J Breast Cancer.
2014 Sep;17(3):265-269. 10.4048/jbc.2014.17.3.265.
Absence of Residual Microcalcifications in Atypical Ductal Hyperplasia Diagnosed via Stereotactic Vacuum-Assisted Breast Biopsy: Is Surgical Excision Obviated?
- Affiliations
-
- 1Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Radiology, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea. ekkim@yuhs.ac
- KMID: 2286354
- DOI: http://doi.org/10.4048/jbc.2014.17.3.265
Abstract
- PURPOSE
The purpose of our study was to evaluate the underestimation rate of atypical ductal hyperplasia (ADH) on vacuum-assisted breast biopsy (VABB), and to examine the correlation between residual microcalcifications and the underestimation rate of ADH.
METHODS
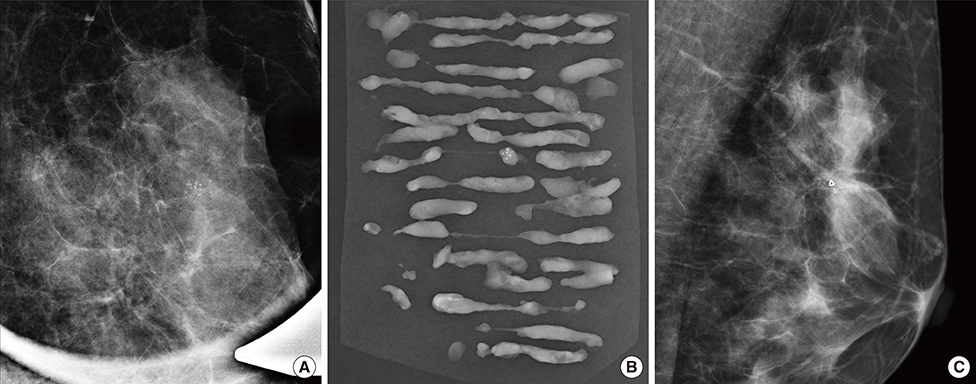
A retrospective study was performed on 27 women (mean age, 49.2+/-9.2 years) who underwent additional excision for ADH via VABB for microcalcifications observed by using mammography. The mammographic findings, histopathologic diagnosis of all VABB and surgical specimens, and association of malignancy with residual microcalcifications were evaluated. The underestimation rate of ADH was also calculated.
RESULTS
Of the 27 women with microcalcifications, nine were upgraded to ductal carcinoma in situ (DCIS); thus, the underestimation rate was 33.3% (9/27). There was no difference in age (p=0.40) and extent of microcalcifications (p=0.10) when comparing benign and malignant cases. Six of 17 patients (35.3%) with remaining calcifications after VABB were upgraded to DCIS, and three of 10 patients (30%) with no residual calcifications after VABB were upgraded (p=1.00).
CONCLUSION
The underestimation rate of ADH on VABB was 33.3%. Furthermore, 30% of patients with no remaining calcifications were upgraded to DCIS. Therefore, we conclude that all ADH cases diagnosed via VABB should be excised regardless of the presence of residual microcalcifications.
MeSH Terms
Figure
Reference
-
1. Nguyen CV, Albarracin CT, Whitman GJ, Lopez A, Sneige N. Atypical ductal hyperplasia in directional vacuum-assisted biopsy of breast microcalcifications: considerations for surgical excision. Ann Surg Oncol. 2011; 18:752–761.
Article2. McGhan LJ, Pockaj BA, Wasif N, Giurescu ME, McCullough AE, Gray RJ. Atypical ductal hyperplasia on core biopsy: an automatic trigger for excisional biopsy? Ann Surg Oncol. 2012; 19:3264–3269.
Article3. Jain RK, Mehta R, Dimitrov R, Larsson LG, Musto PM, Hodges KB, et al. Atypical ductal hyperplasia: interobserver and intraobserver variability. Mod Pathol. 2011; 24:917–923.
Article4. Polat AK, Kanbour-Shakir A, Andacoglu O, Polat AV, Johnson R, Bonaventura M, et al. Atypical hyperplasia on core biopsy: is further surgery needed? Am J Med Sci. 2012; 344:28–31.
Article5. Winchester DJ, Bernstein JR, Jeske JM, Nicholson MH, Hahn EA, Goldschmidt RA, et al. Upstaging of atypical ductal hyperplasia after vacuum-assisted 11-gauge stereotactic core needle biopsy. Arch Surg. 2003; 138:619–622.
Article6. Liberman L, Smolkin JH, Dershaw DD, Morris EA, Abramson AF, Rosen PP. Calcification retrieval at stereotactic, 11-gauge, directional, vacuum-assisted breast biopsy. Radiology. 1998; 208:251–260.
Article7. Philpotts LE, Lee CH, Horvath LJ, Lange RC, Carter D, Tocino I. Underestimation of breast cancer with II-gauge vacuum suction biopsy. AJR Am J Roentgenol. 2000; 175:1047–1050.
Article8. Arora S, Moezzi M, Kim U, Menes TS. Is surgical excision necessary for atypical ductal hyperplasia diagnosed with 8 gauge stereotactic biopsy? Breast J. 2009; 15:673–674.
Article9. Lourenco AP, Mainiero MB, Lazarus E, Giri D, Schepps B. Stereotactic breast biopsy: comparison of histologic underestimation rates with 11- and 9-gauge vacuum-assisted breast biopsy. AJR Am J Roentgenol. 2007; 189:W275–W279.
Article10. Park HL, Kim LS. The current role of vacuum assisted breast biopsy system in breast disease. J Breast Cancer. 2011; 14:1–7.
Article11. Jung YJ, Bae YT, Lee JY, Seo HI, Kim JY, Choo KS. Lateral decubitus positioning stereotactic vacuum-assisted breast biopsy with true lateral mammography. J Breast Cancer. 2011; 14:64–68.
Article12. Adrales G, Turk P, Wallace T, Bird R, Norton HJ, Greene F. Is surgical excision necessary for atypical ductal hyperplasia of the breast diagnosed by Mammotome? Am J Surg. 2000; 180:313–315.
Article13. Sneige N, Lim SC, Whitman GJ, Krishnamurthy S, Sahin AA, Smith TL, et al. Atypical ductal hyperplasia diagnosis by directional vacuum-assisted stereotactic biopsy of breast microcalcifications. Considerations for surgical excision. Am J Clin Pathol. 2003; 119:248–253.
Article14. Teng-Swan Ho J, Tan PH, Hee SW, Su-Lin Wong J. Underestimation of malignancy of atypical ductal hyperplasia diagnosed on 11-gauge stereotactically guided Mammotome breast biopsy: an Asian breast screen experience. Breast. 2008; 17:401–406.
Article15. Dupont WD, Parl FF, Hartmann WH, Brinton LA, Winfield AC, Worrell JA, et al. Breast cancer risk associated with proliferative breast disease and atypical hyperplasia. Cancer. 1993; 71:1258–1265.
Article16. Jackman RJ, Birdwell RL, Ikeda DM. Atypical ductal hyperplasia: can some lesions be defined as probably benign after stereotactic 11-gauge vacuum-assisted biopsy, eliminating the recommendation for surgical excision? Radiology. 2002; 224:548–554.
Article17. Liberman L, LaTrenta LR, Van Zee KJ, Morris EA, Abramson AF, Dershaw DD. Stereotactic core biopsy of calcifications highly suggestive of malignancy. Radiology. 1997; 203:673–677.
Article18. de Mascarel I, Brouste V, Asad-Syed M, Hurtevent G, Macgrogan G. All atypia diagnosed at stereotactic vacuum-assisted breast biopsy do not need surgical excision. Mod Pathol. 2011; 24:1198–1206.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- US-Guided Vacuum-Assisted Biopsy of Microcalcifications in Breast Lesions and Long-Term Follow-Up Results
- Impact of Non-Calcified Specimen Pathology on the Underestimation of Malignancy for the Incomplete Retrieval of Suspicious Calcifications Diagnosed as Flat Epithelial Atypia or Atypical Ductal Hyperplasia by Stereotactic Vacuum-Assisted Breast Biopsy
- Lateral Decubitus Positioning Stereotactic Vacuum-Assisted Breast Biopsy with True Lateral Mammography
- Stereotactic Vacuum-Assisted Biopsy of Microcalcifications Using an Upright Add-On Type Stereotactic Mammography Unit
- US-guided Vacuum-assisted Breast Biopsy with Air Localization for Patients with Microcalcifications