Ann Dermatol.
2010 Nov;22(4):447-451. 10.5021/ad.2010.22.4.447.
Lymphomatoid Papulosis Followed by Anaplastic Large Cell Lymphoma in a Pediatric Patient
- Affiliations
-
- 1Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea. hjpark@catholic.ac.kr
- 2Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2266185
- DOI: http://doi.org/10.5021/ad.2010.22.4.447
Abstract
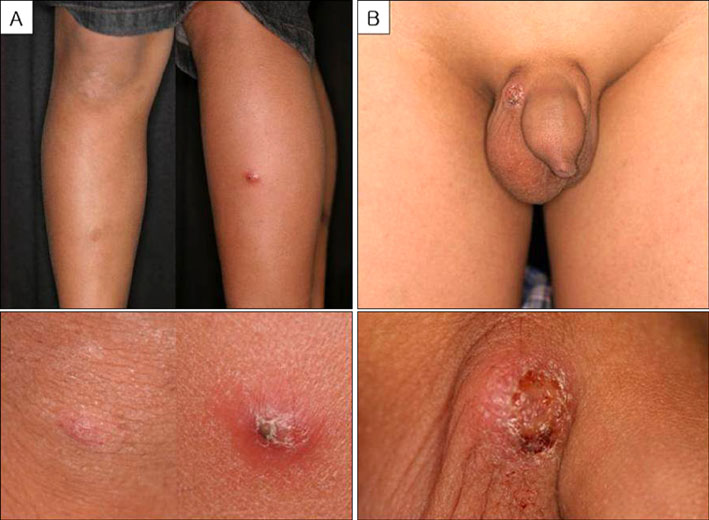
- Lymphomatoid papulosis (LyP) is a benign, self-healing, papular eruption that can wax and wane over time. Transformation to T-cell lymphoma has been well documented in 10% to 20% of adults with LyP. However, this transformation rarely occurs in patients younger than 20 years of age. Here, we present the first known pediatric patient in Korea, a 12-year-old boy who developed a subcutaneous nodule on the scrotum 13 months after papulonecrotic lesions of LyP were identified on both lower extremities and face. Histological and immunohistochemical examination of the subcutaneous nodule revealed anaplastic large cell lymphoma (ALCL). A T-cell receptor gene rearrangement analysis demonstrated an identical rearranged pattern in the two specimens, indicating that a common T-cell clone had proliferated over time in both the LyP and ALCL lesions.
MeSH Terms
Figure
Reference
-
1. Willemze R, Meyer CJ, Van Vloten WA, Scheffer E. The clinical and histological spectrum of lymphomatoid papulosis. Br J Dermatol. 1982. 107:131–144.
Article2. Kadin ME. Lymphomatoid papulosis, Ki-1+ lymphoma, and primary cutaneous Hodgkin's disease. Semin Dermatol. 1991. 10:164–171.3. Rifkin S, Valderrama E, Lipton JM, Karayalcin G. Lymphomatoid papulosis and Ki-1+ anaplastic large cell lymphoma occurring concurrently in a pediatric patient. J Pediatr Hematol Oncol. 2001. 23:321–323.
Article4. Kaudewitz P, Herbst H, Anagnostopoulos I, Eckert F, Braun-Falco O, Stein H. Lymphomatoid papulosis followed by large-cell lymphoma: immunophenotypical and genotypical analysis. Br J Dermatol. 1991. 124:465–469.
Article5. Amagai M, Kawakubo Y, Tsuyuki A, Harada R. Lymphomatoid papulosis followed by Ki-1 positive anaplastic large cell lymphoma: proliferation of a common T-cell clone. J Dermatol. 1995. 22:743–746.
Article6. Jaffe ES, Harris NL, Stein H, Isaacson PG. Classification of lymphoid neoplasms: the microscope as a tool for disease discovery. Blood. 2008. 112:4384–4399.
Article7. Bekkenk MW, Geelen FA, van Voorst Vader PC, Heule F, Geerts ML, van Vloten WA, et al. Primary and secondary cutaneous CD30(+) lymphoproliferative disorders: a report from the Dutch Cutaneous Lymphoma Group on the long-term follow-up data of 219 patients and guidelines for diagnosis and treatment. Blood. 2000. 95:3653–3661.
Article8. Diamantidis MD, Papadopoulos A, Kaiafa G, Ntaios G, Karayannopoulou G, Kostopoulos I, et al. Differential diagnosis and treatment of primary, cutaneous, anaplastic large cell lymphoma: not always an easy task. Int J Hematol. 2009. 90:226–229.
Article9. Brown JR, Skarin AT. Clinical mimics of lymphoma. Oncologist. 2004. 9:406–416.
Article10. McCarty MJ, Vukelja SJ, Sausville EA, Perry JJ, James WD, Jaffe ES, et al. Lymphomatoid papulosis associated with Ki-1-positive anaplastic large cell lymphoma. A report of two cases and a review of the literature. Cancer. 1994. 74:3051–3058.
Article11. Dawn G, Morrison A, Morton R, Bilsland D, Jackson R. Co-existent primary cutaneous anaplastic large cell lymphoma and lymphomatoid papulosis. Clin Exp Dermatol. 2003. 28:620–624.
Article12. Cerio R, Black MM. Regressing atypical histiocytosis and lymphomatoid papulosis: variants of the same disorder? Br J Dermatol. 1990. 123:515–521.
Article13. Zirbel GM, Gellis SE, Kadin ME, Esterly NB. Lymphomatoid papulosis in children. J Am Acad Dermatol. 1995. 33:741–748.
Article14. Wang HH, Myers T, Lach LJ, Hsieh CC, Kadin ME. Increased risk of lymphoid and nonlymphoid malignancies in patients with lymphomatoid papulosis. Cancer. 1999. 86:1240–1245.
Article15. Weiss LM, Wood GS, Trela M, Warnke RA, Sklar J. Clonal T-cell populations in lymphomatoid papulosis. Evidence of a lymphoproliferative origin for a clinically benign disease. N Engl J Med. 1986. 315:475–479.16. Kunishige JH, McDonald H, Alvarez G, Johnson M, Prieto V, Duvic M. Lymphomatoid papulosis and associated lymphomas: a retrospective case series of 84 patients. Clin Exp Dermatol. 2009. 34:576–581.
Article17. Tomaszewski MM, Moad JC, Lupton GP. Primary cutaneous Ki-1(CD30) positive anaplastic large cell lymphoma in childhood. J Am Acad Dermatol. 1999. 40:857–861.
Article18. Ng A, Hobson R, Williams D, Morland B. Anaplastic large cell lymphoma of bone -is it a bad tumor? Pediatr Blood Cancer. 2007. 48:473–476.19. Williams DM, Hobson R, Imeson J, Gerrard M, McCarthy K, Pinkerton CR. Anaplastic large cell lymphoma in childhood: analysis of 72 patients treated on The United Kingdom Children's Cancer Study Group chemotherapy regimens. Br J Haematol. 2002. 117:812–820.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lymphomatoid Papulosis Developed after Remission of Hodgkin's Lymphoma
- A case of lymphomatoid papulosis occurred simultaneously with Ki-1-positive anaplastic large cell lymphoma
- A Case of Lymphomatoid Papulosis Associated with Early Mycosis Fungoides
- Lymphomatoid Papulosis Following Anaplastic Large Cell Lymphoma in a Child
- Primary Cutaneous CD30+ Anaplastic Large Cell Lymphoma That Developed after Lymphomatoid Papulosis