Ann Rehabil Med.
2013 Aug;37(4):498-504. 10.5535/arm.2013.37.4.498.
The Location of Multifidus Atrophy in Patients With a Single Level, Unilateral Lumbar Radiculopathy
- Affiliations
-
- 1Department of Rehabilitation Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. mdlis@nate.com
- 2Champyunhan Pain and Rehabilitation Clinic, Cheongwon, Korea.
- KMID: 2266605
- DOI: http://doi.org/10.5535/arm.2013.37.4.498
Abstract
OBJECTIVE
To identify the correlations between the location of multifidus atrophy and the level of lumbar radiculopathy.
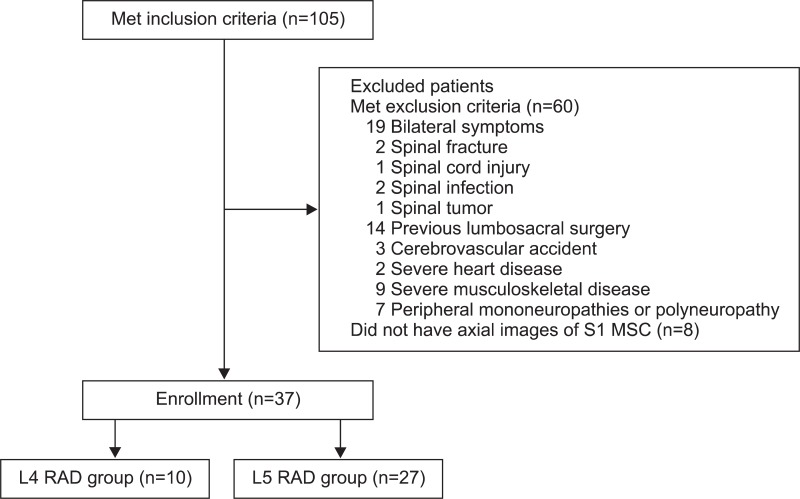
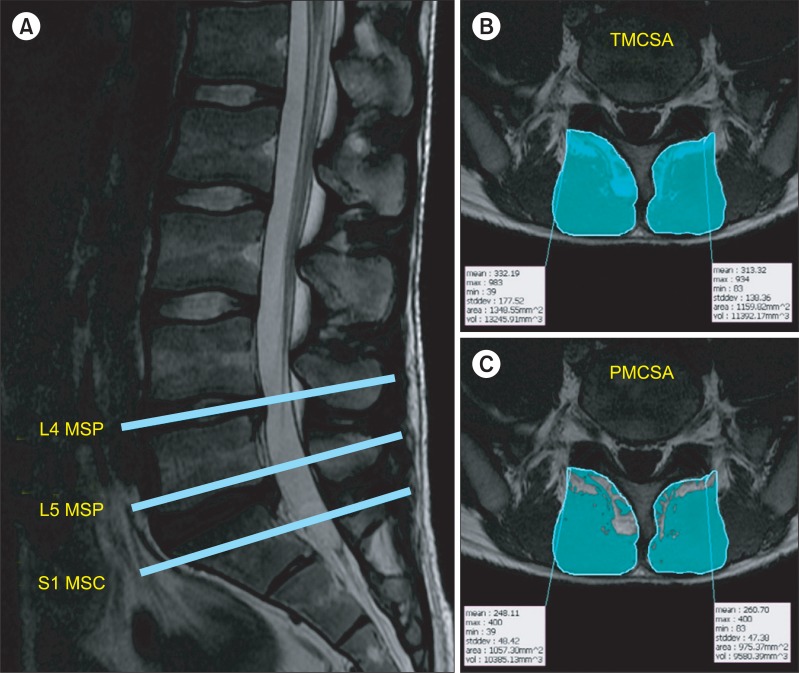
METHODS
Thirty-seven patients who had unilateral L4 or L5 radiculopathy were divided into 2 groups; the L4 radiculopathy (L4 RAD) group and the L5 radiculopathy (L5 RAD) group. Bilateral lumbar multifidus muscles at the mid-spinous process level of L4 vertebra (L4 MSP), the mid-spinous process level of L5 vertebra (L5 MSP), and the mid-sacral crest level of S1 vertebra (S1 MSC) were detected in T1 axial magnetic resonance imaging. The total muscle cross-sectional area of multifidus muscles (TMCSA) and the pure muscle cross-sectional area of multifidus muscles (PMCSA) were measured by a computerized analysis program, and the ratio of PMCSA to TMCSA (PMCSA/TMCSA) was calculated.
RESULTS
There were no significant differences in TMCSA between the involved and the uninvolved sides in both groups. PMCSA was only significantly smaller at the S1 MSC on the involved side as compared with the uninvolved side in the L5 RAD group. The ratio of PMCSA to TMCSA was the lowest at the L5 MSP on the involved side in the L4 RAD group and at the S1 MSC on the involved side in the L5 RAD group.
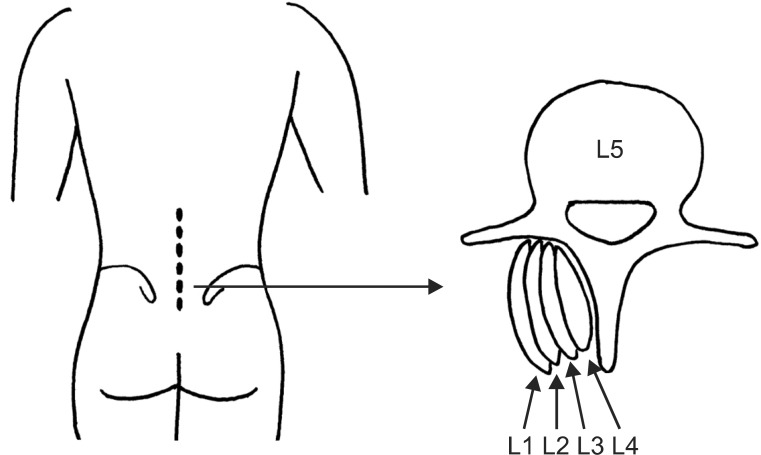
CONCLUSION
Our findings suggest that the most severe atrophy of multifidus muscle may occur at the mid-spinous process or mid-sacral crest level of the vertebra which is one level below the segmental number of the involved nerve root in patients with a single-level, unilateral lumbar radiculopathy.
MeSH Terms
Figure
Cited by 1 articles
-
Asymmetric Atrophy of Paraspinal Muscles in Patients With Chronic Unilateral Lumbar Radiculopathy
Jinmann Chon, Hee-Sang Kim, Jong Ha Lee, Seung Don Yoo, Dong Hwan Yun, Dong Hwan Kim, Seung Ah Lee, Yoo Jin Han, Hyun Seok Lee, Young Rok Han, Seonyoung Han, Yong Kim
Ann Rehabil Med. 2017;41(5):801-807. doi: 10.5535/arm.2017.41.5.801.
Reference
-
1. Kong WZ, Goel VK, Gilbertson LG, Weinstein JN. Effects of muscle dysfunction on lumbar spine mechanics: a finite element study based on a two motion segments model. . Spine (Phila Pa 1976). 1996; 21:2197–2206. PMID: 8902963.2. Parkkola R, Rytokoski U, Kormano M. Magnetic resonance imaging of the discs and trunk muscles in patients with chronic low back pain and healthy control subjects. Spine (Phila Pa 1976). 1993; 18:830–836. PMID: 8316880.
Article3. Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976). 1994; 19:165–172. PMID: 8153825.
Article4. Bae JH, Na JK, Yu JY, Park YO. Atrophy of multifidus muscle on low back pain patients. J Korean Acad Rehabil Med. 2001; 25:684–691.5. Campbell WW, Vasconcelos O, Laine FJ. Focal atrophy of the multifidus muscle in lumbosacral radiculopathy. Muscle Nerve. 1998; 21:1350–1353. PMID: 9736071.
Article6. Yoshihara K, Shirai Y, Nakayama Y, Uesaka S. Histochemical changes in the multifidus muscle in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 2001; 26:622–626. PMID: 11246373.
Article7. Hyun JK, Lee JY, Lee SJ, Jeon JY. Asymmetric atrophy of multifidus muscle in patients with unilateral lumbosacral radiculopathy. Spine (Phila Pa 1976). 2007; 32:E598–E602. PMID: 17906560.
Article8. Chae SH, Lee SJ, Kim MS, Kim TU, Hyun JK. Cervical multifidus muscle atrophy in patients with unilateral cervical radiculopathy. J Korean Acad Rehabil Med. 2010; 34:743–751.9. Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976). 1993; 18:575–581. PMID: 8484148.
Article10. Hyun SJ, Kim YB, Kim YS, Park SW, Nam TK, Hong HJ, et al. Postoperative changes in paraspinal muscle volume: comparison between paramedian interfascial and midline approaches for lumbar fusion. J Korean Med Sci. 2007; 22:646–651. PMID: 17728503.
Article11. Zhao WP, Kawaguchi Y, Matsui H, Kanamori M, Kimura T. Histochemistry and morphology of the multifidus muscle in lumbar disc herniation: comparative study between diseased and normal sides. Spine (Phila Pa 1976). 2000; 25:2191–2199. PMID: 10973402.12. Hodges P, Holm AK, Hansson T, Holm S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine (Phila Pa 1976). 2006; 31:2926–2933. PMID: 17139223.
Article13. Estlander AM, Vanharanta H, Moneta GB, Kaivanto K. Anthropometric variables, self-efficacy beliefs, and pain and disability ratings on the isokinetic performance of low back pain patients. Spine (Phila Pa 1976). 1994; 19:941–947. PMID: 8009353.
Article14. Mannion AF, Dolan P. Electromyographic median frequency changes during isometric contraction of the back extensors to fatigue. Spine (Phila Pa 1976). 1994; 19:1223–1229. PMID: 8073313.
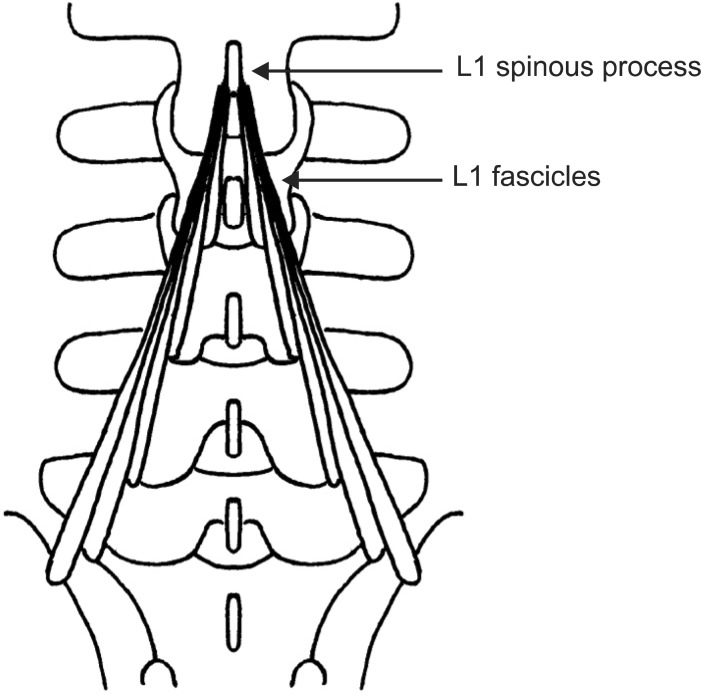
Article15. Bogduk N, Wilson AS, Tynan W. The human lumbar dorsal rami. J Anat. 1982; 134(Pt 2):383–397. PMID: 7076562.16. Macintosh JE, Valencia F, Bogduk N, Munro RR. The morphology of the human lumbar multifidus. Clin Biomech (Bristol, Avon). 1986; 1:196–204.
Article17. Haig AJ, Moffroid M, Henry S, Haugh L, Pope M. A technique for needle localization in paraspinal muscles with cadaveric confirmation. Muscle Nerve. 1991; 14:521–526. PMID: 1852159.
Article18. Haig AJ, Talley C, Grobler LJ, LeBreck DB. Paraspinal mapping: quantified needle electromyography in lumbar radiculopathy. Muscle Nerve. 1993; 16:477–484. PMID: 8390606.
Article19. Kim BJ, Date ES, Derby R, Lee SH, Seo KS, Oh KJ, et al. Electromyographic technique for lumbar multifidus examination: comparison of previous techniques used to localize the multifidus. Arch Phys Med Rehabil. 2005; 86:1325–1329. PMID: 16003658.
Article20. Kalimo H, Rantanen J, Viljanen T, Einola S. Lumbar muscles: structure and function. Ann Med. 1989; 21:353–359. PMID: 2532525.
Article21. Zhang J, Tsuzuki N, Hirabayashi S, Saiki K, Fujita K. Surgical anatomy of the nerves and muscles in the posterior cervical spine: a guide for avoiding inadvertent nerve injuries during the posterior approach. Spine (Phila Pa 1976). 2003; 28:1379–1384. PMID: 12838094.22. Lau P, Mercer S, Govind J, Bogduk N. The surgical anatomy of lumbar medial branch neurotomy (facet denervation). Pain Med. 2004; 5:289–298. PMID: 15367308.
Article23. Petersilge CA, Pathria MN, Gentili A, Recht MP, Resnick D. Denervation hypertrophy of muscle: MR features. J Comput Assist Tomogr. 1995; 19:596–600. PMID: 7622691.24. Bogduk N. A reappraisal of the anatomy of the human lumbar erector spinae. J Anat. 1980; 131(Pt 3):525–540. PMID: 7216917.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atrophy of Multifidus Muscle on Low Back Pain Patients
- Measurements of Multifidus Signal Intensity in Magnetic Resonance Imaging of the Patients with Unilateral Lumbar Radiculopathy
- Asymmetric Atrophy of Paraspinal Muscles in Patients With Chronic Unilateral Lumbar Radiculopathy
- Cervical Multifidus Muscle Atrophy in Patients with Unilateral Cervical Radiculopathy
- Changes in the Cross-Sectional Area of Multifidus and Psoas in Unilateral Sciatica Caused by Lumbar Disc Herniation