Diabetes Metab J.
2012 Apr;36(2):151-156. 10.4093/dmj.2012.36.2.151.
Impact of HbA1c Criterion on the Detection of Subjects with Increased Risk for Diabetes among Health Check-Up Recipients in Korea
- Affiliations
-
- 1Health Screening and Promotion Center, Asan Medical Center, Seoul, Korea. hkkim0801@amc.seoul.kr
- KMID: 2281418
- DOI: http://doi.org/10.4093/dmj.2012.36.2.151
Abstract
- BACKGROUND
We performed the study to examine the impact of hemoglobin A1c (HbA1c) criterion on the screening of increased risk for diabetes among health check-up subjects in Korea.
METHODS
We retrospectively analyzed clinical and laboratory data of 37,754 Korean adults (age, 20 to 89 years; 41% women) which were measured during regular health check-ups. After excluding subjects with previously diagnosed diabetes mellitus (n=1,812) and with overt anemia (n=318), 35,624 subjects (21,201 men and 14,423 women) were included in the analysis.
RESULTS
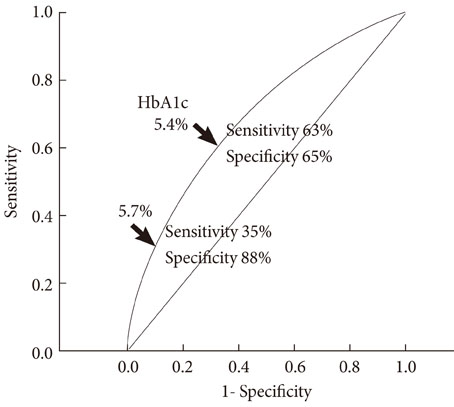
Among the 35,624 subjects, 11,316 (31.8%) subjects were categorized as increased risk for diabetes (IRD) by fasting plasma glucose (FPG) criteria, 6,531 (18.1%) subjects by HbA1c criteria, and 13,556 (38.1%) subjects by combined criteria. Therefore, although HbA1c criteria alone identifies 42% [(11,316-6,531)/11,316] fewer subjects with IRD than does FPG criteria, about 20% [(13,556-11,316)/11,316] more subjects could be detected by including new HbA1c criteria in addition to FPG criteria. Among the 13,556 subjects with IRD, 7,025 (51.8%) met FPG criteria only, 2,240 (16.5%) met HbA1c criteria only, and 4,291 (31.7%) met both criteria. Among subjects with impaired fasting glucose, 65% were normal, 32% were IRD, and 3% were diabetes by HbA1c criterion. In receiver operating characteristic curve analysis, cutoff point of HbA1c with optimal sensitivity and specificity for identifying IRD was 5.4%.
CONCLUSION
Although HbA1c criteria alone identifies fewer subjects with IRD than does FPG criteria, about 20% more could be detected by addition of HbA1c criteria. Further studies are needed to define optimal cutoff point of HbA1c and to establish screening and management guidelines for IRD.
MeSH Terms
Figure
Reference
-
1. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010. 33:Suppl 1. S62–S69.2. Mann DM, Carson AP, Shimbo D, Fonseca V, Fox CS, Muntner P. Impact of A1C screening criterion on the diagnosis of pre-diabetes among U.S. adults. Diabetes Care. 2010. 33:2190–2195.3. Cowie CC, Rust KF, Byrd-Holt DD, Gregg EW, Ford ES, Geiss LS, Bainbridge KE, Fradkin JE. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care. 2010. 33:562–568.4. Herman WH, Ma Y, Uwaifo G, Haffner S, Kahn SE, Horton ES, Lachin JM, Montez MG, Brenneman T, Barrett-Connor E. Diabetes Prevention Program Research Group. Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program. Diabetes Care. 2007. 30:2453–2457.5. Christensen DL, Witte DR, Kaduka L, Jorgensen ME, Borch-Johnsen K, Mohan V, Shaw JE, Tabak AG, Vistisen D. Moving to an A1C-based diagnosis of diabetes has a different impact on prevalence in different ethnic groups. Diabetes Care. 2010. 33:580–582.6. Likhari T, Gama R. Glycaemia-independent ethnic differences in HbA(1c) in subjects with impaired glucose tolerance. Diabet Med. 2009. 26:1068–1069.7. Saha S, Gerdtham UG, Johansson P. Economic evaluation of lifestyle interventions for preventing diabetes and cardiovascular diseases. Int J Environ Res Public Health. 2010. 7:3150–3195.8. Pani LN, Korenda L, Meigs JB, Driver C, Chamany S, Fox CS, Sullivan L, D'Agostino RB, Nathan DM. Effect of aging on A1C levels in individuals without diabetes: evidence from the Framingham Offspring Study and the National Health and Nutrition Examination Survey 2001-2004. Diabetes Care. 2008. 31:1991–1996.9. Rhee MK, Ziemer DC, Kolm P, Phillips LS. Postchallenge glucose rises with increasing age even when glucose tolerance is normal. Diabet Med. 2006. 23:1174–1179.10. International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009. 32:1327–1334.11. Edelman D, Olsen MK, Dudley TK, Harris AC, Oddone EZ. Utility of hemoglobin A1c in predicting diabetes risk. J Gen Intern Med. 2004. 19:1175–1180.12. Pradhan AD, Rifai N, Buring JE, Ridker PM. Hemoglobin A1c predicts diabetes but not cardiovascular disease in nondiabetic women. Am J Med. 2007. 120:720–727.13. Sato KK, Hayashi T, Harita N, Yoneda T, Nakamura Y, Endo G, Kambe H. Combined measurement of fasting plasma glucose and A1C is effective for the prediction of type 2 diabetes: the Kansai Healthcare Study. Diabetes Care. 2009. 32:644–646.14. Kim KS, Kim SK, Lee YK, Park SW, Cho YW. Diagnostic value of glycated haemoglobin HbA(1c) for the early detection of diabetes in high-risk subjects. Diabet Med. 2008. 25:997–1000.15. Bae JC, Rhee EJ, Choi ES, Kim JH, Kim WJ, Yoo SH, Park SE, Park CY, Lee WY, Oh KW, Park SW, Kim SW. The cutoff value of HbA1c in predicting diabetes in Korean adults in a university hospital in Seoul. Korean Diabetes J. 2009. 33:503–510.16. Lee YS, Moon SS. The use of HbA1c for diagnosis of type 2 diabetes in Korea. Korean J Med. 2011. 80:291–297.17. Lee CH, Chang WJ, Chung HH, Kim HJ, Park SH, Moon JS, Lee JE, Yoon JS, Chun KA, Won KC, Cho IH, Lee HW. The combination of fasting plasma glucose and glycosylated hemoglobin as a predictor for type 2 diabetes in Korean adults. Korean Diabetes J. 2009. 33:306–314.18. Kim CH, Kim HK, Bae SJ, Park JY, Lee KU. Discordance between fasting glucose-based and hemoglobin A1c-based diagnosis of diabetes mellitus in Koreans. Diabetes Res Clin Pract. 2011. 91:e8–e10.19. El-Agouza I, Abu Shahla A, Sirdah M. The effect of iron deficiency anaemia on the levels of haemoglobin subtypes: possible consequences for clinical diagnosis. Clin Lab Haematol. 2002. 24:285–289.20. Coban E, Ozdogan M, Timuragaoglu A. Effect of iron deficiency anemia on the levels of hemoglobin A1c in nondiabetic patients. Acta Haematol. 2004. 112:126–128.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Response: Impact of HbA1c Criterion on the Detection of Subjects with Increased Risk for Diabetes among Health Check-Up Recipients in Korea (Diabetes Metab J 2012;36:151-6)
- Letter: Impact of HbA1c Criterion on the Detection of Subjects with Increased Risk for Diabetes among Health Check-Up Recipients in Korea (Diabetes Metab J 2012;36:151-6)
- Usefulness of Glycated Hemoglobin as Diagnostic Criteria for Metabolic Syndrome
- The Utility of HbA1c as a Diagnostic Criterion of Diabetes
- The Use of HbA1c for Diagnosis of Type 2 Diabetes in Korea