Intest Res.
2015 Apr;13(2):135-144. 10.5217/ir.2015.13.2.135.
The Clinical Usefulness of Endoscopic Ultrasound-Guided Fine Needle Aspiration and Biopsy for Rectal and Perirectal Lesions
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jsbyeon@amc.seoul.kr
- KMID: 2284880
- DOI: http://doi.org/10.5217/ir.2015.13.2.135
Abstract
- BACKGROUND/AIMS
Endoscopic ultrasound-guided fine needle aspiration and/or biopsy (EUS-FNA/B) have been used to diagnose subepithelial tumors (SETs) and extraluminal lesions in the gastrointestinal tract. Our group previously reported the usefulness of EUS-FNA/B for rectal and perirectal lesions. This study reports our expanded experience with EUS-FNA/B for rectal and perirectal lesions in terms of diagnostic accuracy and safety. We also included our new experience with EUS-FNB using the recently introduced ProCore needle.
METHODS
From April 2009 to March 2014, EUS-FNA/B for rectal and perirectal lesions was performed in 30 consecutive patients. We evaluated EUS-FNA/B performance by comparing histological diagnoses with final results. We also investigated factors affecting diagnostic accuracy.
RESULTS
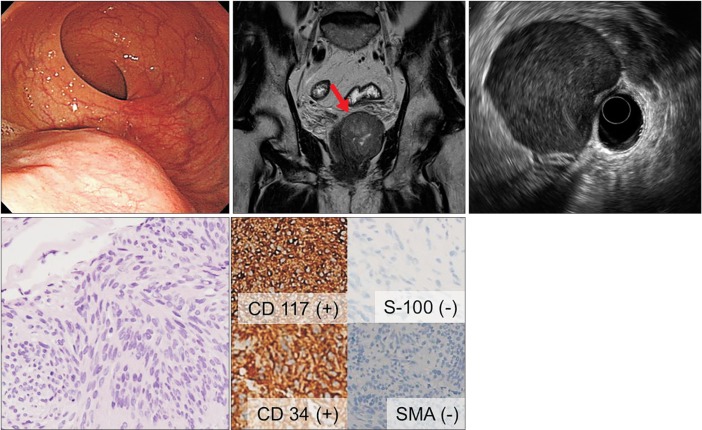
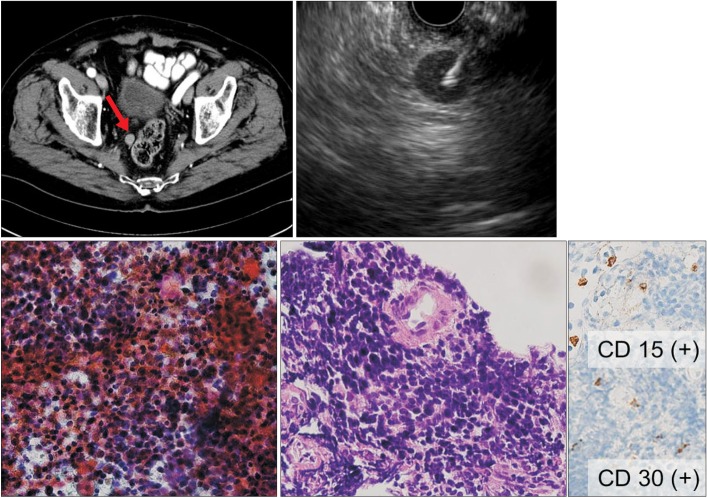
Among 10 patients with SETs, EUS-FNA/B specimen results revealed a gastrointestinal stromal tumor in 4 patients and malignant lymphoma in 1 patient. The diagnostic accuracy of EUS-FNA/B was 50% for SETs (5/10). Among 20 patients with non-SET lesions, 8 patients were diagnosed with malignant disease and 7 were diagnosed with benign disease based on both EUS-FNA/B and the final results. The diagnostic accuracy of EUS-FNA/B for non-SET lesions was 75% (15/20). The size of lesions was the only factor related to diagnostic accuracy (P=0.027). Two complications of mild fever and asymptomatic pneumoperitoneum occurred after EUS-FNA/B.
CONCLUSIONS
The overall diagnostic accuracy of EUS-FNA/B for rectal and perirectal lesions was 67% (20/30). EUS-FNA/B is a clinically useful method for cytological and histological diagnoses of rectal and perirectal lesions.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Application of Endoscopic Ultrasonography in the Diagnosis and Treatment of Lower Gastrointestinal Disease
Eun Young Kim
Intest Res. 2015;13(2):101-102. doi: 10.5217/ir.2015.13.2.101.
Reference
-
1. Godfrey EM, Rushbrook SM, Carroll NR. Endoscopic ultrasound: a review of current diagnostic and therapeutic applications. Postgrad Med J. 2010; 86:346–353. PMID: 20547601.
Article2. Zhu Q, Xu C, Hu D. Dose endoscopic ultrasonography impact diagnosis of intestinal diseases? Intest Res. 2011; 9:179–188.
Article3. Soetikno RM, Chang K. Endoscopic ultrasound-guided diagnosis and therapy in pancreatic disease. Gastrointest Endosc Clin N Am. 1998; 8:237–247. PMID: 9405760.4. Südhoff T, Hollerbach S, Wilhelms I, et al. Clinical utility of EUS-FNA in upper gastrointestinal and mediastinal disease. Dtsch Med Wochenschr. 2004; 129:2227–2232. PMID: 15483756.5. Hucl T, Wee E, Anuradha S, et al. Feasibility and efficiency of a new 22G core needle: a prospective comparison study. Endoscopy. 2013; 45:792–798. PMID: 24068588.
Article6. Hara K, Yamao K, Ohashi K, et al. Endoscopic ultrasonography and endoscopic ultrasound-guided fine-needle aspiration biopsy for the diagnosis of lower digestive tract disease. Endoscopy. 2003; 35:966–969. PMID: 14606022.
Article7. Sasaki Y, Niwa Y, Hirooka Y, et al. The use of endoscopic ultrasound-guided fine-needle aspiration for investigation of submucosal and extrinsic masses of the colon and rectum. Endoscopy. 2005; 37:154–160. PMID: 15692931.
Article8. Boo SJ, Byeon JS, Park do H, et al. EUS-guided fine needle aspiration and trucut needle biopsy for examination of rectal and perirectal lesions. Scand J Gastroenterol. 2011; 46:1510–1518. PMID: 21936722.
Article9. Arantes V, Logrono R, Faruqi S, Ahmed I, Waxman I, Bhutani MS. Endoscopic sonographically guided fine-needle aspiration yield in submucosal tumors of the gastrointestinal tract. J Ultrasound Med. 2004; 23:1141–1150. PMID: 15328428.10. Vander Noot MR 3rd, Eloubeidi MA, Chen VK, et al. Diagnosis of gastrointestinal tract lesions by endoscopic ultrasound-guided fine-needle aspiration biopsy. Cancer. 2004; 102:157–163. PMID: 15211474.
Article11. Hunt GC, Smith PP, Faigel DO. Yield of tissue sampling for submucosal lesions evaluated by EUS. Gastrointest Endosc. 2003; 57:68–72. PMID: 12518134.
Article12. Strand DS, Jeffus SK, Sauer BG, Wang AY, Stelow EB, Shami VM. EUS guided 22 gauge fine needle aspiration versus core biopsy needle in the evaluation of solid pancreatic neoplasms. Diagn Cytopathol. 2014; 42:751–758. PMID: 24550162.
Article13. Witt BL, Adler DG, Hilden K, Layfield LJ. A comparative needle study: EUS-FNA procedures using the HD ProCore™ and Echo-Tip® 22-gauge needle types. Diagn Cytopathol. 2013; 41:1069–1074. PMID: 23513000.
Article14. Iglesias-Garcia J, Poley JW, Larghi A, et al. Feasibility and yield of a new EUS histology needle: results from a multicenter, pooled, cohort study. Gastrointest Endosc. 2011; 73:1189–1196. PMID: 21420083.15. Kim GH, Cho YK, Kim EY, et al. Comparison of 22-gauge aspiration needle with 22-gauge biopsy needle in endoscopic ultrasonography-guided subepithelial tumor sampling. Scand J Gastroenterol. 2014; 49:347–354. PMID: 24325591.
Article16. Ginès A, Wiersema MJ, Clain JE, Pochron NL, Rajan E, Levy MJ. Prospective study of a Trucut needle for performing EUS-guided biopsy with EUS-guided FNA rescue. Gastrointest Endosc. 2005; 62:597–601. PMID: 16185976.
Article17. Storch I, Jorda M, Thurer R, et al. Advantage of EUS Trucut biopsy combined with fine-needle aspiration without immediate on-site cytopathologic examination. Gastrointest Endosc. 2006; 64:505–511. PMID: 16996340.
Article18. Eloubeidi MA, Tamhane A. Prospective assessment of diagnostic utility and complications of endoscopic ultrasound-guided fine needle aspiration. Results from a newly developed academic endoscopic ultrasound program. Dig Dis. 2008; 26:356–363. PMID: 19188728.
Article19. Thomas T, Kaye PV, Ragunath K, Aithal G. Efficacy, safety, and predictive factors for a positive yield of EUS-guided Trucut biopsy: a large tertiary referral center experience. Am J Gastroenterol. 2009; 104:584–591. PMID: 19262518.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound-Fine Needle Aspiration versus Core Biopsy for the Diagnosis of Subepithelial Tumors
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?
- The Usefulness of Ultrasound-Guided Fine Needle Aspiration in Breast Lesions
- Procore and Flexible 19 Gauge Needle Can Replace Trucut Biopsy Needle?
- How to optimize the diagnostic yield of endoscopic ultrasoundguided fine-needle sampling in solid pancreatic lesions from a technical perspective