Cancer Res Treat.
2006 Apr;38(2):84-91.
Evaluation of Parotid Gland Function following Intensity Modulated Radiation Therapy for Head and Neck Cancer
- Affiliations
-
- 1Research Institute and Hospital, National Cancer Center, Goyang, Korea. kwancho@ncc.re.kr
Abstract
-
PURPOSE: This study was undertaken to determine the parotid gland tolerance dose levels following intensity modulated radiation therapy (IMRT) for treating patients who suffered with head and neck cancer.
MATERIALS AND METHODS
From February 2003 through June 2004, 34 head and neck patients with 6 months of follow-up were evaluated for xerostomia after being treated by IMRT. Their median age was 59 years (range: 29~78). Xerostomia was assessed using a 4-question xerostomia questionnaire score (XQS) and a test for the salivary flow rates (unstimulated and stimulated: USFR and SSFR, respectively). The patients were also given a validated LENT SOMA scale (LSS) questionnaire. Evaluations were performed before IMRT and at 1, 3 and 6 months after IMRT.
RESULTS
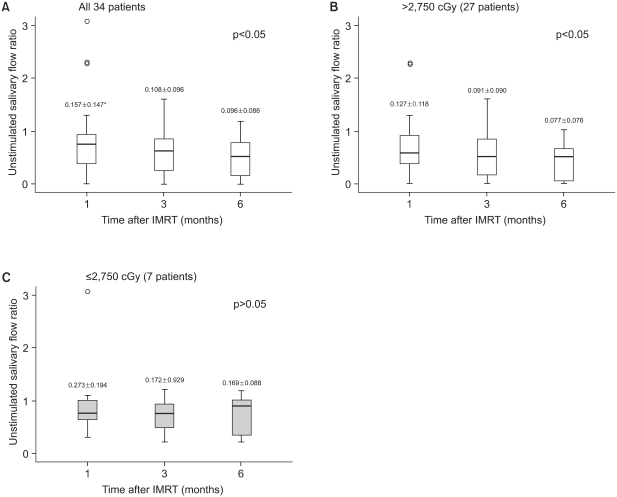
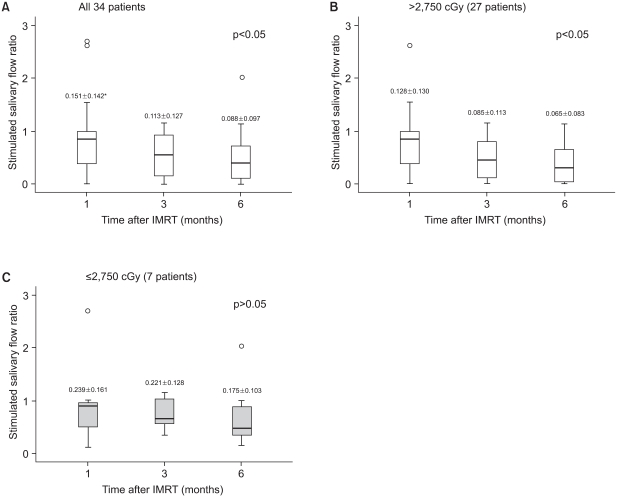
All 34 patients showed significant changes in the XQS, LSS and Salivary Flow rates (USFR and SSFR) after IMRT. No significant changes in the XQS or LSS were noted in 12 patients who received a total parotid mean dose of < or =3,100 cGy at 1, 3 and 6 months post-IMRT relative to the baseline values. However, for the 22 patients who received >3,100 cGy, significant increases in the XQS and LSS were observed. The USFR and SSFR from the parotid glands in 7 patients who received < or =2,750 cGy were significantly preserved at up to 6 months after IMRT. However, the USFR and SSFR in 27 patients who were treated with >2,750 cGy were significantly lower than the baseline values at all times after IMRT.
CONCLUSION
We suggest that the total parotid mean dose should be limited to < or =2,750 cGy to preserve the USFR and SSFR and so improve the subsequent quality of life.
MeSH Terms
Figure
Reference
-
1. Bjordal K, Kaasa S, Mastekaasa A. Quality of life in patients treated for head and neck cancer: a follow up study 7 to 11 years after radiotherapy. Int J Radiat Oncol Biol Phys. 1994; 28:847–856. PMID: 8138437.2. Harrison LB, Zelefsky MJ, Pfister DG, Carper E, Raben A, Kraus DH, et al. Detailed quality of life assessment in patients treated with primary radiotherapy for squamous cell cancer cancer of the base of tongue. Head Neck. 1997; 19:169–175. PMID: 9142514.3. Garg AK, Malo M. Manifestations and treatment of xerostomia and associated oral effects secondary to head and neck radiation therapy. J Am Dent Assoc. 1997; 128:1128–1133. PMID: 9260423.
Article4. Lim JH, Kim GE, Keum KC, Suh CO, Lee SW, Park HC, et al. Parotid gland sparing radiotherapy technique using 3-D conformal radiotherapy for nasopharyngeal carcinoma. J Korean Soc Ther Radiol Oncol. 2000; 18:1–10.5. Malouf JG, Aragon C, Henson BS, Eisbruch A, Ship JA. Influence of parotid-sparing radiotherapy on xerostomia in head, and neck cancer patients. Cancer Detect Prev. 2003; 27:305–310. PMID: 12893079.
Article6. Eisbruch A, Ten Haken RK, Kim HM, Marsh LH, Ship JA. Dose, volume and function relationships in parotid salivry glands following conformal and intensity modulated irradiation of head and neck cancer. Int J Radiat Oncol Biol Phys. 1999; 45:577–587. PMID: 10524409.7. Chao KS, Deasy JO, Markman J, Haynie J, Perez CA, Purdy JA, et al. A prospective study of salivary function sparing in patients with head and neck cancers receiving intensity-modulated or three-dimensional radiation therapy: initial results. Int J Radiat Oncol Biol Phys. 2001; 49:907–916. PMID: 11240231.8. Saarilahti K, Kouri M, Collan J, Hamalainen T, Atula T, Joensuu H, et al. Intensity modulated radiotherapy for head and neck cancer: evidence for preserved salivary gland function. Radiother Oncol. 2005; 74:251–258. PMID: 15763305.
Article9. Amosson CM, Teh BS, Van TJ, Uy N, Huang E, Mai WY, et al. Dosimetric predictors of xerostomia for head and neck cancer patients treated with the smart (simultaneous modulated accelerated radiation therapy) boost technique. Int J Radiat Oncol Biol Phys. 2003; 56:136–144. PMID: 12694832.10. Franzen L, Funegard U, Ericson T, Henriksson R. Parotid gland function during and following radiotherapy of malignancies in the head and neck. A consecutive study of salivary flow and patient discomfort. Eur J Cancer. 1992; 28:457–462. PMID: 1591063.11. Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991; 21:109–122. PMID: 2032882.
Article12. Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982; 5:649–655. PMID: 7165009.
Article13. LENT SOMA tables. Radiother Oncol. 1995; 35:17–60. PMID: 7569012.14. Eisbruch A, Kim HM, Terrell JE, Marsh LH, Dawson LA, Ship JA, et al. Xerostomia and its predictors following parotid-sparing irradiation of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2001; 50:695–704. PMID: 11395238.
Article15. Lee SH, Kim TH, Chie EK, Im HS, Im ES, Ryu JS, et al. Evaluation of xerostomia following intensity modulated radiotherapy (IMRT) for head and neck cancer patients. J Korean Soc Ther Radiol Oncol. 2004; 22:106–114.16. Cooper JS, Fu K, Marks J, Silverman S. Late effects of radia tion therapy in the head and neck region. Int J Radiat Oncol Biol Phys. 1995; 31:1141–1164. PMID: 7713779.17. Roesink JM, Moerland MA, Battermann JJ, Hordijk GJ, Terhaard CH. Quantitative dose-volume response analysis of changes in parotid gland function after radiotherapy in the head and neck region. Int J Radiat Oncol Biol Phys. 2001; 51:938–946. PMID: 11704314.18. Lyman JT. Complication probability as assessed from dose-volume histograms. Radiat Res Suppl. 1985; 8:S13–S19. PMID: 3867079.
Article19. Rubin P, Constine LS, Fajardo LF, Phillips TL, Wasserman TL, Bartelink H, et al. Late effects consensus conference: RTOG/EORTC. Radiother Oncol. 1995; 35:5–7. PMID: 7569013.20. Munter MW, Karger CP, Hoffner SG, Hof H, Thilmann C, Rudat V, et al. Evaluation of salivary gland function after treatment of head-and neck tumors with intensity modulated radiotherapy by quantitative pertechnetate scintigraphy. Int J Radiat Oncol Biol Phys. 2004; 58:175–184. PMID: 14697436.21. Guchelaar HJ, Vermes A, Meerwaldt JH. Radiation-induced xerostomia: pathophysiology, clinical course and supportive treatment. Support Care Cancer. 1997; 5:281–288. PMID: 9257424.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proton Therapy for Head and Neck Cancer: Current Clinical Applications and Future Direction
- Evaluation of Xerostomia Following Intensity Modulated Radiotherapy (IMRT) for Head and Neck Cancer Patients
- Impact of Computed Tomography Slice Thickness on Intensity Modulated Radiation Therapy Plan
- A Case of Parotid Tuberculosis Mimicking Benign Tumor of Parotid Gland
- Radiation therapy of the tumor of head and neck