Clinical Experiences of Transforaminal Balloon Decompression for Patients with Spinal Stenosis
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. jinwoos@amc.seoul.kr
- KMID: 2278118
- DOI: http://doi.org/10.3344/kjp.2012.25.1.55
Abstract
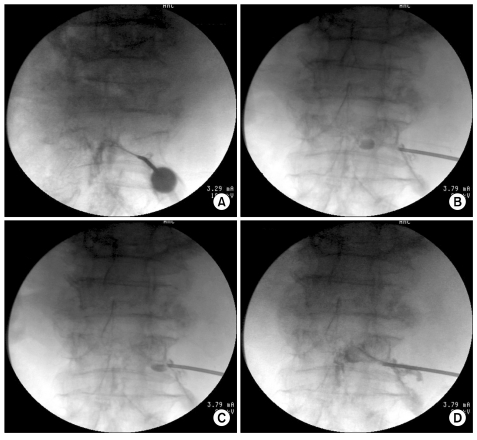
- Lumbar spinal stenosis is a commonly treated with epidural injections of local anesthetics and corticosteroids, however, these therapies may relieve leg pain for weeks to months but do not influence functional status. Furthermore, the majority of patients report no substantial symptom change over the repeated treatment. Utilizing balloon catheters, we successfully treated with three patients who complained persistent symptoms despite repeated conventional steroid injections. Our results suggest that transforaminal decompression using a balloon catheter may have potential in the nonsurgical treatment of spinal stenosis by modifying the underlying pathophysiology.
MeSH Terms
Figure
Cited by 5 articles
-
Clinical experiences of performing transforaminal balloon adhesiolysis in patients with failed back surgery syndrome: two cases report
Bo-Young Hwang, Hong-Seok Ko, Jeong-Hun Suh, Jin-Woo Shin, Jeong-Gill Leem, Jae-Do Lee
Korean J Anesthesiol. 2014;66(2):169-172. doi: 10.4097/kjae.2014.66.2.169.A New Approach to Neuroplasty
Jin Woo Shin
Korean J Pain. 2013;26(4):323-326. doi: 10.3344/kjp.2013.26.4.323.A Novel Balloon-Inflatable Catheter for Percutaneous Epidural Adhesiolysis and Decompression
Seong Soo Choi, Eun Young Joo, Beom Sang Hwang, Jong Hyuk Lee, Gunn Lee, Jeong Hun Suh, Jeong Gill Leem, Jin Woo Shin
Korean J Pain. 2014;27(2):178-185. doi: 10.3344/kjp.2014.27.2.178.The Effects of a Forceful Transforaminal Epidural Steroid Injection on Radicular Pain: A Preliminary Study
Jong Min Byun, Hahck Soo Park, Jae Hee Woo, Jin Kim
Korean J Pain. 2014;27(4):334-338. doi: 10.3344/kjp.2014.27.4.334.Percutaneous epidural balloon neuroplasty: a narrative review of current evidence
Doo-Hwan Kim, Jin-Woo Shin, Seong-Soo Choi
Anesth Pain Med. 2022;17(4):361-370. doi: 10.17085/apm.22237.
Reference
-
1. Atlas SJ, Keller RB, Robson D, Deyo RA, Singer DE. Surgical and nonsurgical management of lumbar spinal stenosis: four-year outcomes from the maine lumbar spine study. Spine (Phila Pa 1976). 2000; 25:556–562. PMID: 10749631.2. Benoist M. The natural history of lumbar degenerative spinal stenosis. Joint Bone Spine. 2002; 69:450–457. PMID: 12477228.
Article3. Armon C, Argoff CE, Samuels J, Backonja MM. Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007; 68:723–729. PMID: 17339579.
Article4. Hwang BM, Hwang BS. A comparison of the efficacy of epidural steroid injections in terms of the dosages and frequency of triancinolone injections for the pain related to lumbar spinal stenosis or herniated disks. Korean J Pain. 2006; 19:72–76.
Article5. Hong JH, Lee YC, Lee HM, Kang CH. An analysis of the outcome of transforaminal epidural steroid injections in patients with spinal stenosis or herniated intervertebral discs. Korean J Pain. 2008; 21:38–43.
Article6. Katz JN, Harris MB. Clinical practice. Lumbar spinal stenosis. N Engl J Med. 2008; 358:818–825. PMID: 18287604.7. Winnie AP, Hartman JT, Meyers HL Jr, Ramamurthy S, Barangan V. Pain clinic. II. Intradural and extradural corticosteroids for sciatica. Anesth Analg. 1972; 51:990–1003. PMID: 4678361.8. Coderre TJ. Contribution of protein kinase C to central sensitization and persistent pain following tissue injury. Neurosci Lett. 1992; 140:181–184. PMID: 1501774.
Article9. Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990; 34:335–338. PMID: 2167604.
Article10. Yabuki S, Kikuchi S. Nerve root infiltration and sympathetic block. An experimental study of intraradicular blood flow. Spine (Phila Pa 1976). 1995; 20:901–906. PMID: 7644954.11. Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998; 14:148–151. PMID: 9647457.
Article12. Geurts JW, Kallewaard JW, Richardson J, Groen GJ. Targeted methylprednisolone acetate/hyaluronidase/clonidine injection after diagnostic epiduroscopy for chronic sciatica: a prospective, 1-year follow-up study. Reg Anesth Pain Med. 2002; 27:343–352. PMID: 12132057.
Article13. Parke WW, Watanabe R. The intrinsic vasculature of the lumbosacral spinal nerve roots. Spine (Phila Pa 1976). 1985; 10:508–515. PMID: 4081865.14. Kobayashi S, Takeno K, Miyazaki T, Kubota M, Shimada S, Yayama T, et al. Effects of arterial ischemia and venous congestion on the lumbar nerve root in dogs. J Orthop Res. 2008; 26:1533–1540. PMID: 18536056.
Article15. Lee JS, Kwon HT, Park CH. Anterior epidural irrigation in a lumbar spinal stenosis patient. Korean J Pain. 2006; 19:63–67.
Article16. Olmarker K, Rydevik B, Holm S. Edema formation in spinal nerve roots induced by experimental, graded compression. An experimental study on the pig cauda equina with special reference to differences in effects between rapid and slow onset of compression. Spine (Phila Pa 1976). 1989; 14:569–573. PMID: 2546258.
Article17. Basaran A, Topatan S. Spinal balloon nucleoplasty: a hypothetical minimally invasive treatment for herniated nucleus pulposus. Med Hypotheses. 2008; 70:1201–1206. PMID: 18096323.
Article18. Pedowitz RA, Garfin SR, Massie JB, Hargens AR, Swenson MR, Myers RR, et al. Effects of magnitude and duration of compression on spinal nerve root conduction. Spine (Phila Pa 1976). 1992; 17:194–199. PMID: 1553590.
Article19. Song SO, Lim HJ. Clinical experience of epidural adhesiolysis in patients with failed back surgery syndrome. Korean J Anesthesiol. 2004; 47:547–552.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical study on the posterior decompression and posterolateral fusion with instrumentation in lumbar spinal stenosis
- Treatment of lumbar spinal stenosis after fracture of posterior ring apophysis by anterior decompression
- Uniportal Endoscopic Lumbar Interbody Fusion
- Spinal Stenosis Presenting with Scrotal and Perianal Claudication
- Percutaneous epidural balloon neuroplasty: a narrative review of current evidence