Endocrinol Metab.
2012 Sep;27(3):222-226. 10.3803/EnM.2012.27.3.222.
A Case of Actinomycotic Thyroiditis in an Adult with Piriform Sinus Fistula
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. pons71@hanmail.net
- 2Kim Yong Ki Internal Medicine Clinic, Busan, Korea.
- KMID: 2282406
- DOI: http://doi.org/10.3803/EnM.2012.27.3.222
Abstract
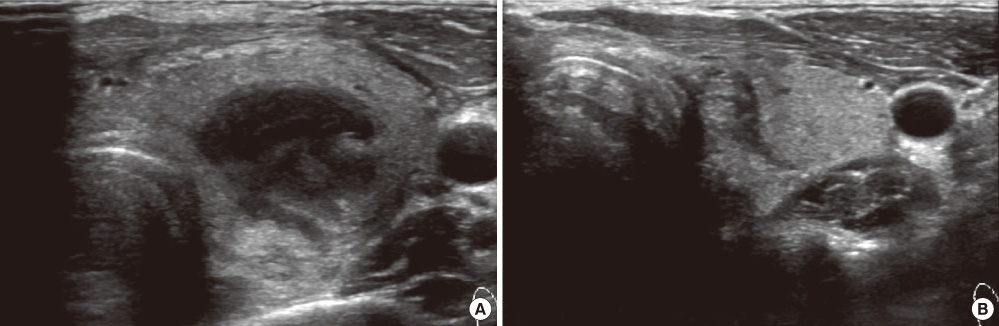
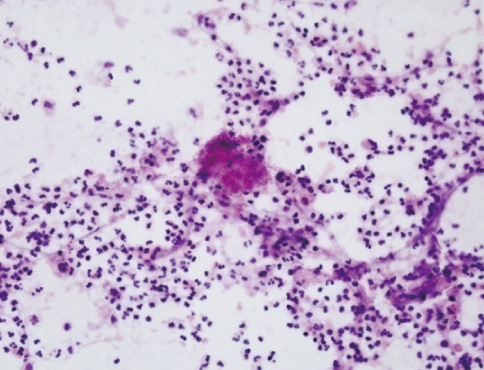
- Acute suppurative thyroiditis is an uncommon infectious thyroid disease affecting mainly children and young adults. The route of infection is frequently a pyriform sinus fistula. The major pathogens responsible for acute bacterial suppurative thyroiditis are the Streptococcus and Staphylococcus species. In contrast, Actinomyces species are a very rare cause of acute suppurative thyroiditis. We experienced a case of a 23-year-old man who has presented general weakness and neck pain. Thyroid ultrasonography showed an ill-defined area of heterogeneous hypoechogenicity in the left lobe of the thyroid gland. Histologic examination by fine needle aspiration demonstrated gram-positive, filamentous-like organisms with branching hyphae and characteristic sulfur granules. Barium esophagogram showed a linear barium-filled track at the left pyriform sinus. We report a case of actinomycotic thyroiditis in a young adult with pyriform sinus fistula along with a brief review of related literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Berger SA, Zonszein J, Villamena P, Mittman N. Infectious diseases of the thyroid gland. Rev Infect Dis. 1983. 5:108–122.2. Takai SI, Miyauchi A, Matsuzuka F, Kuma K, Kosaki G. Internal fistula as a route of infection in acute suppurative thyroiditis. Lancet. 1979. 1:751–752.3. Godin MS, Kearns DB, Pransky SM, Seid AB, Wilson DB. Fourth branchial pouch sinus: principles of diagnosis and management. Laryngoscope. 1990. 100:174–178.4. Brook I. Microbiology and management of acute suppurative thyroiditis in children. Int J Pediatr Otorhinolaryngol. 2003. 67:447–451.5. Kim MK, Sun BH. Clinical analysis of actinomycosis: 66 cases of Korean experience. J Korean Surg Soc. 1997. 52:702–710.6. Hwang HP, Lee MR, Kim JH. Pelvic actinomycosis: is it possible to diagnose preoperatively? J Korean Soc Coloproctol. 2007. 23:437–440.7. Burge D, Middleton A. Persistent pharyngeal pouch derivatives in the neonate. J Pediatr Surg. 1983. 18:230–234.8. Roediger WE, Kalk F, Spitz L, Schmaman A. Congenital thyroid cyst of ultimobranchial gland origin. J Pediatr Surg. 1977. 12:575–576.9. Park SW, Han MH, Sung MH, Kim IO, Kim KH, Chang KH, Han MC. Neck infection associated with pyriform sinus fistula: imaging findings. AJNR Am J Neuroradiol. 2000. 21:817–822.10. Mali VP, Prabhakaran K. Recurrent acute thyroid swellings because of pyriform sinus fistula. J Pediatr Surg. 2008. 43:e27–e30.11. Hillel AD, Schwartz AN. Trumpet maneuver for visual and CT examination of the pyriform sinus and retrocricoid area. Head Neck. 1989. 11:231–236.12. Van Dellen JR. Actinomycosis: an ancient disease difficult to diagnose. World Neurosurg. 2010. 74:263–264.13. Hong SG, Jin SH, Ko BG, Park DC, Cho JT, Lee JK. Primary actinomycosis of the thyroid. Korean J Intern Med. 1986. 31:821–826.14. Custal-Teixidor M, Trull-Gimbernat JM, Garijo-López G, Valldosera-Rosello M. Fine-needle aspiration cytology in the diagnosis of cervicofacial actinomycosis: report of 15 cases. Med Oral Patol Oral Cir Bucal. 2004. 9:467–470. 464–467.15. Japanese Society of Chemotherapy Committee on guidelines for treatment of anaerobic infections. Japanese Association for Anaerobic Infection Research. Chapter 2-12-1. Anaerobic infections (individual fields): actinomycosis. J Infect Chemother. 2011. 17:Suppl 1. 119–120.16. Kim KH, Sung MW, Lee KJ, Roh JL, Kwon TK, Kim IS, Jin JW. Management of pyriform sinus fistula with chemocauterization. Korean J Otolaryngol-Head Neck Surg. 2002. 45:906–910.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Acute Suppurative Thyroiditis due to Piriform Sinus Fistula
- A Case of Piriform Sinus Fistula Complicated with Suppurative Thyroiditis Treated with Chemocauterization Using Trichloroacetic Acid
- Acute suppurative thyroiditis associated with piriform sinus fistula
- A Child of Acute Suppurative Thyroiditis with Transient Thyrotoxicosis
- Acute Suppurative Thyroiditis Caused by Methicillin - Resistant Staphylococcus Aureus in Healthy Children