J Breast Cancer.
2015 Mar;18(1):36-43. 10.4048/jbc.2015.18.1.36.
Operable Breast Cancer of the Inner Hemisphere Is Associated with Poor Survival
- Affiliations
-
- 1Department of Medical Oncology, Sun Yat-Sen University Cancer Center; State Key Laboratory of Oncology in South China; Collaborative Innovation Center of Cancer Medicine, Guangzhou, China. yuanzhygz@163.com
- KMID: 2286335
- DOI: http://doi.org/10.4048/jbc.2015.18.1.36
Abstract
- PURPOSE
This study investigated the clinicopathological features of operable breast cancer lesions located in different hemispheres of the breast and determined related survival outcomes.
METHODS
Data from 5,330 patients with invasive ductal carcinoma were retrospectively analyzed based on tumor location.
RESULTS
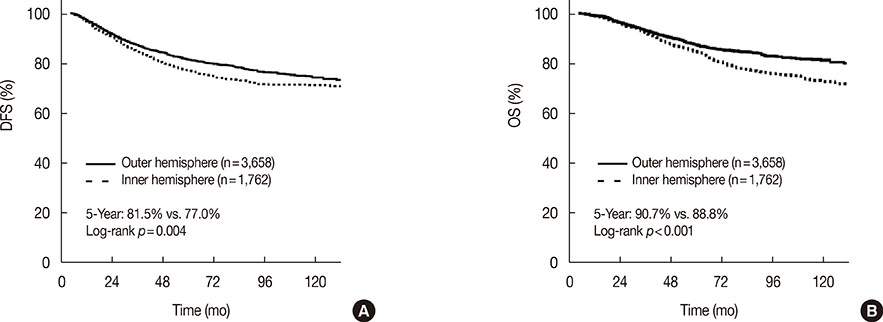
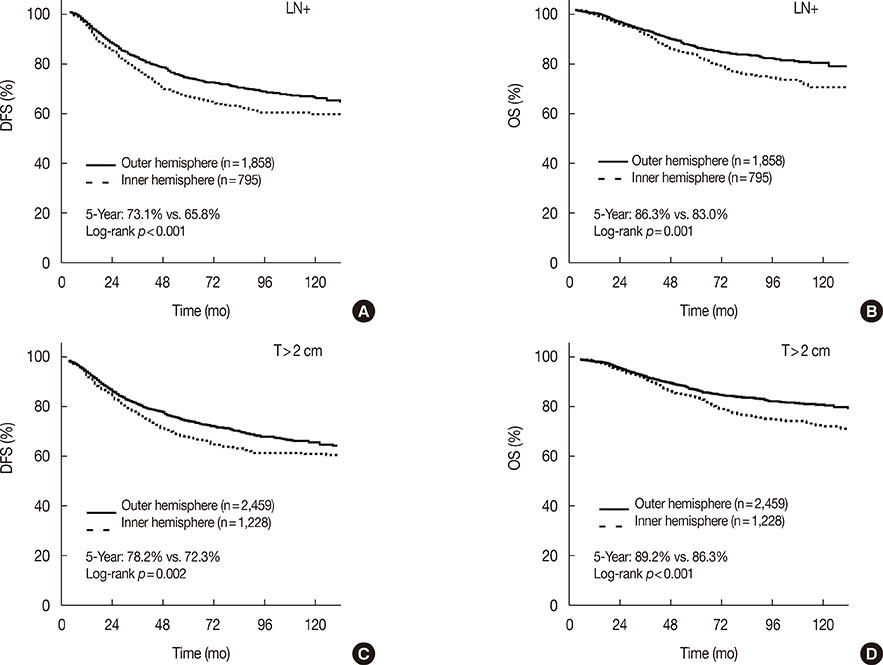
The median follow-up time was 68 months (range, 18-176 months). Patients with breast cancer located in the outer hemisphere of the breast had lesions with more advanced nodal stages and more frequently received adjuvant chemotherapy than patients with breast cancer in the inner hemisphere. The 5-year disease-free survival (DFS) rates of patients with tumors located in outer versus inner hemispheres were 81.5% and 77.0%, respectively (p=0.004); the overall survival (OS) rates were 90.7% and 88.8%, respectively (p<0.001). The association between tumor location and the 5-year DFS rate was most apparent in node-positive patients (73.1% vs. 65.8% for outer vs. inner hemisphere lesions, p<0.001) and in patients with primary tumors greater than 2 cm in diameter (78.2% vs. 72.3%, p=0.002). Multivariate analysis showed that tumor location was an independent predictor of DFS (hazard ratio [HR], 1.23; p=0.002) and OS (HR, 1.28; p=0.006). There were no significant differences in 5-year DFS or OS rates between patients with outer versus inner hemisphere tumors when internal mammary node irradiation was performed.
CONCLUSION
This study demonstrated that tumor location was an independent prognostic factor for operable breast cancer. Internal mammary node irradiation is recommended for patients with breast cancer of the inner hemisphere and positive axillary lymph nodes or large primary tumors.
Keyword
MeSH Terms
Figure
Reference
-
1. Zucali R, Mariani L, Marubini E, Kenda R, Lozza L, Rilke F, et al. Early breast cancer: evaluation of the prognostic role of the site of the primary tumor. J Clin Oncol. 1998; 16:1363–1366.
Article2. Arriagada R, Lê MG, Mouriesse H, Fontaine F, Dewar J, Rochard F, et al. Long-term effect of internal mammary chain treatment: results of a multivariate analysis of 1195 patients with operable breast cancer and positive axillary nodes. Radiother Oncol. 1988; 11:213–222.
Article3. Høst H, Brennhovd IO, Loeb M. Postoperative radiotherapy in breast cancer: long-term results from the Oslo study. Int J Radiat Oncol Biol Phys. 1986; 12:727–732.
Article4. Lacour J, Bucalossi P, Cacers E, Jacobelli G, Koszarowski T, Le M, et al. Radical mastectomy versus radical mastectomy plus internal mammary dissection: five-year results of an international cooperative study. Cancer. 1976; 37:206–214.
Article5. Xue C, Wang X, Peng R, Shi Y, Qin T, Liu D, et al. Distribution, clinicopathologic features and survival of breast cancer subtypes in Southern China. Cancer Sci. 2012; 103:1679–1687.
Article6. Gaffney DK, Tsodikov A, Wiggins CL. Diminished survival in patients with inner versus outer quadrant breast cancers. J Clin Oncol. 2003; 21:467–472.
Article7. Colleoni M, Zahrieh D, Gelber RD, Holmberg SB, Mattsson JE, Rudenstam CM, et al. Site of primary tumor has a prognostic role in operable breast cancer: the international breast cancer study group experience. J Clin Oncol. 2005; 23:1390–1400.
Article8. Lohrisch C, Jackson J, Jones A, Mates D, Olivotto IA. Relationship between tumor location and relapse in 6,781 women with early invasive breast cancer. J Clin Oncol. 2000; 18:2828–2835.
Article9. Huang O, Wang L, Shen K, Lin H, Hu Z, Liu G, et al. Breast cancer subpopulation with high risk of internal mammary lymph nodes metastasis: analysis of 2,269 Chinese breast cancer patients treated with extended radical mastectomy. Breast Cancer Res Treat. 2008; 107:379–387.
Article10. Veronesi U, Cascinelli N, Bufalino R, Morabito A, Greco M, Galluzzo D, et al. Risk of internal mammary lymph node metastases and its relevance on prognosis of breast cancer patients. Ann Surg. 1983; 198:681–684.
Article11. Shahar KH, Buchholz TA, Delpassand E, Sahin AA, Ross MI, Ames FC, et al. Lower and central tumor location correlates with lymphoscintigraphy drainage to the internal mammary lymph nodes in breast carcinoma. Cancer. 2005; 103:1323–1329.
Article12. Kong AL, Tereffe W, Hunt KK, Yi M, Kang T, Weatherspoon K, et al. Impact of internal mammary lymph node drainage identified by preoperative lymphoscintigraphy on outcomes in patients with stage I to III breast cancer. Cancer. 2012; 118:6287–6296.
Article13. Chen RC, Lin NU, Golshan M, Harris JR, Bellon JR. Internal mammary nodes in breast cancer: diagnosis and implications for patient management. A systematic review. J Clin Oncol. 2008; 26:4981–4989.
Article14. Chang JS, Park W, Kim YB, Lee IJ, Keum KC, Lee CG, et al. Long-term survival outcomes following internal mammary node irradiation in stage II-III breast cancer: results of a large retrospective study with 12-year follow-up. Int J Radiat Oncol Biol Phys. 2013; 86:867–872.
Article15. Fowble B, Hanlon A, Freedman G, Nicolaou N, Hoffman J, Sigurdson E, et al. Internal mammary node irradiation neither decreases distant metastases nor improves survival in stage I and II breast cancer. Int J Radiat Oncol Biol Phys. 2000; 47:883–894.
Article16. Stemmer SM, Rizel S, Hardan I, Adamo A, Neumann A, Goffman J, et al. The role of irradiation of the internal mammary lymph nodes in high-risk stage II to IIIA breast cancer patients after high-dose chemotherapy: a prospective sequential nonrandomized study. J Clin Oncol. 2003; 21:2713–2718.
Article17. Veronesi U, Valagussa P. Inefficacy of internal mammary nodes dissection in breast cancer surgery. Cancer. 1981; 47:170–175.
Article18. Olson RA, Woods R, Speers C, Lau J, Lo A, Truong PT, et al. Does the intent to irradiate the internal mammary nodes impact survival in women with breast cancer? A population-based analysis in British Columbia. Int J Radiat Oncol Biol Phys. 2012; 83:e35–e41.19. Obedian E, Haffty BG. Internal mammary nodal irradiation in conservatively-managed breast cancer patients: is there a benefit? Int J Radiat Oncol Biol Phys. 1999; 44:997–1003.
Article20. Lê MG, Arriagada R, de Vathaire F, Dewar J, Fontaine F, Lacour J, et al. Can internal mammary chain treatment decrease the risk of death for patients with medial breast cancers and positive axillary lymph nodes? Cancer. 1990; 66:2313–2318.
Article21. Arriagada R, Rutqvist LE, Mattsson A, Kramar A, Rotstein S. Adequate locoregional treatment for early breast cancer may prevent secondary dissemination. J Clin Oncol. 1995; 13:2869–2878.
Article22. Cuzick J, Stewart H, Rutqvist L, Houghton J, Edwards R, Redmond C, et al. Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol. 1994; 12:447–453.
Article23. Hennequin C, Bossard N, Servagi-Vernat S, Maingon P, Dubois JB, Datchary J, et al. Ten-year survival results of a randomized trial of irradiation of internal mammary nodes after mastectomy. Int J Radiat Oncol Biol Phys. 2013; 86:860–866.
Article24. Lacour J, Le M, Caceres E, Koszarowski T, Veronesi U, Hill C. Radical mastectomy versus radical mastectomy plus internal mammary dissection. Ten year results of an international cooperative trial in breast cancer. Cancer. 1983; 51:1941–1943.
Article25. Poortmans P. Irradiation of the internal mammary and medial supraclavicular lymph nodes in stage I to III breast cancer: 10 years results of the EORTC Radiation Oncology and Breast Cancer Groups phase III trial 22922/10925. In : The European Cancer Congress; 2013. p. Abstract BA 2.26. Paszat LF, Vallis KA, Benk VM, Groome PA, Mackillop WJ, Wielgosz A. A population-based case-cohort study of the risk of myocardial infarction following radiation therapy for breast cancer. Radiother Oncol. 2007; 82:294–300.
Article27. Darby SC, McGale P, Taylor CW, Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 2005; 6:557–565.
Article28. Giordano SH, Kuo YF, Freeman JL, Buchholz TA, Hortobagyi GN, Goodwin JS. Risk of cardiac death after adjuvant radiotherapy for breast cancer. J Natl Cancer Inst. 2005; 97:419–424.
Article29. Patt DA, Goodwin JS, Kuo YF, Freeman JL, Zhang DD, Buchholz TA, et al. Cardiac morbidity of adjuvant radiotherapy for breast cancer. J Clin Oncol. 2005; 23:7475–7482.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circulating Tumor Cells Detected by RT-PCR for CK-20 before Surgery Indicate Worse Prognostic Impact in Triple-Negative and HER2 Subtype Breast Cancer
- Somatic Mutations of TP53 and Prognostic Factors for Primary Operable Breast Cancer: Correspondence
- Surgical Treatment of Locoregional Recurrence in Breast Cancer
- Prognostic Significance of Immunohistochemical Expression of p53 Gene Product in Operable Breast Cancer
- High Expression of NRF2 and Low Expression of KEAP1 Predict Worse Survival in Patients With Operable Triple-Negative Breast Cancer