Blood Res.
2014 Dec;49(4):259-264. 10.5045/br.2014.49.4.259.
Can we predict neonatal thrombocytopenia in offspring of women with idiopathic thrombocytopenic purpura?
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan. hidaka.nobuhiro.484@m.kyushu-u.ac.jp
- KMID: 2270684
- DOI: http://doi.org/10.5045/br.2014.49.4.259
Abstract
- BACKGROUND
We aimed to investigate which factors in the clinical profile of mothers with idiopathic thrombocytopenic purpura (ITP) can predict neonatal risk of thrombocytopenia.
METHODS
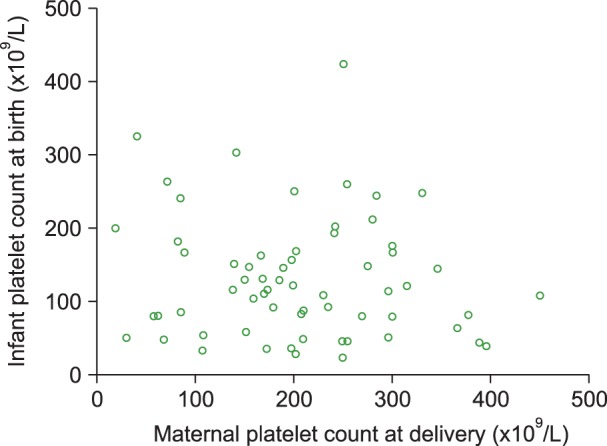
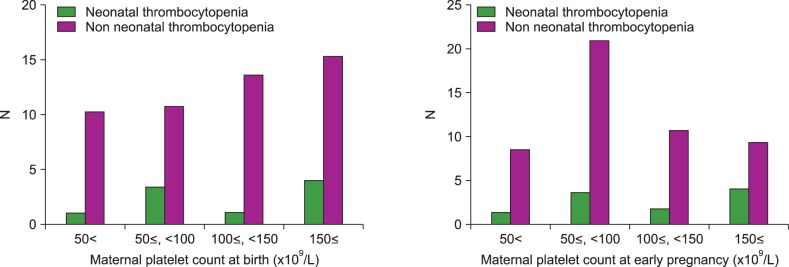
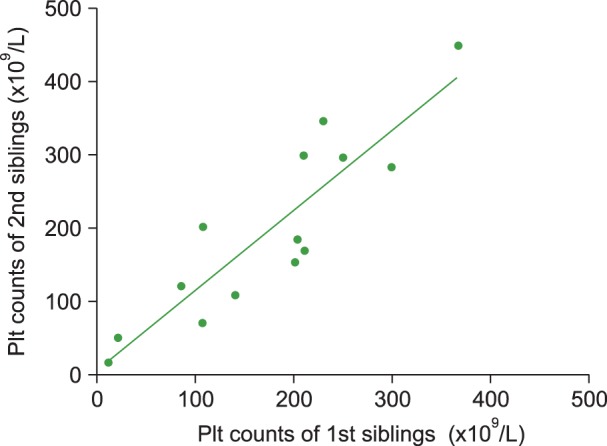
Data was retrospectively collected from all pregnant women with ITP who presented to our institution between 2001 and 2013. Neonatal offspring of these women were classified into 2 groups based on the presence or absence of neonatal thrombocytopenia (platelet count <100x109/L). Several parameters were compared between the 2 groups, including maternal age, maternal platelet count, maternal treatment history, and thrombocytopenia in siblings. We further examined the correlation between maternal platelet count at the time of delivery and neonatal platelet count at birth; we also examined the correlation between the minimum platelet counts of other children born to multiparous women.
RESULTS
Sixty-six neonates from 49 mothers were enrolled in the study. Thrombocytopenia was observed in 13 (19.7%) neonates. Maternal treatment for ITP such as splenectomy did not correlate with a risk of neonatal thrombocytopenia. Sibling thrombocytopenia was more frequently observed in neonates with thrombocytopenia than in those without (7/13 vs. 4/53, P<0.01). No association was observed between maternal and neonatal platelet counts. However, the nadir neonatal platelet counts of first- and second-born siblings were highly correlated (r=0.87).
CONCLUSION
Thrombocytopenia in neonates of women with ITP cannot be predicted by maternal treatment history or platelet count. However, the presence of an older sibling with neonatal thrombocytopenia is a reliable risk factor for neonatal thrombocytopenia in subsequent pregnancies.
MeSH Terms
Figure
Reference
-
1. Burrows RF, Kelton JG. Pregnancy in patients with idiopathic thrombocytopenic purpura: assessing the risks for the infant at delivery. Obstet Gynecol Surv. 1993; 48:781–788. PMID: 8309660.2. Payne SD, Resnik R, Moore TR, Hedriana HL, Kelly TF. Maternal characteristics and risk of severe neonatal thrombocytopenia and intracranial hemorrhage in pregnancies complicated by autoimmune thrombocytopenia. Am J Obstet Gynecol. 1997; 177:149–155. PMID: 9240599.
Article3. Debouverie O, Roblot P, Roy-Peaud F, Boinot C, Pierre F, Pourrat O. Chronic idiopathic thrombocytopenia outcome during pregnancy (62 cases). Rev Med Interne. 2012; 33:426–432. PMID: 22677087.4. Gill KK, Kelton JG. Management of idiopathic thrombocytopenic purpura in pregnancy. Semin Hematol. 2000; 37:275–289. PMID: 10942222.
Article5. Subbaiah M, Kumar S, Roy KK, Sharma JB, Singh N. Pregnancy outcome in patients with idiopathic thrombocytopenic purpura. Arch Gynecol Obstet. 2014; 289:269–273. PMID: 23852640.
Article6. Fujimura K, Harada Y, Fujimoto T, et al. Nationwide study of idiopathic thrombocytopenic purpura in pregnant women and the clinical influence on neonates. Int J Hematol. 2002; 75:426–433. PMID: 12041677.
Article7. Sukenik-Halevy R, Ellis MH, Fejgin MD. Management of immune thrombocytopenic purpura in pregnancy. Obstet Gynecol Surv. 2008; 63:182–188. PMID: 18279544.
Article8. Song TB, Lee JY, Kim YH, Choi YY. Low neonatal risk of thrombocytopenia in pregnancy associated with immune thrombocytopenic purpura. Fetal Diagn Ther. 1999; 14:216–219. PMID: 10420044.
Article9. Iyori H, Fujisawa K, Akatsuka J. Thrombocytopenia in neonates born to women with autoimmune thrombocytopenic purpura. Pediatr Hematol Oncol. 1997; 14:367–373. PMID: 9211541.10. Tampakoudis P, Bili H, Lazaridis E, Anastasiadou E, Andreou A, Mantalenakis S. Prenatal diagnosis of intracranial hemorrhage secondary to maternal idiopathic thrombocytopenic purpura: a case report. Am J Perinatol. 1995; 12:268–270. PMID: 7575833.
Article11. Koyama S, Tomimatsu T, Sawada K, et al. Prenatal diagnosis of fetal intracranial hemorrhage in pregnancy complicated by idiopathic thrombocytopenic purpura. Prenat Diagn. 2010; 30:489–491. PMID: 20440739.
Article12. Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med. 1993; 329:1463–1466. PMID: 8413457.
Article13. Yamada H, Kato EH, Kishida T, Negishi H, Makinoda S, Fujimoto S. Risk factors for neonatal thrombocytopenia in pregnancy complicated by idiopathic thrombocytopenic purpura. Ann Hematol. 1998; 76:211–214. PMID: 9671135.
Article14. Webert KE, Mittal R, Sigouin C, Heddle NM, Kelton JG. A retrospective 11-year analysis of obstetric patients with idiopathic thrombocytopenic purpura. Blood. 2003; 102:4306–4311. PMID: 12947011.
Article15. Valat AS, Caulier MT, Devos P, et al. Relationships between severe neonatal thrombocytopenia and maternal characteristics in pregnancies associated with autoimmune thrombocytopenia. Br J Haematol. 1998; 103:397–401. PMID: 9827911.
Article16. Sharon R, Tatarsky I. Low fetal morbidity in pregnancy associated with acute and chronic idiopathic thrombocytopenic purpura. Am J Hematol. 1994; 46:87–90. PMID: 8172201.
Article17. Mazzucconi MG, Petrelli V, Gandolfo GM, et al. Autoimmune thrombocytopenic purpura in pregnancy: maternal risk factors predictive of neonatal thrombocytopenia. Autoimmunity. 1993; 16:209–214. PMID: 8003616.
Article18. Koyama S, Tomimatsu T, Kanagawa T, Kumasawa K, Tsutsui T, Kimura T. Reliable predictors of neonatal immune thrombocytopenia in pregnant women with idiopathic thrombocytopenic purpura. Am J Hematol. 2012; 87:15–21. PMID: 22031338.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neonate with severe thrombocytopenia delivered from woman who has idiopathic thrombocytopenic purpura with normalized platelet count
- Maternal and neonatal outcomes in pregnancies complicated with idiopathic thrombocytopenic purpura (ITP)
- Differential diagnosis of Thrombocytopenia newly developed during pregnancy
- A Case of Antiphospholipid Syndrome Associated with Autoimmune Thrombocytopenic Purpura
- Diagnosis and treatment of purpura