J Breast Cancer.
2012 Sep;15(3):320-328. 10.4048/jbc.2012.15.3.320.
Correlation of Conventional and Conformal Plan Parameters for Predicting Radiation Pneumonitis in Patients Treated with Breast Cancer
- Affiliations
-
- 1Department of Radiation Oncology, Baskent University Faculty of Medicine, Adana Research and Treatment Centre, Adana, Turkey. hcemonal@hotmail.com
- KMID: 2286458
- DOI: http://doi.org/10.4048/jbc.2012.15.3.320
Abstract
- PURPOSE
The purpose of this study is to evaluate the correlation between the conventional plan parameters and dosimetric parameters obtained from conformal radiotherapy (RT) planning, and between these parameters and radiation pneumontitis (RP) incidence.
METHODS
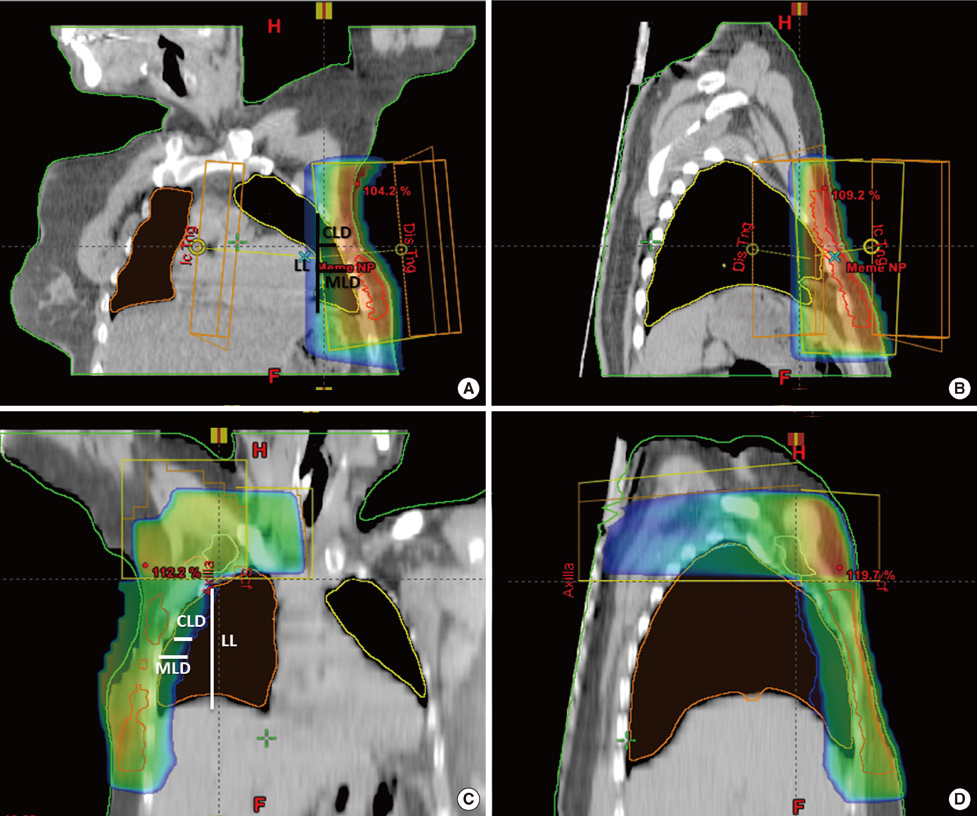
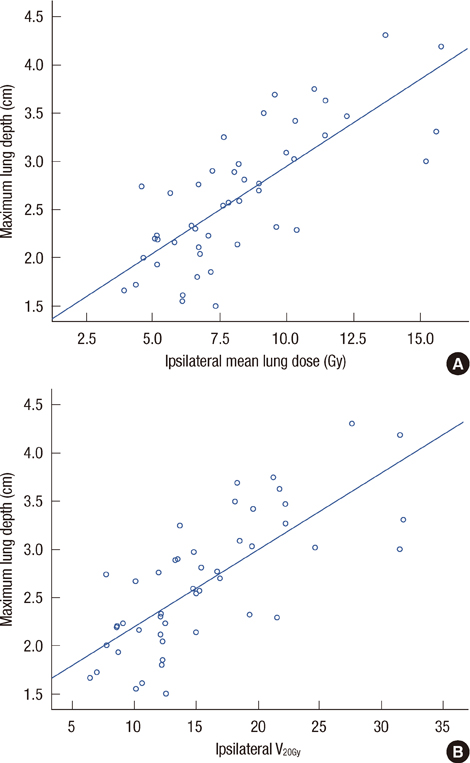
Clinical and dosimetric data of 122 patients that were treated with mastectomy and adjuvant 3D conformal RT (39% received 2-field RT [2-FRT], and in addition, 61% received 4-field RT [4-FRT]) were retrospectively analyzed. Central lung depth (CLD), maximum lung depth (MLD), and lung length were measured by the conventional plan. Lung dose-volume histograms (DVH) were created with conformal planning, and the lung volumes receiving 5 to 50 Gy (V5Gy to V50Gy) were calculated. Minimum (Dmin), maximum (Dmax), and mean doses (Dmean) for the ipsilateral lung and bilateral lungs were measured by DVH. Correlations between 3D dosimetric data and 2D radiographic parameters were analyzed.
RESULTS
The conventional plan parameters did not significantly differ between 2-FRT and 4-FRT. The conformal plan Dmin, Dmax, and Dmean values were higher in 4-FRT versus 2-FRT. CLD and MLD were correlated with DVH parameter V5Gy to V45Gy values for ipsilateral, as well as bilateral lungs for 2-FRT. MLD and ipsilateral Dmean via 2-FRT planning had the strongest positive correlation (r=0.76, p<0.01). Moderate correlations existed between CLD and ipsilateral and bilateral lung V5Gy-45Gy, and between MLD and bilateral lung V5Gy-45Gy values in 2-FRT. Only four patients developed symptomatic RP, 4 with 4-FRT and one with 2-FRT.
CONCLUSION
The conformal plan parameters were strongly correlated with dose-volume parameters for breast 2-FRT. With only 4 cases of Grade 3 RP observed, our study is limited in its ability to provide definitive guidance, however assuming that CLD is an indicator for RP, V20Gy could be used as a predictor for RP and for 2-FRT. A well-defined parameters are still required to predict RP in 4-FRT.
Keyword
MeSH Terms
Figure
Reference
-
1. Recht A. Integration of systemic therapy and radiation therapy for patients with early-stage breast cancer treated with conservative surgery. Clin Breast Cancer. 2003. 4:104–113.
Article2. Olivotto IA, Chua B, Elliott EA, Parda DS, Pierce LJ, Shepherd L, et al. A clinical trial of breast radiation therapy versus breast plus regional radiation therapy in early-stage breast cancer: the MA20 trial. Clin Breast Cancer. 2003. 4:361–363.
Article3. Neal AJ, Yarnold JR. Estimating the volume of lung irradiated during tangential breast irradiation using the central lung distance. Br J Radiol. 1995. 68:1004–1008.
Article4. Das IJ, Cheng EC, Freedman G, Fowble B. Lung and heart dose volume analyses with CT simulator in radiation treatment of breast cancer. Int J Radiat Oncol Biol Phys. 1998. 42:11–19.
Article5. Teh AY, Park EJ, Shen L, Chung HT. Three-dimensional volumetric analysis of irradiated lung with adjuvant breast irradiation. Int J Radiat Oncol Biol Phys. 2009. 75:1309–1315.
Article6. Kong FM, Klein EE, Bradley JD, Mansur DB, Taylor ME, Perez CA, et al. The impact of central lung distance, maximal heart distance, and radiation technique on the volumetric dose of the lung and heart for intact breast radiation. Int J Radiat Oncol Biol Phys. 2002. 54:963–971.
Article7. Chie EK, Shin KH, Kim DY, Kim TH, Kang HS, Lee ES, et al. Radiation pneumonitis after adjuvant radiotherapy for breast cancer: a volumetric analysis using CT simulator. J Breast Cancer. 2009. 12:73–78.
Article8. Lind PA, Wennberg B, Gagliardi G, Fornander T. Pulmonary complications following different radiotherapy techniques for breast cancer, and the association to irradiated lung volume and dose. Breast Cancer Res Treat. 2001. 68:199–210.
Article9. Lind PA, Marks LB, Hardenbergh PH, Clough R, Fan M, Hollis D, et al. Technical factors associated with radiation pneumonitis after local +/- regional radiation therapy for breast cancer. Int J Radiat Oncol Biol Phys. 2002. 52:137–143.
Article10. Hernando ML, Marks LB, Bentel GC, Zhou SM, Hollis D, Das SK, et al. Radiation-induced pulmonary toxicity: a dose-volume histogram analysis in 201 patients with lung cancer. Int J Radiat Oncol Biol Phys. 2001. 51:650–659.
Article11. Yorke ED, Jackson A, Rosenzweig KE, Merrick SA, Gabrys D, Venkatraman ES, et al. Dose-volume factors contributing to the incidence of radiation pneumonitis in non-small-cell lung cancer patients treated with three-dimensional conformal radiation therapy. Int J Radiat Oncol Biol Phys. 2002. 54:329–339.
Article12. Martinez-Monge R, Fernandes PS, Gupta N, Gahbauer R. Cross-sectional nodal atlas: a tool for the definition of clinical target volumes in three-dimensional radiation therapy planning. Radiology. 1999. 211:815–828.
Article13. Li XA, Tai A, Arthur DW, Buchholz TA, Macdonald S, Marks LB, et al. Variability of target and normal structure delineation for breast cancer radiotherapy: an RTOG Multi-Institutional and Multiobserver Study. Int J Radiat Oncol Biol Phys. 2009. 73:944–951.
Article14. Castro Pena P, Kirova YM, Campana F, Dendale R, Bollet MA, Fournier-Bidoz N, et al. Anatomical, clinical and radiological delineation of target volumes in breast cancer radiotherapy planning: individual variability, questions and answers. Br J Radiol. 2009. 82:595–599.
Article15. Atahan IL, Ozyigit G, Yildiz F, Gurkaynak M, Selek U, Sari S, et al. Percent positive axillary involvement predicts for the development of brain metastasis in high-risk patients with nonmetastatic breast cancer receiving post-mastectomy radiotherapy. Breast J. 2008. 14:245–249.
Article16. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995. 31:1341–1346.
Article17. Maguire PD, Marks LB, Sibley GS, Herndon JE 2nd, Clough RW, Light KL, et al. 73.6 Gy and beyond: hyperfractionated, accelerated radiotherapy for non-small-cell lung cancer. J Clin Oncol. 2001. 19:705–711.
Article18. Chung HT, Xia P, Chan LW, Park-Somers E, Roach M 3rd. Does image-guided radiotherapy improve toxicity profile in whole pelvic-treated high-risk prostate cancer? Comparison between IG-IMRT and IMRT. Int J Radiat Oncol Biol Phys. 2009. 73:53–60.
Article19. Tsoutsou PG, Koukourakis MI. Radiation pneumonitis and fibrosis: mechanisms underlying its pathogenesis and implications for future research. Int J Radiat Oncol Biol Phys. 2006. 66:1281–1293.
Article20. Kim TH, Cho KH, Pyo HR, Lee JS, Zo JI, Lee DH, et al. Dose-volumetric parameters for predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer. Radiology. 2005. 235:208–215.
Article21. Wang S, Liao Z, Wei X, Liu HH, Tucker SL, Hu CS, et al. Analysis of clinical and dosimetric factors associated with treatment-related pneumonitis (TRP) in patients with non-small-cell lung cancer (NSCLC) treated with concurrent chemotherapy and three-dimensional conformal radiotherapy (3D-CRT). Int J Radiat Oncol Biol Phys. 2006. 66:1399–1407.
Article22. Seppenwoolde Y, De Jaeger K, Boersma LJ, Belderbos JS, Lebesque JV. Regional differences in lung radiosensitivity after radiotherapy for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2004. 60:748–758.
Article23. Tsujino K, Hirota S, Endo M, Obayashi K, Kotani Y, Satouchi M, et al. Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys. 2003. 55:110–115.
Article24. Hurkmans CW, Borger JH, Bos LJ, van der Horst A, Pieters BR, Lebesque JV, et al. Cardiac and lung complication probabilities after breast cancer irradiation. Radiother Oncol. 2000. 55:145–151.
Article25. Kahan Z, Csenki M, Varga Z, Szil E, Cserháti A, Balogh A, et al. The risk of early and late lung sequelae after conformal radiotherapy in breast cancer patients. Int J Radiat Oncol Biol Phys. 2007. 68:673–681.
Article26. Varga Z, Cserháti A, Kelemen G, Boda K, Thurzó L, Kahán Z. Role of systemic therapy in the development of lung sequelae after conformal radiotherapy in breast cancer patients. Int J Radiat Oncol Biol Phys. 2011. 80:1109–1116.
Article27. Bartelink H, Garavaglia G, Johansson KA, Mijnheer BJ, Van den Bogaert W, van Tienhoven G, et al. Quality assurance in conservative treatment of early breast cancer. Report on a consensus meeting of the EORTC Radiotherapy and Breast Cancer Cooperative Groups and the EUSOMA (European Society of Mastology). Radiother Oncol. 1991. 22:323–326.28. Lingos TI, Recht A, Vicini F, Abner A, Silver B, Harris JR. Radiation pneumonitis in breast cancer patients treated with conservative surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 1991. 21:355–360.
Article29. Minor GI, Yashar CM, Spanos WJ Jr, Jose BO, Silverman CL, Carrascosa LA, et al. The relationship of radiation pneumonitis to treated lung volume in breast conservation therapy. Breast J. 2006. 12:48–52.
Article30. Bentzen SM, Constine LS, Deasy JO, Eisbruch A, Jackson A, Marks LB, et al. Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC): an introduction to the scientific issues. Int J Radiat Oncol Biol Phys. 2010. 76:3 Suppl. S3–S9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiation Pneumonitis in Breast Cancer Patients Who Received Radiotherapy Using the Partially Wide Tangent Technique after Breast Conserving Surgery
- Comparative Study Between Respiratory Gated Conventional 2-D Plan and 3-D Conformal Plan for Predicting Radiation Hepatitis
- Probabilities of Pulmonary and Cardiac Complications and Radiographic Parameters in Breast Cancer Radiotherapy
- Internal Mammary Lymph Node Irradiation after Breast Conservation Surgery: Radiation Pneumonitis versus Dose?Volume Histogram Parameters
- Radiation Induced Lung Damage : Mechanisms and Clinical Implications