Ann Rehabil Med.
2013 Oct;37(5):628-632. 10.5535/arm.2013.37.5.628.
Factors Associated With Compliance With Viscosity-Modified Diet Among Dysphagic Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul, Korea. tairyoon@snu.ac.kr
- KMID: 2266579
- DOI: http://doi.org/10.5535/arm.2013.37.5.628
Abstract
OBJECTIVE
To investigate compliance with a viscosity-modified diet among Korean dysphagic patients and to determine which factors are associated with compliance.
METHODS
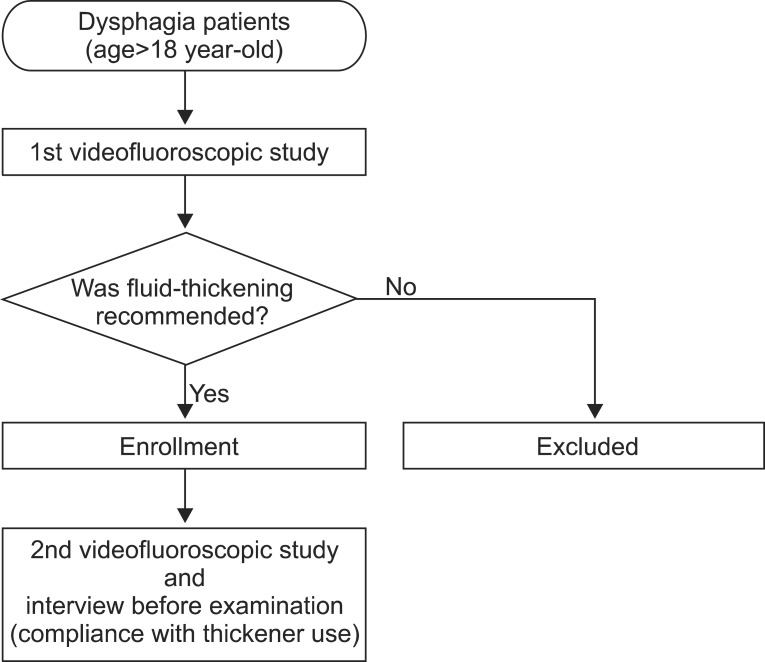
We retrospectively reviewed medical records of patients who had been recommended to use thickeners in the previous videofluoroscopic swallowing study (VFSS). Among 68 patients, 6 were excluded because tube feeding was required due to deterioration in their medical condition. Finally, 62 patients were included in the study. Patient compliance was assessed using their medical records by checking whether he or she had maintained thickener use until the next VFSS. To determine which factors affect compliance, the relationship between thickener use and patient characteristics, such as sex, age, inpatient/outpatient status, severity of dysphagia, aspiration symptoms, follow-up interval of VFSS, and current swallowing therapy status were assessed. For noncompliers, reasons for not using thickeners were investigated by telephone interview.
RESULTS
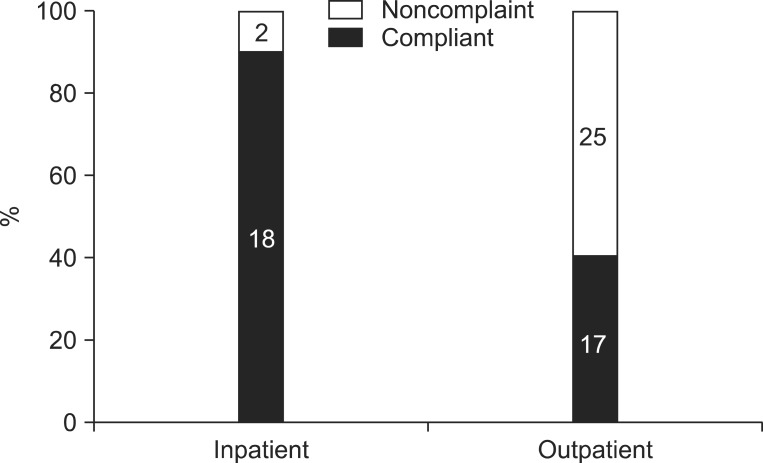
Among 62 patients, 35 (56.5%) were compliers, and 27 (43.5%) were noncompliers. Eighteen (90%) of 20 inpatients had followed previous recommendations; however, only 17 (40.5%) of 42 outpatients had been using thickeners. Of patient characteristics, only admission status was significantly correlated with compliance. When asked about the reason why they had not used thickeners, noncompliers complained about dissatisfaction with texture and taste, greater difficulty in swallowing, and inconvenience of preparing meals.
CONCLUSION
Among Korean dysphagic patients, compliance with a viscosity-modified liquid diet was only about 50%. Betterments of texture and taste along with patient education might be necessary to improve compliance with thickener use.
Keyword
MeSH Terms
Figure
Reference
-
1. Olszewski J. Causes, diagnosis and treatment of neurogenic dysphagia as an interdisciplinary clinical problem. Otolaryngol Pol. 2006; 60:491–500. PMID: 17152798.2. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012; 7:287–298. PMID: 22956864.3. Groher ME, McKaig TN. Dysphagia and dietary levels in skilled nursing facilities. J Am Geriatr Soc. 1995; 43:528–532. PMID: 7730535.
Article4. Feinberg MJ, Knebl J, Tully J, Segall L. Aspiration and the elderly. Dysphagia. 1990; 5:61–71. PMID: 2209101.
Article5. Curran J, Groher ME. Development and dissemination of an aspiration risk reduction diet. Dysphagia. 1990; 5:6–12. PMID: 2202558.
Article6. Groher ME. Bolus management and aspiration pneumonia in patients with pseudobulbar dysphagia. Dysphagia. 1987; 1:215–216.
Article7. Macqueen C, Taubert S, Cotter D, Stevens S, Frost G. Which commercial thickening agent do patients prefer? Dysphagia. 2003; 18:46–52. PMID: 12497196.
Article8. Leiter AE, Windsor J. Compliance of geriatric dysphagic patients with safe-swallowing instructions. J Med Speech Lang Pathol. 1996; 4:289–300.9. Kim DH, Choi KH, Kim HM, Koo JH, Kim BR, Kim TW, et al. Inter-rater reliability of videofluoroscopic dysphagia scale. Ann Rehabil Med. 2012; 36:791–796. PMID: 23342311.
Article10. Low J, Wyles C, Wilkinson T, Sainsbury R. The effect of compliance on clinical outcomes for patients with dysphagia on videofluoroscopy. Dysphagia. 2001; 16:123–127. PMID: 11305222.
Article11. Rosenvinge SK, Starke ID. Improving care for patients with dysphagia. Age Ageing. 2005; 34:587–593. PMID: 16267184.
Article12. King JM, Ligman K. Patient noncompliance with swallowing recommendations: reports from speech-language pathologists. Contemp Issues Commun Sci Disord. 2011; 38:53–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Compliance with Viscosity-modified Diet among Patients with Dysphagia
- Effect of Salivary Reaction Time on Flow Properties of Commercial Food Thickeners Used for Dysphagic Patients
- Efficacy of and Patient Compliance with a Ketogenic Diet in Adults with Intractable Epilepsy: A Meta-Analysis
- Principles and Considerations in the Prescription of Dysphagia Diets: Viscosity, Size, Texture, Taste and Temperature
- Viscosity Control: Effect on Pharyngeal Residue in Dysphagia Patients with Reduced Pharyngeal Constriction