Ewha Med J.
2013 Mar;36(1):72-76. 10.12771/emj.2013.36.1.72.
Polyuria during Sevoflurane Anesthesia for Parotidectomy Patient
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ewha Womans University School of Medicine, Seoul, Korea. 00044@ewha.ac.kr
- KMID: 2284019
- DOI: http://doi.org/10.12771/emj.2013.36.1.72
Abstract
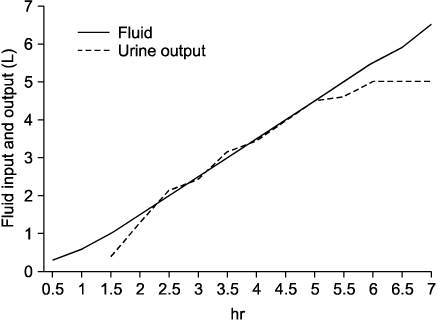
- Polyuria is occasionally observed during general anesthesia. Usually urine output during general anesthesia is decreased because of anesthetic agents. The authors came across with a case of polyruia during sevoflurane anesthesia which occurred after induction of anesthesia. Polyuria is a nonspecific symptom, but can cause many serious complications. Therefore, it is very important to investigate the cause thoroughly and treat patient appropriately.
Keyword
MeSH Terms
Figure
Reference
-
1. Im DG. The Korean Society of Anesthesiologists. Renal function monitoring. Anesthesia and pain management. 2009. 2nd ed. Korea: Koonja;980–983.2. Denker BM, Brenner BM. Kasper DL, Braunwald E, Hauser S, Longo D, Jameson JL, Fauci AS, editors. Azotemia and urinary abnormalities. Harrison's principles of internal medicine. 2004. 16th ed. New York: McGraw-Hill Professional;251.3. Teymoortash A, Lippert BM, Werner JA. Steroid hormone receptors in parotid gland cystadenolymphoma (Warthin's tumour). Clin Otolaryngol Allied Sci. 2001. 26:411–416.4. Fang ZX, Eger EI 2nd. Factors affecting the concentration of compound A resulting from the degradation of sevoflurane by soda lime and Baralyme in a standard anesthetic circuit. Anesth Analg. 1995. 81:564–568.5. Eger EI 2nd, Koblin DD, Bowland T, Ionescu P, Laster MJ, Fang Z, et al. Nephrotoxicity of sevoflurane versus desflurane anesthesia in volunteers. Anesth Analg. 1997. 84:160–168.6. Sekeroğlu MR, Kati I, Noyan T, Dülger H, Yalçinkaya AS. Alterations in the biochemical markers of renal function after sevoflurane anaesthesia. Nephrology (Carlton). 2005. 10:544–547.7. Schirle L. Polyuria with sevoflurane administration: a case report. AANA J. 2011. 79:47–50.8. Lee SY, Kim HY, Shin HW, Lee HW, Lim HJ, Yoon SM, et al. Transient polyuria during sevoflurane anesthesia: a report of two cases. Anesth Pain Med. 2006. 1:139–143.9. Morita K, Otsuka F, Ogura T, Takeuchi M, Mizobuchi S, Yamauchi T, et al. Sevoflurane anaesthesia causes a transient decrease in aquaporin-2 and impairment of urine concentration. Br J Anaesth. 1999. 83:734–739.10. Derosa G, Maffioli P. Drug safety evaluation of amlodipine. Expert Opin Drug Saf. 2011. 10:795–804.11. Derosa G, Cicero AF, Carbone A, Querci F, Fogari E, D'Angelo A, et al. Olmesartan/amlodipine combination versus olmesartan or amlodipine monotherapies on blood pressure and insulin resistance in a sample of hypertensive patients. Clin Exp Hypertens. 2012. 09. 06. [Epub]. http://dx.doi.org/10.3109/10641963.2012.721841.12. Colson P, Saussine M, Séguin JR, Cuchet D, Chaptal PA, Roquefeuil B. Hemodynamic effects of anesthesia in patients chronically treated with angiotensin-converting enzyme inhibitors. Anesth Analg. 1992. 74:805–808.13. Fraser CL, Arieff AI. Fatal central diabetes mellitus and insipidus resulting from untreated hyponatremia: a new syndrome. Ann Intern Med. 1990. 112:113–119.14. Robertson GL. Kasper DL, Braunwald E, Hauser S, Longo D, Jameson JL, Fauci AS, editors. Disorders of the neurohypophysis. Harrison's principles of internal medicine. 2004. 16th ed. New York: McGraw-Hill Professional;2098–2099.15. D'Orio V, el Allaf D, Juchmès J, Marcelle R. The use of low doses of dopamine in intensive care medicine. Arch Int Physiol Biochim. 1984. 92:S11–S20.16. McDonald RH Jr, Goldberg LI, McNay JL, Tuttle EP Jr. Effects of dopamine in man: augmentation of sodium excretion, glomerular filtration rate, and renal plasma flow. J Clin Invest. 1964. 43:1116–1124.17. Debaveye YA, Van den Berghe GH. Is there still a place for dopamine in the modern intensive care unit? Anesth Analg. 2004. 98:461–468.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transient Polyuria during SevofluraneAnesthesia : A report of two cases
- Effect of Nitrous Oxide on Bispectral Index during Sevoflurane Anesthesia
- Case Report of Sevoflurane Anesthesia in Healthy Patient
- Comparison of plasma inorganic fluoride concentration with sevoflurane-N2O and enflurane-N2O anesthesia
- Postoperative Nausea and Vomiting after Strabismus Surgery in Pediatrics: A Comparison between VIMA with Sevoflurane and TIVA with Propofol