Ann Surg Treat Res.
2014 Jan;86(1):22-27. 10.4174/astr.2014.86.1.22.
Low molecular-weight heparin for thromboprophylaxis in patients undergoing gastric cancer surgery: an experience from one Korean institute
- Affiliations
-
- 1Division of Gastrointestinal Surgery, Department of Surgery, The Catholic University of Korea School of Medicine, Seoul, Korea. skygs@catholic.ac.kr
- KMID: 2266902
- DOI: http://doi.org/10.4174/astr.2014.86.1.22
Abstract
- PURPOSE
This study evaluated the efficacy for preventing venous thromboembolism (VTE) and adverse effects of low-molecular-weight heparin (LMWH) in order to launch a prospective clinical trial in Korea.
METHODS
We reviewed the medical records of 108 consecutive patients who underwent gastric cancer surgery. These patients were divided into 2 groups according to the type of thromboprophylaxis: group A, LMWH combined with intermittent pneumatic compression (IPC); group B, IPC alone. The postoperative outcomes of the two groups were compared.
RESULTS
Symptomatic VTE was observed in only 1 patient (0.9%) from group B. Postoperative bleeding was more common in group A than in group B (10.9% vs. 7.5%), although the difference was not significant (P = 0.055). Most bleeding episodes were minor and managed conservatively without intervention. Only a high body mass index was associated with a significantly increased risk of postoperative bleeding (odds ratio, 1.45; 95% confidence interval, 1.12-2.43; P = 0.051).
CONCLUSION
A 40 mg of enoxaparin sodium is a safe and feasible dose for prevention of VTE. With the results of this study, we are planning a prospective randomized clinical trial to investigate the clinical efficacy of LMWH thromboprophylaxis in gastric cancer patients in Korea.
MeSH Terms
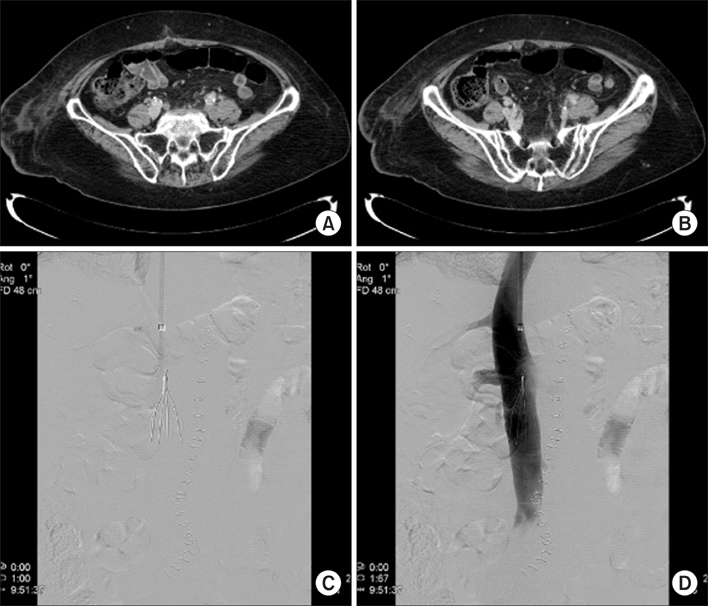
Figure
Reference
-
1. Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA Jr, et al. Prevention of venous thromboembolism. Chest. 2001; 119:1 Suppl. 132S–175S.2. Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991; 151:933–938.3. Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006; 119:60–68.4. Levitan N, Dowlati A, Remick SC, Tahsildar HI, Sivinski LD, Beyth R, et al. Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy: risk analysis using Medicare claims data. Medicine (Baltimore). 1999; 78:285–291.5. Khorana AA, Francis CW, Culakova E, Fisher RI, Kuderer NM, Lyman GH. Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol. 2006; 24:484–490.6. Lyman GH, Khorana AA, Falanga A, Clarke-Pearson D, Flowers C, Jahanzeb M, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007; 25:5490–5505.7. Jeong O, Ryu SY, Park YK, Kim YJ. The effect of low molecular weight heparin thromboprophylaxis on bleeding complications after gastric cancer surgery. Ann Surg Oncol. 2010; 17:2363–2369.8. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.9. Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126:3 Suppl. 338S–400S.10. Liew NC, Moissinac K, Gul Y. Postoperative venous thromboembolism in Asia: a critical appraisal of its incidence. Asian J Surg. 2003; 26:154–158.11. Kang MJ, Ryoo BY, Ryu MH, Koo DH, Chang HM, Lee JL, et al. Venous thromboembolism (VTE) in patients with advanced gastric cancer: an Asian experience. Eur J Cancer. 2012; 48:492–500.12. Brown A. Preventing venous thromboembolism in hospitalized patients with cancer: improving compliance with clinical practice guidelines. Am J Health Syst Pharm. 2012; 69:469–481.13. Clagett GP, Reisch JS. Prevention of venous thromboembolism in general surgical patients: results of meta-analysis. Ann Surg. 1988; 208:227–240.14. Kakkar VV, Cohen AT, Edmonson RA, Phillips MJ, Cooper DJ, Das SK, et al. The Thromboprophylaxis Collaborative Group. Low molecular weight versus standard heparin for prevention of venous thromboembolism after major abdominal surgery. Lancet. 1993; 341:259–265.15. Nurmohamed MT, Verhaeghe R, Haas S, Iriarte JA, Vogel G, van Rij AM, et al. A comparative trial of a low molecular weight heparin (enoxaparin) versus standard heparin for the prophylaxis of postoperative deep vein thrombosis in general surgery. Am J Surg. 1995; 169:567–571.16. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005; 92:1099–1102.17. Kim KH, Kim MC, Jung GJ, Kim HH. The impact of obesity on LADG for early gastric cancer. Gastric Cancer. 2006; 9:303–307.18. Bergqvist D, Burmark US, Flordal PA, Frisell J, Hallbook T, Hedberg M, et al. Low molecular weight heparin started before surgery as prophylaxis against deep vein thrombosis: 2500 versus 5000 XaI units in 2070 patients. Br J Surg. 1995; 82:496–501.19. Lechler E, Schramm W, Flosbach CW. The Prime Study Group. The venous thrombotic risk in non-surgical patients: epidemiological data and efficacy/safety profile of a low-molecular-weight heparin (enoxaparin). Haemostasis. 1996; 26:Suppl 2. 49–56.20. Sherman DG, Albers GW, Bladin C, Fieschi C, Gabbai AA, Kase CS, et al. The efficacy and safety of enoxaparin versus unfractionated heparin for the prevention of venous thromboembolism after acute ischaemic stroke (PREVAIL Study): an open-label randomised comparison. Lancet. 2007; 369:1347–1355.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Treatment of Aortic Thrombosis after Umbilical Catheterization with Low-Molecular-Weight Heparin
- Effect of standard heparin and low molecular weight heparin on fibrinolytic activity
- Prophylaxis of Venous Thromboembolism in Patients with Pancreatic Cancer
- Thromboembolism in pregnancy
- Portal vein thrombosis that successfully treated with low molecular weight heparin in acute pancreatitis