancers: analysis of 147 patients. Am Surg. 1996; 7:519–524.13. Fein DA, Fowble BL, Hanlon AL, Hooks MA, Hoffman JP, Sigurdson ER, et al. Identification of women with T1-T2 breast cancer at low risk of positive axillary nodes. J Surg Oncol. 1997; 1:34–39.
Article14. Cetintaş SK, Kurt M, Ozkan L, Engin K, Gökgöz S, Taşdelen I. Factors influencing axillary node metastasis in breast cancer. Tumori. 2006; 92:416–422.
Article15. Jonjic N, Mustac E, Dekanic A, Marijic B, Gaspar B, Kolic I, et al. Predicting sentinel lymph node metastases in infiltrating breast carcinoma with vascular invasion. Int J Surg Pathol. 2006; 14:306–311.
Article16. Silverstein MJ, Skinner KA, Lomis TJ. Predicting axillary nodal positivity in 2282 patients with breast carcinoma. World J Surg. 2001; 25:767–772.
Article17. Shahar KH, Hunt KK, Thames HD, Ross MI, Perkins GH, Kuerer HM, et al. Factors predictive of having four or more positive axillary lymph nodes in patients with positive sentinel lymph nodes: implications for selection of radiation fields. Int J Radiat Oncol Biol Phys. 2004; 59:1074–1079.
Article18. Katz A, Niemierko A, Gage I, Evans S, Shaffer M, Smith FP, et al. Factors associated with involvement of four or more axillary nodes for sentinel lymph node-positive patients. Int J Radiat Oncol Biol Phys. 2006; 65:40–44.
Article19. Katz A, Smith BL, Golshan M, Niemierko A, Kobayashi W, Raad RA, et al. Nomogram for the prediction of having four or more involved nodes for sentinel lymph node-positive breast cancer. J Clin Oncol. 2008; 26:2093–2098.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Axillary Lymph-Node Metastases in Patients with T1 Breast Cancer
- Virtual lymph node analysis to evaluate axillary lymph node coverage provided by tangential breast irradiation
- A Recurrence of Ovarian Carcinoma Presenting as Only Axillary Lymphatic Metastasis: A Case Report
- The Prognosis of breast Cancr with more than 10 Positive Nodes
- Tumor Characteristics Influencing Non-Sentinel Lymph Node Involvement in Clinically Node Negative Patients with Breast Cancer