J Breast Cancer.
2012 Mar;15(1):1-6. 10.4048/jbc.2012.15.1.1.
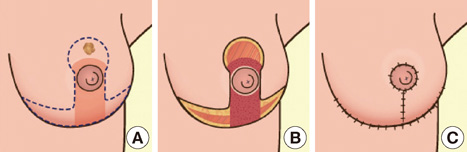
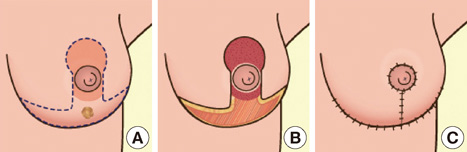
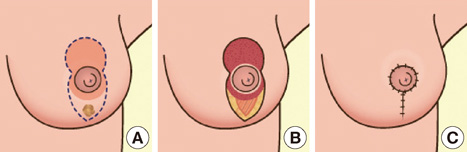
Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 1): Volume Displacement
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Kyungpook National University School of Medicine, Daegu, Korea.
- 2Department of Surgery, Kyungpook National University School of Medicine, Daegu, Korea. phy123@knu.ac.kr
- KMID: 2286467
- DOI: http://doi.org/10.4048/jbc.2012.15.1.1
Abstract
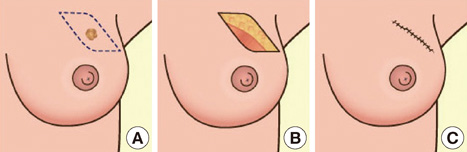
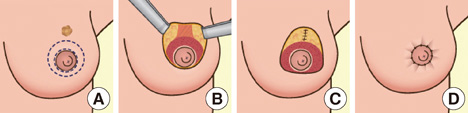
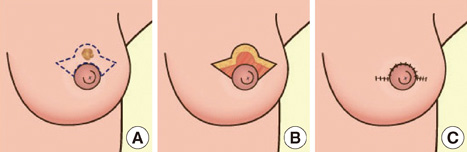
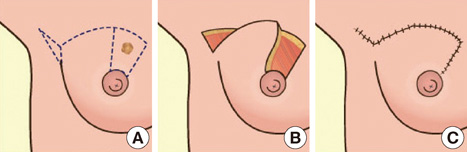
- Despite the popularity of breast-conserving surgery (BCS), which constitutes 50-60% of all breast cancer surgeries, discussions regarding cosmetic results after BCS are not specifically conducted. The simple conservation of breast tissue is no longer adequate to qualify for BCS completion. The incorporation of oncological and plastic surgery techniques allows for the complete resection of local disease while achieving superior cosmetic outcome. Oncoplastic BCS can be performed in one of the following two ways: 1) volume displacement techniques and 2) volume replacement techniques. This study reports volume displacement surgical techniques, which allow the use of remaining breast tissue after BCS by glandular reshaping or reduction techniques for better cosmetic results. Thorough understanding of these procedures and careful consideration of the patient's breast size, tumor location, excised volume, and volume of the remaining breast tissue during the surgery in choosing appropriate patient and surgical techniques will result in good cosmetic results. Surgery of the contralateral breast may be requested to improve symmetry and may take the form of a reduction mammoplasty or mastopexy. The timing of such surgery and the merits of synchronous versus delayed approaches should be discussed in full with the patients. Because Korean women have relatively small breast sizes compared to Western women, it is not very easy to apply the oncoplastic volume displacement technique to cover defects. However, we have performed various types of oncoplastic volume displacement techniques on Korean women, and based on our experience, we report a number of oncoplastic volume displacement techniques that are applicable to Korean women with small- to moderate-sized breasts.
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Oncoplastic Breast-Conserving Surgery and Breast-Conserving Surgery Alone: A Meta-Analysis
Jun-Ying Chen, Yi-Jie Huang, Liu-Lu Zhang, Ci-Qiu Yang, Kun Wang
J Breast Cancer. 2018;21(3):321-329. doi: 10.4048/jbc.2018.21.e36.
Reference
-
1. Yang JD, Lee JW, Kim WW, Jung JH, Park HY. Oncoplastic surgical techniques for personalized breast conserving surgery in breast cancer patient with small to moderate sized breast. J Breast Cancer. 2011. 14:253–261.
Article2. Yang JD, Bae SG, Chung HY, Cho BC, Park HY, Jung JH. The usefulness of oncoplastic volume displacement techniques in the superiorly located breast cancers for Korean patients with small to moderate-sized breasts. Ann Plast Surg. 2011. 67:474–480.
Article3. Anderson BO, Masetti R, Silverstein MJ. Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Lancet Oncol. 2005. 6:145–157.
Article4. Berry MG, Fitoussi AD, Curnier A, Couturaud B, Salmon RJ. Oncoplastic breast surgery: a review and systematic approach. J Plast Reconstr Aesthet Surg. 2010. 63:1233–1243.
Article5. Malka I, Villet R, Fitoussi A, Salmon RJ. Oncoplastic conservative treatment for breast cancer (part 3): techniques for the upper quadrants. J Visc Surg. 2010. 147:e365–e372.
Article6. Chang E, Johnson N, Webber B, Booth J, Rahhal D, Gannett D, et al. Bilateral reduction mammoplasty in combination with lumpectomy for treatment of breast cancer in patients with macromastia. Am J Surg. 2004. 187:647–650.
Article7. Smith ML, Evans GR, Gürlek A, Bouvet M, Singletary SE, Ames FC, et al. Reduction mammaplasty: its role in breast conservation surgery for early-stage breast cancer. Ann Plast Surg. 1998. 41:234–239.8. Losken A, Elwood ET, Styblo TM, Bostwick J 3rd. The role of reduction mammaplasty in reconstructing partial mastectomy defects. Plast Reconstr Surg. 2002. 109:968–975.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 2): Volume Replacement
- Oncoplastic Surgical Techniques for Personalized Breast Conserving Surgery in Breast Cancer Patient with Small to Moderate Sized Breast
- Usefulness of Oncoplastic Volume Replacement Techniques after Breast Conserving Surgery in Small to Moderate-sized Breasts
- Partial Breast Reconstruction Using Various Oncoplastic Techniques for Centrally Located Breast Cancer
- Oncoplastic Breast Surgery