J Bone Metab.
2013 Nov;20(2):75-81. 10.11005/jbm.2013.20.2.75.
Changes of Paraspinal Muscles in Postmenopausal Osteoporotic Spinal Compression Fractures: Magnetic Resonance Imaging Study
- Affiliations
-
- 1Department of Orthopedic Surgery, School of Medicine, Wonkwang University Hospital, Iksan, Korea. oschae68@hanmail.net
- 2Department of Radiology, School of Medicine, Wonkwang University Hospital, Iksan, Korea.
- KMID: 2286297
- DOI: http://doi.org/10.11005/jbm.2013.20.2.75
Abstract
- BACKGROUND
To investigate the changes of cross sectional area (CSA) in paraspinal muscles upon magnetic resonance imaging (MRI) and bone mineral density (BMD) in postmenopausal osteoporotic spinal compression fractures.
METHODS
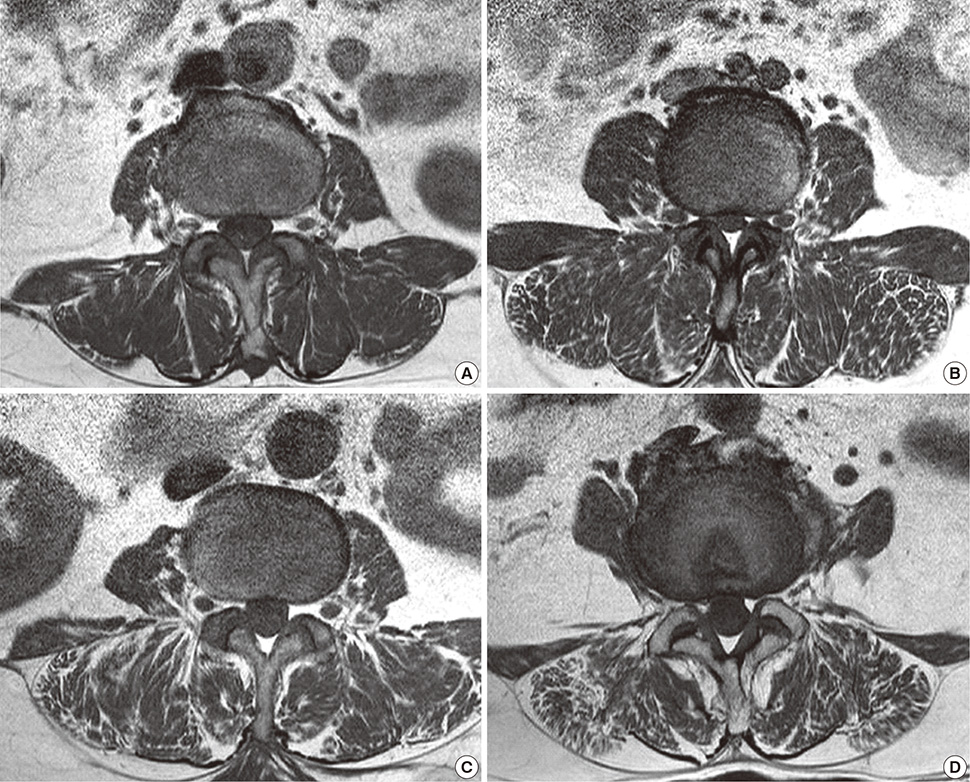
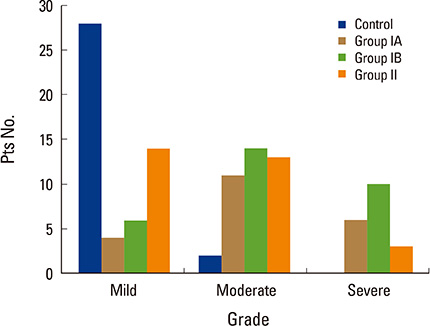
We reviewed 81 postmenopausal women with osteoporosis, who had underwent MRI examination. The patients were divided into 51 patients who had osteoporotic spinal compression fractures (group I), and 30 patients who without fractures (group II). Group I were subdivided into IA and IB, based on whether they were younger (IA) of older (IB) than 70 years of age. We additionally measured body mass index and BMD. The CSA of multifidus, erector spinae, paraspinal muscles, psoas major (PT), and intervertebral (IV) discs were measured. The degree of fatty atrophy was estimated using three grades.
RESULTS
The BMD and T-score of group I were significantly lower than those of group II. The CSA of erector spinae, paraspinal muscles, and PT in the group I was significantly smaller than that of group II. The CSA of paraspinal muscles in group IB were significantly smaller than those of group IA. The CSA of erector spinae, mutifidus, and PT in group IB were smaller than those of group IA, but the difference was not statistically significant. Group 1 exhibited greater fat infiltration in the paraspinal muscle than group II.
CONCLUSIONS
Postmenopausal osteoporotic spinal compression fracture is associated with profound changes of the lumbar paraspinal muscle, reduction of CSA, increased CSA of IV disc, and increased intramuscular fat infiltration.
MeSH Terms
Figure
Reference
-
1. American Society of Clinical Nutrition. Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989; 50:1121–1235.2. Bayramoğlu M, Sözay S, Karataş M, et al. Relationships between muscle strength and bone mineral density of three body regions in sedentary postmenopausal women. Rheumatol Int. 2005; 25:513–517.
Article3. Riggs BL, Wahner HW, Melton LJ 3rd, et al. Rates of bone loss in the appendicular and axial skeletons of women. Evidence of substantial vertebral bone loss before menopause. J Clin Invest. 1986; 77:1487–1491.
Article4. Grimby G, Saltin B. The ageing muscle. Clin Physiol. 1983; 3:209–218.
Article5. Cruz-Jentoft AJ, Landi F, Topinková E, et al. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care. 2010; 13:1–7.
Article6. Cederholm T, Cruz-Jentoft AJ, Maggi S. Sarcopenia and fragility fractures. Eur J Phys Rehabil Med. 2013; 49:111–117.7. Kim TN, Choi KM. Sarcopenia: definition, epidemiology, and pathophysiology. J Bone Metab. 2013; 20:1–10.
Article8. Sinaki M, Khosla S, Limburg PJ, et al. Muscle strength in osteoporotic versus normal women. Osteoporos Int. 1993; 3:8–12.
Article9. Cunha-Henriques S, Costa-Paiva L, Pinto-Neto AM, et al. Postmenopausal women with osteoporosis and musculoskeletal status: a comparative cross-sectional study. J Clin Med Res. 2011; 3:168–176.
Article10. Miyakoshi N, Hongo M, Maekawa S, et al. Factors related to spinal mobility in patients with postmenopausal osteoporosis. Osteoporos Int. 2005; 16:1871–1874.
Article11. Balzini L, Vannucchi L, Benvenuti F, et al. Clinical characteristics of flexed posture in elderly women. J Am Geriatr Soc. 2003; 51:1419–1426.
Article12. Keller TS, Harrison DE, Colloca CJ, et al. Prediction of osteoporotic spinal deformity. Spine (Phila Pa 1976). 2003; 28:455–462.
Article13. Pahor M, Manini T, Cesari M. Sarcopenia: clinical evaluation, biological markers and other evaluation tools. J Nutr Health Aging. 2009; 13:724–728.
Article14. Cesari M, Leeuwenburgh C, Lauretani F, et al. Frailty syndrome and skeletal muscle: results from the Invecchiare in Chianti study. Am J Clin Nutr. 2006; 83:1142–1148.
Article15. Maughan RJ. Relationship between muscle strength and muscle cross-sectional area. Implications for training. Sports Med. 1984; 1:263–269.16. Jorgensen MJ, Marras WS, Gupta P. Cross-sectional area of the lumbar back muscles as a function of torso flexion. Clin Biomech (Bristol, Avon). 2003; 18:280–286.
Article17. Chaffin DB, Redfern MS, Erig M, et al. Lumbar muscle size and locations from CT scans of 96 women of age 40 to 63 years. Clin Biomech (Bristol, Avon). 1990; 5:9–16.
Article18. Ropponen A, Videman T, Battié MC. The reliability of paraspinal muscles composition measurements using routine spine MRI and their association with back function. Man Ther. 2008; 13:349–356.
Article19. Kang CH, Shin MJ, Kim SM, et al. MRI of paraspinal muscles in lumbar degenerative kyphosis patients and control patients with chronic low back pain. Clin Radiol. 2007; 62:479–486.
Article20. Lee HJ, Lim WH, Park JW, et al. The relationship between cross sectional area and strength of back muscles in patients with chronic low back pain. Ann Rehabil Med. 2012; 36:173–181.
Article21. Mengiardi B, Schmid MR, Boos N, et al. Fat content of lumbar paraspinal muscles in patients with chronic low back pain and in asymptomatic volunteers: quantification with MR spectroscopy. Radiology. 2006; 240:786–792.
Article22. Sinaki M, Wollan PC, Scott RW, et al. Can strong back extensors prevent vertebral fractures in women with osteoporosis? Mayo Clin Proc. 1996; 71:951–956.
Article23. McGill SM. A myoelectrically based dynamic three-dimensional model to predict loads on lumbar spine tissues during lateral bending. J Biomech. 1992; 25:395–414.
Article24. Briggs AM, Wrigley TV, van Dieën JH, et al. The effect of osteoporotic vertebral fracture on predicted spinal loads in vivo. Eur Spine J. 2006; 15:1785–1795.
Article25. Crepaldi G, Romanato G, Tonin P, et al. Osteoporosis and body composition. J Endocrinol Invest. 2007; 30:42–47.26. Buehring B, Krueger D, Binkley N. Effect of including historical height and radius BMD measurement on sarco-osteoporosis prevalence. J Cachexia Sarcopenia Muscle. 2013; 4:47–54.
Article27. Verschueren S, Gielen E, O'Neill TW. Sarcopenia and its relationship with bone mineral density in middle-aged and elderly European men. Osteoporos Int. 2013; 24:87–98.
Article28. Miyakoshi N, Hongo M, Mizutani Y, et al. Prevalence of sarcopenia in Japanese women with osteopenia and osteoporosis. J Bone Miner Metab. 2013; 31:556–561.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Epidemiology and Importance of Osteoporotic Spinal Compression Fracture in South Korea
- Lordoplasty: An Alternative Technique for the Treatment of Osteoporotic Compression Fracture
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture
- Magnetic Resonance Enhancement Patterns at the Different Ages of Symptomatic Osteoporotic Vertebral Compression Fractures
- Osteoporotic Compression Fracture of the Thoracolumbar Spine and Sacral Insufficiency Fracture: Incidence and Analysis of the Relationship according to the Clinical Factors