Clin Exp Otorhinolaryngol.
2013 Jun;6(2):94-98.
Conversion from Selective to Comprehensive Neck Dissection: Is It Necessary for Occult Nodal Metastasis? 5-Year Observational Study
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Ilsong Memorial Institute of Head and Neck Cancer, Hallym University Medical Center, Seoul, Korea. cardiolo@empal.com
Abstract
OBJECTIVES
To compare the therapeutic results between selective neck dissection (SND) and conversion modified radical neck dissection (MRND) for the occult nodal metastasis cases in head and neck squamous cell carcinoma.
METHODS
Forty-four cases with occult nodal metastasis were enrolled in this observational cohort study. For twenty-nine cases, SNDs were done and for fifteen cases, as metastatic nodes were found in the operative field, conversion from selective to MRNDs type II were done. Baseline data on primary site, T and N stage, extent of SND, extracapsular spread of occult metastatic node and type of postoperative adjuvant therapy were obtained. We compared locoregional control rate, overall survival rate and disease specific survival rate between two groups.
RESULTS
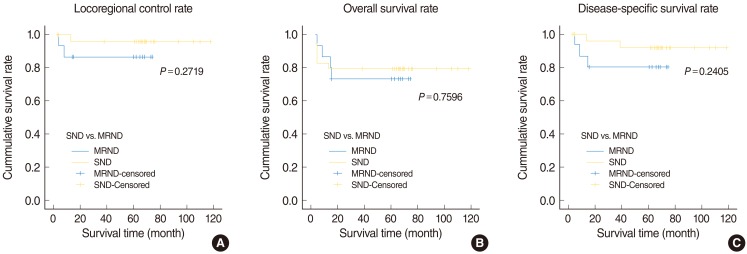
Among the 29 patients who underwent SND, only one patient had a nodal recurrence which occurred in the contralateral undissected neck. On the other hand, among the 15 patients who underwent conversion MRND, two patients had nodal recurrences which occurred in previously undissected neck. According to the Kaplan Meier survival curve, there was no statistically significant difference for locoregional control rate, overall survival rate and disease specific survival rate between two groups (P=0.2719, P=0.7596, and P=0.2405, respectively).
CONCLUSION
SND is enough to treat occult nodal metastasis in head and neck squamous cell carcinoma and it is not necessary to convert from SND to comprehensive neck dissection.
Keyword
MeSH Terms
Figure
Reference
-
1. Ferlito A, Rinaldo A, Silver CE, Gourin CG, Shah JP, Clayman GL, et al. Elective and therapeutic selective neck dissection. Oral Oncol. 2006; 1. 42(1):14–25. PMID: 15979381.
Article2. Patel RS, Clark JR, Gao K, O'Brien CJ. Effectiveness of selective neck dissection in the treatment of the clinically positive neck. Head Neck. 2008; 9. 30(9):1231–1236. PMID: 18642289.
Article3. Pagedar NA, Gilbert RW. Selective neck dissection: a review of the evidence. Oral Oncol. 2009; Apr-May. 45(4-5):416–420. PMID: 19091624.
Article4. Schiff BA, Roberts DB, El-Naggar A, Garden AS, Myers JN. Selective vs modified radical neck dissection and postoperative radiotherapy vs observation in the treatment of squamous cell carcinoma of the oral tongue. Arch Otolaryngol Head Neck Surg. 2005; 10. 131(10):874–878. PMID: 16230589.
Article5. Lim YC, Lee JS, Choi EC. Therapeutic selective neck dissection (level II-V) for node-positive hypopharyngeal carcinoma: is it oncologically safe? Acta Otolaryngol. 2009; 1. 129(1):57–61. PMID: 18607981.
Article6. Huang SF, Kang CJ, Lin CY, Fan KH, Yen TC, Wang HM, et al. Neck treatment of patients with early stage oral tongue cancer: comparison between observation, supraomohyoid dissection, and extended dissection. Cancer. 2008; 3. 112(5):1066–1075. PMID: 18246535.7. Yuen AP, Ho CM, Chow TL, Tang LC, Cheung WY, Ng RW, et al. Prospective randomized study of selective neck dissection versus observation for N0 neck of early tongue carcinoma. Head Neck. 2009; 6. 31(6):765–772. PMID: 19408291.
Article8. Jin WL, Ye WM, Zheng JW, Zhou L, Zhu HG, Zhang ZY, et al. Occult cervical lymph node metastases in 100 consecutive patients with cN0 tongue cancer. Chin Med J (Engl). 2008; 10. 121(19):1871–1874. PMID: 19080116.
Article9. Gourin CG, Conger BT, Porubsky ES, Sheils WC, Bilodeau PA, Coleman TA. The effect of occult nodal metastases on survival and regional control in patients with head and neck squamous cell carcinoma. Laryngoscope. 2008; 7. 118(7):1191–1194. PMID: 18391764.
Article10. Finn S, Toner M, Timon C. The node-negative neck: accuracy of clinical intraoperative lymph node assessment for metastatic disease in head and neck cancer. Laryngoscope. 2002; 4. 112(4):630–633. PMID: 12150514.
Article11. Talmi YP, Hoffman HT, Horowitz Z, McCulloch TM, Funk GF, Graham SM, et al. Patterns of metastases to the upper jugular lymph nodes (the "submuscular recess"). Head Neck. 1998; 12. 20(8):682–686. PMID: 9790288.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experience of the Elective Neck Dissection in Clinical N0 Neck
- Elective Neck Dissection in Oral Squamous Cell Carcinoma
- Occult Papillary Carcinoma of the Thyroid
- Frequency and Patterns of nodal metastasis in supraglottic squamous cell carcinoma
- Occult Neck Metastasis in Larynx and Hypopharynx Squamous Cell Carcinomas Confirmed with Simultaneous Bilateral Elective Neck Dissection