Clin Exp Otorhinolaryngol.
2014 Dec;7(4):319-323. 10.3342/ceo.2014.7.4.319.
Mapping Regional Laryngopharyngeal Mechanoreceptor Response
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, University of Texas Medical Branch, Galveston, TX, USA. seckin.ulualp@utsouthwestern.edu
- KMID: 2278374
- DOI: http://doi.org/10.3342/ceo.2014.7.4.319
Abstract
OBJECTIVES
To map mechanoreceptor response in various regions of the laryngopharynx.
METHODS
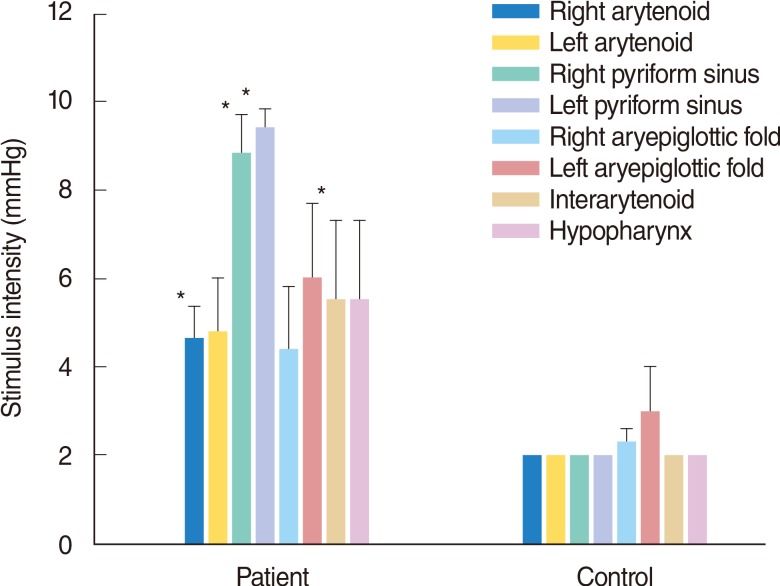
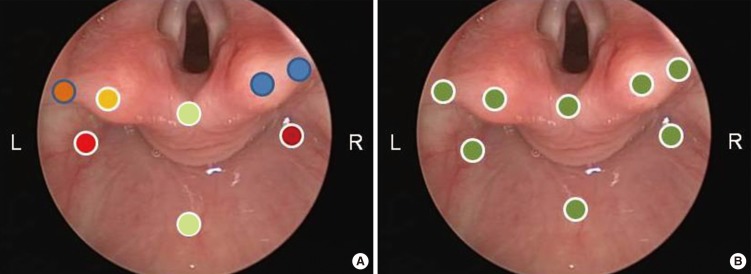
Five patients with suspected laryngopharyngeal reflux and six healthy control subjects underwent stimulation of mechanoreceptors in the hypopharynx, interarytenoid area, arytenoids, aryepiglottic folds, and pyriform sinuses. The threshold stimuli evoking sensation and eliciting laryngeal adductor reflex were recorded.
RESULTS
In controls, an air pulse with 2 mmHg pressure evoked mechanoreceptor response in all regions, except bilateral aryepiglottic folds of one control. In patients, stimulus intensity to elicit mechanoreceptor response ranged between 2 mmHg and 10 mmHg and varied among the regions. Air pulse intensity differed between right and left sides of laryngopharyngeal regions in the majority of patients.
CONCLUSION
Laryngopharyngeal mechanoreceptor response was uniform among regions and subjects in the healthy group. Patients with suspected laryngopharyngeal reflux showed inter- and intra-regional variations in mechanoreceptor response. Laryngopharyngeal sensory deficit in patients with suspected laryngopharyngeal reflux is not limited to aryepiglottic folds.
Figure
Reference
-
1. Aviv JE, Martin JH, Keen MS, Debell M, Blitzer A. Air pulse quantification of supraglottic and pharyngeal sensation: a new technique. Ann Otol Rhinol Laryngol. 1993; 10. 102(10):777–780. PMID: 8215097.
Article2. Aviv JE, Martin JH, Sacco RL, Zagar D, Diamond B, Keen MS, et al. Supraglottic and pharyngeal sensory abnormalities in stroke patients with dysphagia. Ann Otol Rhinol Laryngol. 1996; 2. 105(2):92–97. PMID: 8659942.
Article3. Aviv JE, Liu H, Parides M, Kaplan ST, Close LG. Laryngopharyngeal sensory deficits in patients with laryngopharyngeal reflux and dysphagia. Ann Otol Rhinol Laryngol. 2000; 11. 109(11):1000–1006. PMID: 11089989.
Article4. Aviv JE, Parides M, Fellowes J, Close LG. Endoscopic evaluation of swallowing as an alternative to 24-hour pH monitoring for diagnosis of extraesophageal reflux. Ann Otol Rhinol Laryngol Suppl. 2000; 10. 184:25–27. PMID: 11051427.
Article5. Setzen M, Cohen MA, Mattucci KF, Perlman PW, Ditkoff MK. Laryngopharyngeal sensory deficits as a predictor of aspiration. Otolaryngol Head Neck Surg. 2001; 6. 124(6):622–624. PMID: 11391251.
Article6. Suskind DL, Thompson DM, Gulati M, Huddleston P, Liu DC, Baroody FM. Improved infant swallowing after gastroesophageal reflux disease treatment: a function of improved laryngeal sensation? Laryngoscope. 2006; 8. 116(8):1397–1403. PMID: 16885743.
Article7. Thompson DM. Abnormal sensorimotor integrative function of the larynx in congenital laryngomalacia: a new theory of etiology. Laryngoscope. 2007; 6. 117(6 Pt 2):Suppl 114. 1–33. PMID: 17513991.
Article8. Thompson DM, Rutter MJ, Rudolph CD, Willging JP, Cotton RT. Altered laryngeal sensation: a potential etiology of apnea of infancy. Ann Otol Rhinol Laryngol. 2005; 4. 114(4):258–263. PMID: 15895779.9. Amin MR, Harris D, Cassel SG, Grimes E, Heiman-Patterson T. Sensory testing in the assessment of laryngeal sensation in patients with amyotrophic lateral sclerosis. Ann Otol Rhinol Laryngol. 2006; 7. 115(7):528–534. PMID: 16900807.
Article10. Carr MM, Nguyen A, Poje C, Pizzuto M, Nagy M, Brodsky L. Correlation of findings on direct laryngoscopy and bronchoscopy with presence of extraesophageal reflux disease. Laryngoscope. 2000; 9. 110(9):1560–1562. PMID: 10983962.
Article11. Carr MM, Nagy ML, Pizzuto MP, Poje CP, Brodsky LS. Correlation of findings at direct laryngoscopy and bronchoscopy with gastroesophageal reflux disease in children: a prospective study. Arch Otolaryngol Head Neck Surg. 2001; 4. 127(4):369–374. PMID: 11296043.12. Ulualp SO, Toohill RJ, Hoffmann R, Shaker R. Pharyngeal pH monitoring in patients with posterior laryngitis. Otolaryngol Head Neck Surg. 1999; 5. 120(5):672–677. PMID: 10229591.
Article13. Ulualp SO, Toohill RJ, Shaker R. Pharyngeal acid reflux in patients with single and multiple otolaryngologic disorders. Otolaryngol Head Neck Surg. 1999; 12. 121(6):725–730. PMID: 10580227.
Article14. Ulualp SO, Toohill RJ. Laryngopharyngeal reflux: state of the art diagnosis and treatment. Otolaryngol Clin North Am. 2000; 8. 33(4):785–802. PMID: 10918661.15. Belafsky PC, Postma GN, Koufman JA. The validity and reliability of the reflux symptom index (RSI). J Voice. 2002; 6. 16(2):274–277. PMID: 12150380.16. Aviv JE, Martin JH, Kim T, Sacco RL, Thomson JE, Diamond B, et al. Laryngopharyngeal sensory discrimination testing and the laryngeal adductor reflex. Ann Otol Rhinol Laryngol. 1999; 8. 108(8):725–730. PMID: 10453777.
Article17. Yoshida Y, Tanaka Y, Hirano M, Nakashima T. Sensory innervation of the pharynx and larynx. Am J Med. 2000; 3. 108(Suppl 4a):51S–61S. PMID: 10718453.
Article18. Botoman VA, Hanft KL, Breno SM, Vickers D, Astor FC, Caristo IB, et al. Prospective controlled evaluation of pH testing, laryngoscopy and laryngopharyngeal sensory testing (LPST) shows a specific posterior inter-arytenoid neuropathy in proximal GERD (P-GERD). LPST improves laryngoscopy diagnostic yield in PGERD. Am J Gastroenterol. 2002; 9. 97(9 Suppl):S11–S12.
Article19. Shaker R, Ulualp SO, Kannappan A, Narayannan S, Hofmann C. Identification of laryngo-UES contractile reflex in humans. Gastroenterology. 1999; 116(4 Pt 2):A1081.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Histologic Mapping of Sensory Innervation in the Human Anterior Cruciate Ligament
- The laryngopharyngeal nerve: a comprehensive review
- The Change of the Mechanoreceptor fo Anterior Cruciate Ligament after Injuries of Medial Articular Cartilage and Ligament in the Rabbit
- The Change of the Mechanoreceptor in Anterior Cruciate Ligament following Injury of Posterior Cruciate Ligament in the Rabbit
- The Usefulness of Esophagography as a Screening Test for Laryngopharyngeal Reflux