Clin Exp Otorhinolaryngol.
2010 Sep;3(3):141-146.
The Effect of Uvula-Preserving Palatopharyngoplasty in Obstructive Sleep Apnea on Globus Sense and Positional Dependency
- Affiliations
-
- 1Department of Otolaryngology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. yschung@amc.seoul.kr
Abstract
OBJECTIVES
This study investigated the outcomes of uvula-preserving palatopharyngoplasty (UPPPP) in patients with obstructive sleep apnea syndrome (OSAS).
METHODS
Twenty men with obstructive sleep apnea syndrome received the UPPPP operation at our institution. We measured symptom changes after UPPPP using a visual analog scale (VAS), and all patients were examined with polysomnography pre- and post-operatively. 'Surgical success' was defined as reduction in apnea-hypopnea index (AHI) to below 20 events per hour and more than 50% post-operative reduction.
RESULTS
Snoring decreased significantly (6.7+/-2.3 to 3.7+/-2.9 on VAS, P=0.002) but the postoperative globus sense did not differ from that preoperatively (2.0+/-2.4 to 2.1+/-2.7 on VAS, P=0.79). Apnea and apnea-hypopnea indices were significantly reduced after UPPPP (34.7+/-20 to 24.2+/-17.2 events/hour, P=0.029). The surgical success rate was 40% regardless of Friedman stage. There was significant reduction in the AHI on supine sleep in both surgically successful and unsuccessful patient groups.
CONCLUSION
UPPPP may minimize postoperative globus sense and other complications, with a success rate comparable to that of previously reported surgical methods in OSAS patients. In addition, it may reduce the apnea-hypopnea index in the supine sleep position.
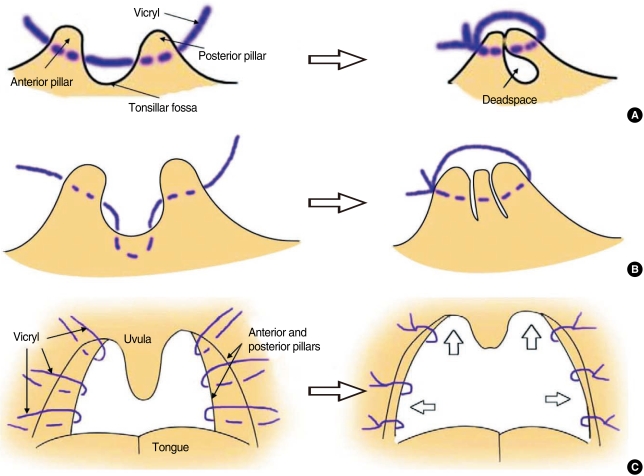
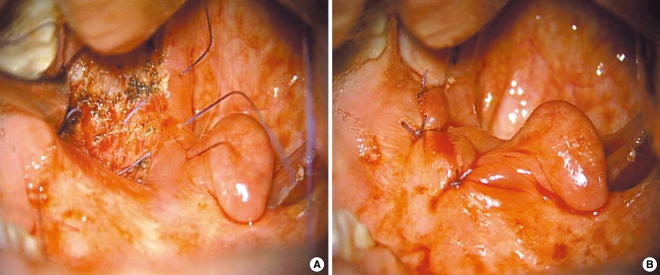
Figure
Reference
-
1. Moon HS. Influence of sleep-related breathing disorders in changes of cardiovascular function. Sleep Med Psychophysiol. 1997; 12. 4(2):129–139.2. Lee SH, Wang SG, Koo SK, Koo HE, Yun JH, Roh HJ, et al. Long-term polysomnographic findings and subjective results in sleep apnea patients treated with laser assisted uvulopalatoplasty. Korean J Otolaryngol-Head Neck Surg. 2002; 2. 45(2):144–148.3. Fujita S, Conway W, Zorick F, Roth T. Surgical correction of anatomic azbnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1981; Nov–Dec. 89(6):923–934. PMID: 6801592.4. Rapoport DM, Garay SM, Goldring RM. Nasal CPAP in obstructive sleep apnea: mechanisms of action. Bull Eur Physiopathol Respir. 1983; Nov–Dec. 19(6):616–620. PMID: 6360256.5. Croft CB, Golding-Wood DG. Uses and complications of uvulopalatopharyngoplasty. J Laryngol Otol. 1990; 11. 104(11):871–875. PMID: 2266310.
Article6. Haavisto L, Suonpaa J. Complications of uvulopalatopharyngoplasty. Clin Otolaryngol Allied Sci. 1994; 6. 19(3):243–247. PMID: 7923849.
Article7. Hagert B, Wikblad K, Odkvist L, Wahren LK. Side effects after surgical treatment of snoring. ORL J Otorhinolaryngol Relat Spec. 2000; Mar–Apr. 62(2):76–80. PMID: 10729796.
Article8. Goh YH, Mark I, Fee WE Jr. Quality of life 17 to 20 years after uvulopalatopharyngoplasty. Laryngoscope. 2007; 3. 117(3):503–506. PMID: 17334312.
Article9. Back GW, Nadig S, Uppal S, Coatesworth AP. Why do we have a uvula?: literature review and a new theory. Clin Otolaryngol Allied Sci. 2004; 12. 29(6):689–693. PMID: 15533161.
Article10. Han D, Ye J, Lin Z, Wang J, Zhang Y. Revised uvulopalatopharyngoplasty with uvula preservation and its clinical study. ORL J Otorhinolaryngol Relat Spec. 2005; 67(4):213–219. PMID: 16103738.
Article11. Gastaut H, Tassinari CA, Duron B. Polygraphic study of the episodic diurnal and nocturnal (hypnic and respiratory) manifestations of the Pickwick syndrome. Brain Res. 1966; 2. 1(2):167–186. PMID: 5923125.
Article12. Cartwright R, Ristanovic R, Diaz F, Caldarelli D, Alder G. A comparative study of treatments for positional sleep apnea. Sleep. 1991; 12. 14(6):546–552. PMID: 1798889.
Article13. Fujita S, Conway WA, Zorick FJ, Sicklesteel JM, Roehrs TA, Wittig RM, et al. Evaluation of the effectiveness of uvulopalatopharyngoplasty. Laryngoscope. 1985; 1. 95(1):70–74. PMID: 3965833.
Article14. Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996; 2. 19(2):156–177. PMID: 8855039.
Article15. Janson C, Gislason T, Bengtsson H, Eriksson G, Lindberg E, Lindholm CE, et al. Long-term follow-up of patients with obstructive sleep apnea treated with uvulopalatopharyngoplasty. Arch Otolaryngol Head Neck Surg. 1997; 3. 123(3):257–262. PMID: 9076230.
Article16. Schechtman KB, Sher AE, Piccirillo JF. Methodological and statistical problems in sleep apnea research: the literature on uvulopalatopharyngoplasty. Sleep. 1995; 10. 18(8):659–666. PMID: 8560132.
Article17. Friedman M, Ibrahim H, Joseph NJ. Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope. 2004; 3. 114(3):454–459. PMID: 15091218.
Article18. Finkelstein Y, Meshorer A, Talmi YP, Zohar Y, Brenner J, Gal R. The riddle of the uvula. Otolaryngol Head Neck Surg. 1992; 9. 107(3):444–450. PMID: 1408233.
Article19. Kezirian EJ, Weaver EM, Yueh B, Deyo RA, Khuri SF, Daley J, et al. Incidence of serious complications after uvulopalatopharyngoplasty. Laryngoscope. 2004; 3. 114(3):450–453. PMID: 15091217.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Characteristics Between the Positional Obstructive Sleep Apnea Patients with the Non-positional Obstructive Sleep Apnea Patients
- Association between Positional Dependency and Obstruction Site in Obstructive Sleep Apnea Syndrome
- The Prevalence and Characteristics of Positional Sleep Apnea in Korea
- The Differences of anthropometric and polysomnographic characteristics between the positional and non-positional obstructive sleep apnea syndrome
- Minimally Invasive Surgical Technique in Uvulopalatopharyngoplasty: Palatoglossal Line