Korean J Pediatr Gastroenterol Nutr.
2011 Dec;14(4):368-375. 10.5223/kjpgn.2011.14.4.368.
Diagnostic Yield of Pediatric Colonoscopies Based on Presenting Symptoms in a Secondary Hospital
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, The Catholic University of Korea, Seoul, Korea. sykim2010@catholic.ac.kr
- 2Department of Internal Medicine, School of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2277708
- DOI: http://doi.org/10.5223/kjpgn.2011.14.4.368
Abstract
- PURPOSE
We performed this study retrospectively to review the diagnostic yield of colonoscopies in children and adolescents with various gastrointestinal symptoms and to investigate the relationship between presenting symptoms and the colonoscopic findings in a secondary hospital.
METHODS
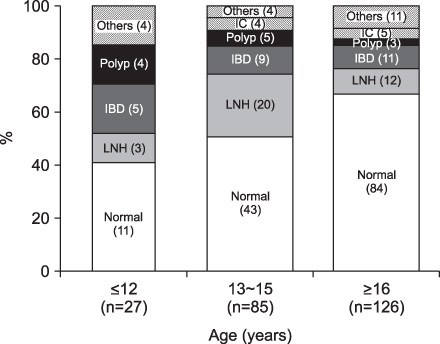
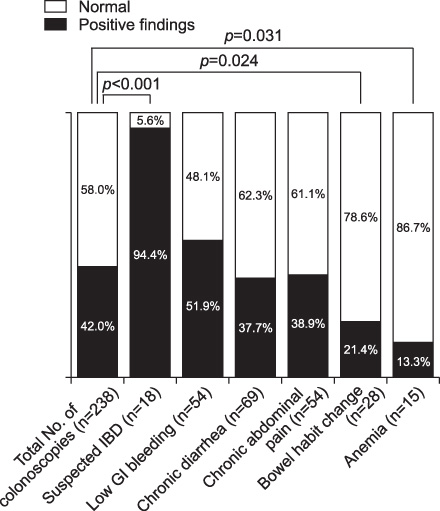
We reviewed the medical records of patients under the age of 19-years who underwent ileocolonoscopy between January 2001 and December 2010. The total number of patients (n=238) were divided into three age groups and six symptom groups. We analyzed clinical characteristics and the colonoscopic findings, and compared the colonoscopic yield between each groups.
RESULTS
The median age of the patients was 16.1 (3.1~18.9) years. The most common presenting symptoms were lower gastrointestinal (GI) bleeding (48.1%) in the < or =12 years group (n=27), chronic abdominal pain (31.8%) in the 13~15 years group (n=85), and chronic diarrhea (34.9%) in the > or =16 years group (n=126). Positive colonoscopic findings were found in 21.4% of the bowel habit change group (n=28), 51.9% of the low GI bleeding group (n=54), 37.7% of the chronic diarrhea group (n=69), and 94.4% of the group with suspected inflammatory bowel disease (IBD) (n=18), 38.9% of the chronic abdominal pain group (n=54) and 13.3% of the anemia group (n=15). The diagnostic yield of the total examination was 42.0%. The suspected IBD group had a higher yield than the presenting symptom groups (p<0.001).
CONCLUSION
Colonoscopy is a safe and useful investigation in children and adolescents with suspected colonic disease. The diagnostic yield of colonoscopy is higher in patients presenting with suspected IBD. Pediatricians practicing in primary or secondary care settings should recommend colonoscopy for patients with suspected IBD.
Keyword
MeSH Terms
Figure
Reference
-
1. Hyams JS, Treem WR, Justinich CJ, Davis P, Shoup M, Burke G. Characterization of symptoms in children with recurrent abdominal pain: resemblance to irritable bowel syndrome. J Pediatr Gastroenterol Nutr. 1995. 20:209–214.2. El Matary W, Spray C, Sandhu B. Irritable bowel syndrome: the commonest cause of recurrent abdominal pain in children. Eur J Pediatr. 2004. 163:584–588.
Article3. de Ridder L, van Lingen AV, Taminiau JA, Benninga MA. Rectal bleeding in children: endoscopic evaluation revisited. Eur J Gastroenterol Hepatol. 2007. 19:317–320.
Article4. Kay M, Wyllie R. Wyllie R, Hyams JS, Kay M, editors. Colonoscopy, polypectomy, and related techniques. Pediatric gastrointestinal and liver disease. 2011. 4th ed. Philadelphia: Elsevier Inc.;650–667.
Article5. Seo JK. Pediatric endoscopy for the diagnosis and management of gastrointestinal diseases in children. J Korean Pediatr Soc. 1996. 39:461–474.6. Gans SL, Ament M, Christie DL, Liebman WM. Pediatric endoscopy with flexible fiberscopes. J Pediatr Surg. 1975. 10:375–380.
Article7. Park EB. Pediatric colonoscopy. Korean J Gastrointest Endosc. 1984. 4:28–34.8. Seo JK. Pediatric endoscopy. Proceedings of The 3rd Gastrointestinal Endoscopy Seminar. 1990. 1990 Sep 9; Seoul, Korea: The Korean Society of Gastrointestinal Endoscopy.9. Seo JK. Infant and pediatric endoscopy. Proceedings of The 28th Gastrointestinal Endoscopy Seminar. 2003. 2003 Mar 30; Seoul, Korea: The Korean Society of Gastrointestinal Endoscopy.10. Park KH, Park JH. Changes in pediatric gastrointestinal endoscopy: review of a recent hospital experience. Korean J Pediatr Gastroenterol Nutr. 2007. 10:20–27.
Article11. Park JH. Role of colonoscopy in the diagnosis and treatment of pediatric lower gastrointestinal disorders. Korean J Pediatr. 2010. 53:824.
Article12. Nam YN, Lee SH, Chung DH, Sim S-Y, Eun BW, Choi DY, et al. The clinical and histopathologic findings of lymphonodular hyperplasia of the colon in infancy and childhood. Korean J Pediatr Gastroenterol Nutr. 2009. 12:1–9.
Article13. Griffiths A, Hugot J. Kleinman R, Sanderson I, Goulet O, Sherman P, editors. Chronic inflammatory bowel disease. Walker's pediatric gastrointestinal disease 5. 2008. 5th ed. Hamilton: BC Decker Inc;519–543.14. Croft N. Kleinman R, Sanderson I, Goulet O, Sherman P, editors. Ulcerative and indeterminate colitis. Walker's pediatric gastrointestinal disease 5. 2008. 5th ed. Hamilton: BC Decker Inc;545–557.15. Glader B. Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. The anemias. Nelson textbook of pediatrics. 2007. 18th ed. Philadelphia: Saunders;2003–2006.16. Hassall E, Barclay GN, Ament ME. Colonoscopy in childhood. Pediatrics. 1984. 73:594–599.
Article17. Colon AR, DiPalma JS, Leftridge CA. Intestinal lymphonodular hyperplasia of childhood: patterns of presentation. J Clin Gastroenterol. 1991. 13:163–166.18. Kokkonen J, Karttunen TJ. Lymphonodular hyperplasia on the mucosa of the lower gastrointestinal tract in children: an indication of enhanced immune response? J Pediatr Gastroenterol Nutr. 2002. 34:42–46.
Article19. Kim BJ, Song SM, Kim KM, Lee YJ, Rhee KW, Jang JY, et al. Characteristics and trends in the incidence of inflammatory bowel disease in Korean children: a single-center experience. Dig Dis Sci. 2010. 55:1989–1995.
Article20. Choe YH. Diagnosis of Inflammatory bowel disease in children. Korean J Pediatr Gastroenterol Nutr. 2008. 11:67–71.21. Mamula P, Markowitz JE, Baldassano RN. Inflammatory bowel disease in early childhood and adolescence: special considerations. Gastroenterol Clin North Am. 2003. 32:967–995. viii
Article22. Stites T, Lund DP. Common anorectal problems. Semin Pediatr Surg. 2007. 16:71–78.
Article23. Ahmed SK, Thomson HJ. The effect of breakfast on minor anal complaints: a matched case-control study. J R Coll Surg Edinb. 1997. 42:331–333.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Appropriateness of Colonoscopy Indication and the Diagnostic Yield of Colonoscopy
- Endoscopic Findings in Patients Under the Age of 40 Years with Hematochezia in Singapore
- Diagnostic Yield of Emergency Brain Magnetic Resonance Imaging in the Evaluation of Patients with Acute Dizziness in a University Hospital
- Pediatric syncope: pearls and pitfalls in history taking
- Magnetic resonance imaging as the first diagnostic imaging modality for pregnant women with suspected acute appendicitis