Clin Exp Otorhinolaryngol.
2008 Dec;1(4):201-205.
Management for the Children with Otitis Media with Effusion in the Tertiary Hospital
- Affiliations
-
- 1Department of Otolaryngology, Ajou University School of Medicine, Suwon, Korea. yhc@ajou.ac.kr
- 2Department of Otolaryngology, Ewha Womans University College of Medicine, Seoul, Korea.
Abstract
OBJECTIVES
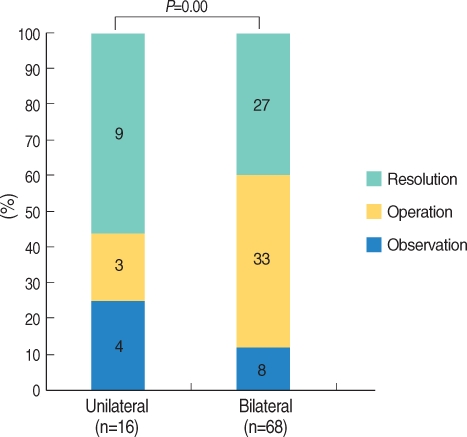
Recently, new evidence-based recommendations have been introduced for diagnosing and managing otitis media with effusion (OME) in children. However, there are some difficulties to follow the general guidelines in the tertiary hospitals. The purpose is to evaluate the efficiency of antibiotics or antihistamines for treatment of children with OME in the tertiary hospital with a randomized prospective clinical study. METHODS: Eighty-four children with OME who had been diagnosed in the tertiary hospital were randomized to receive 5 different medications for 2 weeks. We prescribed antibiotics (amoxicillin-clavulanate syrup) in Group I (n=16), antibiotics/steroids (prednisolone) in Group II (n=18), antibiotics/antihistamines (ebastine) in Group III (n=15), antibiotics/steroids/antihistamines in Group IV (n=17), and mucolytics (ivy leaf extract) in Group V (n=17) for control. We followed-up children every 2 weeks and evaluated the state of OME at 3 months. RESULTS: Thirty six (42.9%) of 84 children were resolved within average 6.9 weeks after the treatments. Thirty-six (42.9%) were treated with ventilation tube insertion and 12 patients (14.3%) were observed. There was no difference in the resolution rates of OME among the five different protocols (P>0.05). There was no difference in the resolution rates among groups who used steroids, antihistamines, steroids and antihistamines, or other medications to manage 42 children with allergies (P>0.05). CONCLUSION: In the tertiary hospital, the cure rate of children with OME was not as high as well-known, and antibiotics or anti-allergic medications were not more effective than control. We may, therefore, need any other guidelines which are different from the previous evidence-based recommendations, including early operation in the tertiary hospitals.
MeSH Terms
Figure
Reference
-
1. Tos M. Epidemiology and natural history of secretory otitis. Am J Otol. 1984; 10. 5(6):459–462. PMID: 6542752.2. Casselbrant ML, Mandel EM. Rosenfeld RM, Bluestone CD, editors. Epidemiology. Evidence-based otitis media. 2003. 2nd ed. Hamilton: BC Decker Inc;p. 147–162.3. Shekelle P, Takata G, Chan LS, Mangione-Smith R, Corley PM, Morphew T, et al. Diagnosis, natural history, and late effects of otitis media with effusion. Evid Rep Technol Assess (Summ). 2002; 6. (55):1–5. PMID: 12945555.4. Bluestone CD. Studies in otitis media: Children's Hospital of Pittsburgh-University of Pittsburgh progress report-2004. Laryngoscope. 2004; 11. 114(11 Pt 3):Suppl 105. 1–26. PMID: 15514559.
Article5. Döner F, Yariktas M, Demirci M. The role of allergy in recurrent otitis media with effusion. J Investig Allergol Clin Immunol. 2004; 14(2):154–158.6. Griffin GH, Flynn C, Bailey RE, Schultz JK. Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst Rev. 2006; 10. (4):CD003423. PMID: 17054169.
Article7. Mandel EM, Casselbrant ML. Recent developments in the treatment of otitis media with effusion. Drugs. 2006; 12. 66(12):1565–1576. PMID: 16956304.
Article8. Stool SE, Berg AO, Berman S, Cooley JR, Culpepper L, Eavey RD, et al. Otitis media with effusion in young children (Clinical Practice Guideline, Number 12). 1994. Rockville, MD: US Department of Health and Human Services;AHCPR Publication No. 94-0622.9. Rosenfeld RM, Culpepper L, Doyle KJ, Grundfast KM, Hoberman A, Kenna MA, et al. Clinical practice guideline: otitis media with effusion. Otolaryngol Head Neck Surg. 2004; 5. 130(5 Suppl):S95–S118. PMID: 15138413.
Article10. Poetker DM, Ubell ML, Kerschner JE. Disease severity in patients referred to pediatric otolaryngologists with a diagnosis of otitis media. Int J Pediatr Otorhinolaryngol. 2006; 2. 70(2):311–317. PMID: 16125250.
Article11. Kenna MA. Otitis media and the new guidelines. J Otolaryngol. 2005; 6. 34(Suppl 1):S24–S32. PMID: 16089237.12. McIsaac WJ, Coyte P, Croxford R, Harji S, Feldman W. Referral of children with otitis media. Do family physicians and pediatricians agree? Can Fam Physician. 2000; 9. 46:1780–1782. 1785–1788. PMID: 11013797.13. Teele DW, Klein JO, Rosner BA. Epidemiology of otitis media in children. Ann Otol Rhinol Laryngol Suppl. 1980; May–Jun. 89(3 Pt 2):5–6. PMID: 6778349.
Article14. Williamson IG, Dunleavey J, Bain J, Robinson D. The natural history of otitis media with effusion-a three-year study of the incidence and prevalence of abnormal tympanograms in four South West Hampshire infant and first schools. J Laryngol Otol. 1994; 11. 108(11):930–934. PMID: 7829943.15. Pichichero ME, Marsocci SM, Murphy ML, Hoeger W, Francis AB, Green JL. A prospective observational study of 5-, 7-, and 10-day antibiotic treatment for acute otitis media. Otolaryngol Head Neck Surg. 2001; 4. 124(4):381–387. PMID: 11283494.
Article16. Pessey JJ, Gehanno P, Thoroddsen E, Dagan R, Leibovitz E, Machac J, et al. Short course therapy with cefuroxime axetil for acute otitis media: results of a randomized multicenter comparison with amoxicillin/clavulanate. Pediatr Infect Dis J. 1999; 10. 18(10):854–859. PMID: 10530579.
Article17. Renko M, Kontiokari T, Jounio-Ervasti K, Rantala H, Uhari M. Disappearance of middle ear effusion in acute otitis media monitored daily with tympanometry. Acta Paediatr. 2006; 3. 95(3):359–363. PMID: 16497649.
Article18. Rovers MM, Glasziou P, Appelman CL, Burke P, McCormick DP, Damoiseaux RA, et al. Predictors of pain and/or fever at 3 to 7 days for children with acute otitis media not treated initially with antibiotics: a metaanalysis of individual patient data. Pediatrics. 2007; 3. 119(3):579–585. PMID: 17332211.
Article19. Berman S, Roark R. Factors influencing outcome in children treated with antibiotics for acute otitis media. Pediatr Infect Dis J. 1993; 1. 12(1):20–24. PMID: 8417420.
Article20. Claessen JQ, Appelman CL, Touw-Otten FW, de Melker RA, Hordijk GJ. Persistence of middle ear dysfunction after recurrent acute otitis media. Clin Otolaryngol Allied Sci. 1994; 2. 19(1):35–40. PMID: 8174299.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Middle ear histopathology in children with otitis media with effusion
- Diagnosis and Management of Acute Otitis Media and Otitis Media With Effusion
- Management of Otitis Media in Children
- Experimental otitis media with effusion induced by lipopolysaccharides from E. coli: the effects of endotoxin to the chronically of OME
- Prognostic significance of mastoid pneumatization in childhood otitis media with effusion: temporal bone CT evaluation