Clin Exp Otorhinolaryngol.
2012 Apr;5(Suppl 1):S32-S36.
Changes in the Hearing Thresholds of Infants Who Failed the Newborn Hearing Screening Test and in Infants Treated in the Neonatal Intensive Care Unit
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Dong-A University College of Medicine, Busan, Korea. su0305@lycos.co.kr
Abstract
OBJECTIVES
The aim of this study was to investigate changes in the hearing thresholds during the first year of life in infants who failed the newborn hearing screening (NHS) test and of infants treated in the neonatal intensive care unit (NICU).
METHODS
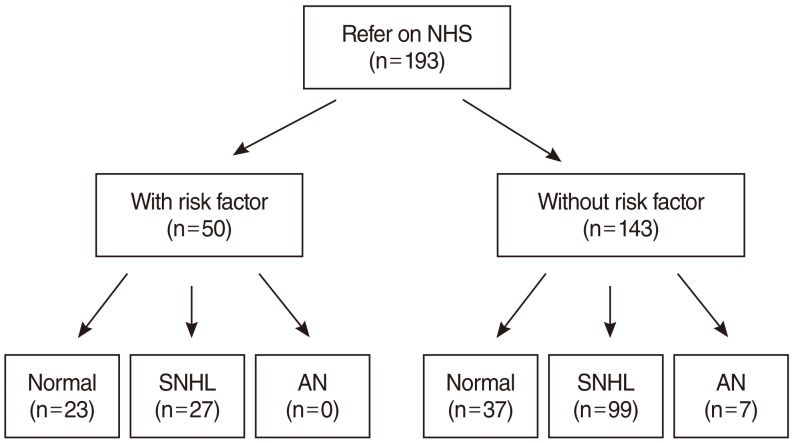
From March 2007 to November 2010, 193 healthy infants who failed the NHS test and 51 infants who were treated in the NICU were referred for evaluation of hearing acuity. Their hearing was evaluated using impedance audiometry, auditory brainstem response (ABR), and otoacoustic emission before 6 months of age, and follow-up hearing tests were administered before 12 months of age. Changes in their hearing thresholds were then analyzed.
RESULTS
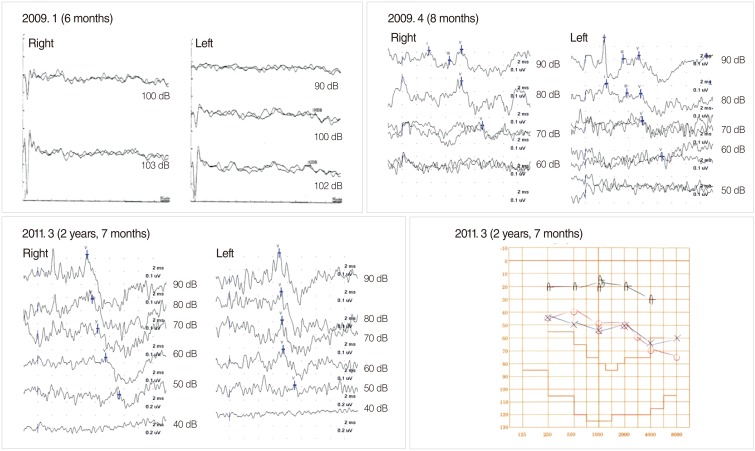
Of the 193 healthy infants who failed the NHS test, 60 infants (31%) had normal hearing acuity, 126 infants (65%) had sensorineural hearing loss (SNHL, ABR threshold > or =40 dB) and 7 infants (4%) had auditory neuropathy (AN). On the follow-up hearing tests, which were conducted in 65 infants, 6 infants showed a hearing threshold deterioration of more than 20 dB, and 19 infants showed a hearing threshold improvement of more than 20 dB. Of the 51 infants who were treated in the NICU, 38 infants (75%) had normal hearing acuity, 12 infants (24%) had SNHL, and one infant (2%) had AN. In the follow-up hearing tests, which were performed in 13 infants, one infant with normal hearing progressed to severe hearing loss. Five infants who had SNHL showed a hearing threshold improvement of more than 20 dB, and 4 infants recovered to normal hearing.
CONCLUSION
The hearing thresholds of infants with congenital SNHL can change during the first year of life; therefore, the importance of administration of follow-up hearing tests is emphasized. Irreversible intervention such as cochlear implantation should be considered with great caution within the first year after birth.
Keyword
MeSH Terms
Figure
Reference
-
1. Yoon PJ, Price M, Gallagher K, Fleisher BE, Messner AH. The need for long-term audiologic follow-up of neonatal intensive care unit (NICU) graduates. Int J Pediatr Otorhinolaryngol. 2003; 4. 67(4):353–357. PMID: 12663106.
Article2. Lee DS, Lee JS, Oh SH, Kim SK, Kim JW, Chung JK, et al. Cross-modal plasticity and cochlear implants. Nature. 2001; 1. 11. 409(6817):149–150. PMID: 11196628.
Article3. Sharma A, Dorman MF, Kral A. The influence of a sensitive period on central auditory development in children with unilateral and bilateral cochlear implants. Hear Res. 2005; 5. 203(1-2):134–143. PMID: 15855038.
Article4. Kim LS, Jeong SW, Lee YM, Kim JS. Cochlear implantation in children. Auris Nasus Larynx. 2010; 2. 37(1):6–17. PMID: 19897328.
Article5. Lesinski-Schiedat A, Illg A, Heermann R, Bertram B, Lenarz T. Paediatric cochlear implantation in the first and in the second year of life: a comparative study. Cochlear Implants Int. 2004; 12. 5(4):146–159. PMID: 18792210.
Article6. Colletti L, Mandala M, Zoccante L, Shannon RV, Colletti V. Infants versus older children fitted with cochlear implants: performance over 10 years. Int J Pediatr Otorhinolaryngol. 2011; 4. 75(4):504–509. PMID: 21277638.
Article7. Adachi N, Ito K, Sakata H, Yamasoba T. Etiology and one-year follow-up results of hearing loss identified by screening of newborn hearing in Japan. Otolaryngol Head Neck Surg. 2010; 7. 143(1):97–100. PMID: 20620626.
Article8. Morimoto N, Taiji H, Tsukamoto K, Morimoto Y, Nakamura T, Hommura T, et al. Risk factors for elevation of ABR threshold in NICU-treated infants. Int J Pediatr Otorhinolaryngol. 2010; 7. 74(7):786–790. PMID: 20434224.
Article9. Hosford-Dunn H, Simmons FB, Winzelberg J, Petroff M. Delayed onset hearing loss in a two-year old. Ear Hear. 1986; 4. 7(2):78–82. PMID: 3699263.
Article10. Lim HW, Han MW, Lee HS, Kim KS, Chung JW, Kim YJ, et al. The validity using two-stage automated auditory brainstem response as a universal newborn hearing screening protocol: experiences in Asan Medical Center. Korean J Otolaryngol-Head Neck Surg. 2007; 2. 50(2):108–114.11. Moon SK, Park HJ, Kim YJ, Park MS, Choung YH, Park KH. Results and cost-effectiveness of newborn hearing screening program in Ajou University Hospital. Korean J Otolaryngol-Head Neck Surg. 2002; 11. 45(11):1052–1056.12. Korres S, Nikolopoulos TP, Komkotou V, Balatsouras D, Kandiloros D, Constantinou D, et al. Newborn hearing screening: effectiveness, importance of high-risk factors, and characteristics of infants in the neonatal intensive care unit and well-baby nursery. Otol Neurotol. 2005; 11. 26(6):1186–1190. PMID: 16272939.
Article13. Vohr BR, Widen JE, Cone-Wesson B, Sininger YS, Gorga MP, Folsom RC, et al. Identification of neonatal hearing impairment: characteristics of infants in the neonatal intensive care unit and well-baby nursery. Ear Hear. 2000; 10. 21(5):373–382. PMID: 11059699.
Article14. Kraus N, Ozdamar O, Stein L, Reed N. Absent auditory brain stem response: peripheral hearing loss or brain stem dysfunction? Laryngoscope. 1984; 3. 94(3):400–406. PMID: 6700356.15. Rance G, Beer DE, Cone-Wesson B, Shepherd RK, Dowell RC, King AM, et al. Clinical findings for a group of infants and young children with auditory neuropathy. Ear Hear. 1999; 6. 20(3):238–252. PMID: 10386850.
Article16. Stein L, Tremblay K, Pasternak J, Banerjee S, Lindemann K, Kraus N. Brainstem abnormalities in neonates with normal otoacoustic emissions. Semin Hear. 1996; 5. 17(2):197–212.
Article17. Huang L, Kaga K, Hashimoto K. Progressive hearing loss in an infant in a neonatal intensive care unit as revealed by auditory evoked brainstem responses. Auris Nasus Larynx. 2002; 4. 29(2):187–190. PMID: 11893455.
Article18. Robertson CM, Howarth TM, Bork DL, Dinu IA. Permanent bilateral sensory and neural hearing loss of children after neonatal intensive care because of extreme prematurity: a thirty-year study. Pediatrics. 2009; 5. 123(5):e797–e807. PMID: 19403472.
Article19. US Preventive Services Task Force. Universal screening for hearing loss in newborns: US Preventive Services Task Force recommendation statement. Pediatrics. 2008; 7. 122(1):143–148. PMID: 18595997.20. Madden C, Rutter M, Hilbert L, Greinwald JH Jr, Choo DI. Clinical and audiological features in auditory neuropathy. Arch Otolaryngol Head Neck Surg. 2002; 9. 128(9):1026–1030. PMID: 12220206.
Article21. Amaral MI, Martins JE, Santos MF. A study on the hearing of children with non-syndromic cleft palate/lip. Braz J Otorhinolaryngol. 2010; Mar-Apr. 76(2):164–171. PMID: 20549075.22. Rhee CK, Park HM, Jang YJ. Audiologic evaluation of neonates with severe hyperbilirubinemia using transiently evoked otoacoustic emissions and auditory brainstem responses. Laryngoscope. 1999; 12. 109(12):2005–2008. PMID: 10591364.
Article23. Talero-Gutierrez C, Carvajalino-Monje I, Samper BS, Ibanez-Pinilla M. Delayed auditory pathway maturation in the differential diagnosis of hypoacusis in young children. Int J Pediatr Otorhinolaryngol. 2008; 4. 72(4):519–527. PMID: 18243343.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Newborn Hearing Screening: 3 Years of Experience
- Neonatal Hearing Screening in Neonatal Intensive Care Unit Graduate
- Newborn Hearing Screening Test: A Comparison between Infants in Neonatal Intensive Care Unit versus Nursery
- Incidence of hearing loss and importance of risk factors in the neonatal intensive care unit
- TEOAE as a Newborn Hearing Screening