Ann Surg Treat Res.
2014 Nov;87(5):273-275. 10.4174/astr.2014.87.5.273.
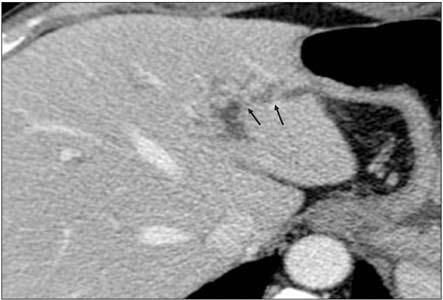
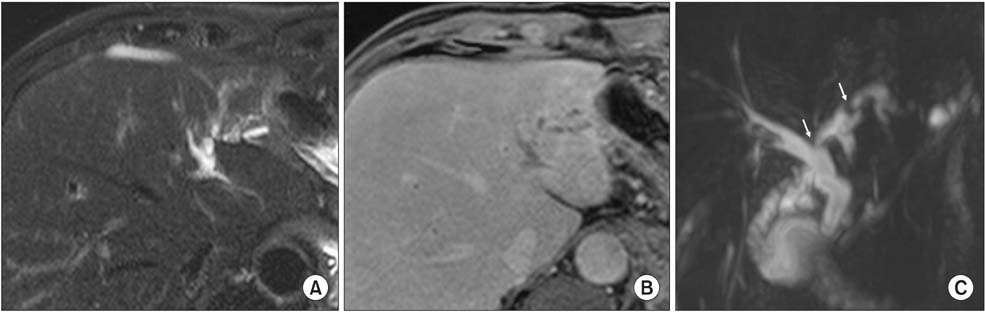
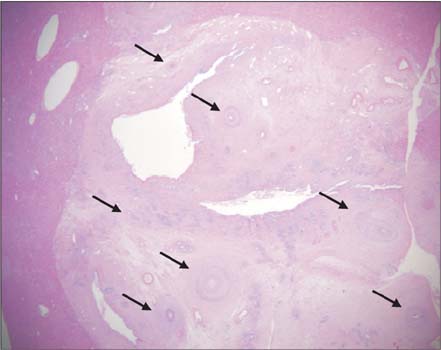
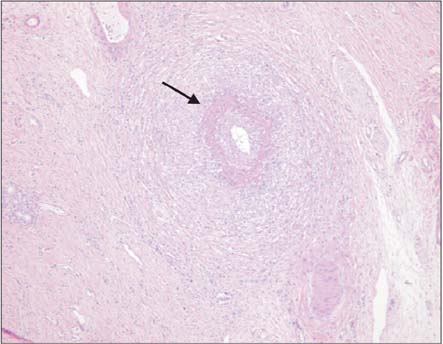
Polyarteritis nodosa presented as a dilatation of the intrahepatic bile duct
- Affiliations
-
- 1Department of Surgery, Chungbuk National University College of Medicine and Medical Research Institute, Cheongju, Korea. dhryu@chungbuk.ac.kr
- 2Department of Pathology, Chungbuk National University College of Medicine and Medical Research Institute, Cheongju, Korea.
- 3Department of Radiology, Chungbuk National University College of Medicine and Medical Research Institute, Cheongju, Korea.
- 4Department of Internal Medicine, Chungbuk National University College of Medicine and Medical Research Institute, Cheongju, Korea.
- KMID: 2266887
- DOI: http://doi.org/10.4174/astr.2014.87.5.273
Abstract
- Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis of small- and medium-sized arteries in multiorgan systems. PAN may affect the gastrointestinal tract in 14%-65% of patients, but rarely involves the biliary tract and liver. We describe a patient without underlying disease who was diagnosed with PAN during resection of the gallbladder and liver.
MeSH Terms
Figure
Reference
-
1. Parangi S, Oz MC, Blume RS, Bixon R, Laffey KJ, Perzin KH, et al. Hepatobiliary complications of polyarteritis nodosa. Arch Surg. 1991; 126:909–912.2. Ebert EC, Hagspiel KD, Nagar M, Schlesinger N. Gastrointestinal involvement in polyarteritis nodosa. Clin Gastroenterol Hepatol. 2008; 6:960–966.3. Lightfoot RW Jr, Michel BA, Bloch DA, Hunder GG, Zvaifler NJ, McShane DJ, et al. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum. 1990; 33:1088–1093.4. Guma M, Lorenzo-Zuniga V, Olive A, Perendreu J, Bechini J, Domenech E, et al. Occult liver involvement by polyarteritis nodosa. Clin Rheumatol. 2002; 21:184–186.5. Abraham S, Begum S, Isenberg D. Hepatic manifestations of autoimmune rheumatic diseases. Ann Rheum Dis. 2004; 63:123–129.6. Kitzing B, O'Toole S, Waugh A, Clayton J, McGill N, Allman KC. Hepatobiliary scintigraphy in vasculitis of the gallbladder as a manifestation of polyarteritis nodosa: a case report. Cases J. 2009; 2:9300.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Benign Biliary Stricture Complicating Isolated Polyarteritis Nodosa
- Intrahepatic Bile Duct Dilatation Caused by Pancreatic Pseudocyst: A Case Report
- Solitary intrahepatic bile-duct cyst presenting with jaundice
- A Case of Polyarteritis Nodosa Presented as Myositis
- Gelatin Sponge Particle Embolization of Spontaneously Ruptured Intrahepatic Arterial Aneurysms in a Patient with Polyarteritis Nodosa: A Case Report