Korean J Obstet Gynecol.
2011 Sep;54(9):492-498. 10.5468/KJOG.2011.54.9.492.
The predictive value of postoperative cervical length after emergent and urgent cervical cerclage as a predictive factor of preterm delivery
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kangnam Sacred Hospital, Hallym University School of Medicine, Seoul, Korea. csran@hallym.or.kr
- KMID: 2274073
- DOI: http://doi.org/10.5468/KJOG.2011.54.9.492
Abstract
OBJECTIVE
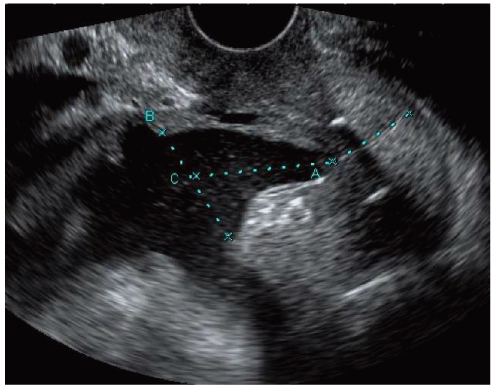
The aim of this study is to evaluate the value of the ultrasonographic cervical length after emergent and urgent cervical cerclage to prediction of preterm delivery in patients with incompetence of cervix.
METHODS
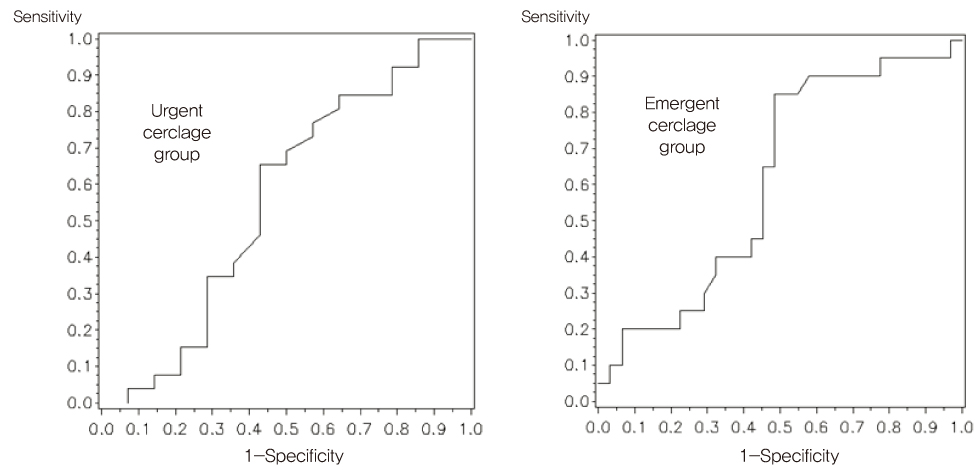
Fifty-one women who underwent emergent cervical cerclage and forty women who underwent urgent cervical cerclage were studied respectively. Receiver-operating characteristic (ROC) curve analysis, Pearson's partial correlation coefficient, and multiple logistic regression analysis were used for statistical analysis.
RESULTS
The mean gestational age at admission was 21.2 +/- 2.3 weeks in emergent cerclage group and 21.8 +/- 3.2 weeks in urgent cerclage group. Postoperative mean cervical length was 17.6 +/- 8.6 mm in emergent group and 21.8 +/- 8.7 mm in urgent group. The diagnostic indices of postoperative cervical length (cut-off value 16.5 mm in emergent cerclage, 23.2 mm in urgency cerclage) by ROC curve were sensitivity of 65%, specificity of 45%, positive predictive value of 17%, and negative predictive value of 8% in emergent cerclage group and in urgent cerclage group, sensitivity of 85%, specificity of 50%, positive predictive value of 17%, and negative predictive value of 16%. Multiple logistic regression analysis indicated that postoperative cervical length was not an independent predictor of preterm delivery after adjustment of confounding factors in emergent group (P=0.65) in urgent groups (P=0.77).
CONCLUSION
In the both groups, the postoperative cervical length was longer than preoperative. However the postoperative cervical length is not a useful predictor of preterm delivery in patients with emergent and urgent cervical cerclage.
Keyword
MeSH Terms
Figure
Reference
-
1. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996. 334:567–572.2. Drakeley AJ, Roberts D, Alfirevic Z. Cervical stitch (cerclage) for preventing pregnancy loss in women. Cochrane Database Syst Rev. 2003. (1):CD003253.3. Althuisius SM, Dekker GA, Hummel P, van Geijn HP. Cervical incompetence prevention randomized cerclage trial. Cervical incompetence prevention randomized cerclage trial: emergency cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2003. 189:907–910.4. Berghella V, Odibo AO, Tolosa JE. Cerclage for prevention of preterm birth in women with a short cervix found on transvaginal ultrasound examination: a randomized trial. Am J Obstet Gynecol. 2004. 191:1311–1317.5. To MS, Alfirevic Z, Heath VC, Cicero S, Cacho AM, Williamson PR, et al. Cervical cerclage for prevention of preterm delivery in women with short cervix: randomised controlled trial. Lancet. 2004. 363:1849–1853.6. Lee KY, Jun HA, Kim HB, Kang SW. Interleukin-6, but not relaxin, predicts outcome of rescue cerclage in women with cervical incompetence. Am J Obstet Gynecol. 2004. 191:784–789.7. Gupta M, Emary K, Impey L. Emergency cervical cerclage: predictors of success. J Matern Fetal Neonatal Med. 2010. 23:670–674.8. Mancuso MS, Szychowski JM, Owen J, Hankins G, Iams JD, Sheffield JS, et al. Cervical funneling: effect on gestational length and ultrasound-indicated cerclage in high-risk women. Am J Obstet Gynecol. 2010. 203:259.e1–259.e5.9. Andersen HF, Nugent CE, Wanty SD, Hayashi RH. Prediction of risk for preterm delivery by ultrasonographic measurement of cervical length. Am J Obstet Gynecol. 1990. 163:859–867.10. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA. Effectiveness of cerclage according to severity of cervical length shortening: a meta-analysis. Ultrasound Obstet Gynecol. 2010. 35:468–473.11. Fuchs F, Bouyer J, Fernandez H, Gervaise A, Frydman R, Senat MV. Ultrasound cervical length measurement for prediction of delivery before 32 weeks in women with emergency cerclage for cervical insufficiency. Int J Gynaecol Obstet. 2010. 110:245–248.12. Scheib S, Visintine JF, Miroshnichenko G, Harvey C, Rychlak K, Berghella V. Is cerclage height associated with the incidence of preterm birth in women with an ultrasound-indicated cerclage? Am J Obstet Gynecol. 2009. 200:e12–e15.13. Weiner CP, Lee KY, Buhimschi CS, Christner R, Buhimschi IA. Proteomic biomarkers that predict the clinical success of rescue cerclage. Am J Obstet Gynecol. 2005. 192:710–718.14. Steel A, Yoong W, Okolo S, Fakokunde A. Is there still a role for emergency cerclage in the developed world? An experience from a London district hospital. Arch Gynecol Obstet. 2008. 277:139–142.15. Dijkstra K, Funai EF, O'Neill L, Rebarber A, Paidas MJ, Young BK. Change in cervical length after cerclage as a predictor of preterm delivery. Obstet Gynecol. 2000. 96:346–350.16. Hedriana HL, Lanouette JM, Haesslein HC, McLean LK. Is there value for serial ultrasonographic assessment of cervical lengths after a cerclage? Am J Obstet Gynecol. 2008. 198:705.e1–705.e6.17. Rust OA, Atlas RO, Meyn J, Wells M, Kimmel S. Does cerclage location influence perinatal outcome? Am J Obstet Gynecol. 2003. 189:1688–1691.18. Song JE, Lee KY, Kim MY, Jun HA. Cervical funneling after cerclage in cervical incompetence as a predictor of pregnancy outcome. J Matern Fetal Neonatal Med. 2011. Apr. 04. [Epub]. DOI: 10.3109/14767058.2011.565835.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Change in cervical length after therapeutic McDonald cerclage using a transvaginal ultrasonography as a predictor of term delivery
- Post-cerclage ultrasonographic cervical length can predict preterm delivery in elective cervical cerclage patients
- Uterine Cervical Length Measurement by Transvaginal Ultrasonography for Prediction of Preterm Delivery
- Association of Cervical Length and Term Delivery after Elective Cerclage in Women with High Risk of Preterm Delivery
- Transvaginal Ultrasonographic Evaluation of the Uterine Cervix in Preterm Labor