Ann Dermatol.
2013 Aug;25(3):292-297. 10.5021/ad.2013.25.3.292.
Improvement of Atopic Dermatitis Severity after Reducing Indoor Air Pollutants
- Affiliations
-
- 1Department of Dermatology, Kangnam Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea. dermap@paran.com
- KMID: 2265867
- DOI: http://doi.org/10.5021/ad.2013.25.3.292
Abstract
- BACKGROUND
Recent epidemiologic studies have shown that environmental contaminants such as air pollution and tobacco smoke play an important role in the pathophysiology of atopic dermatitis (AD).
OBJECTIVE
The aim of this study was to evaluate the relationship between the severity of AD and indoor air pollution.
METHODS
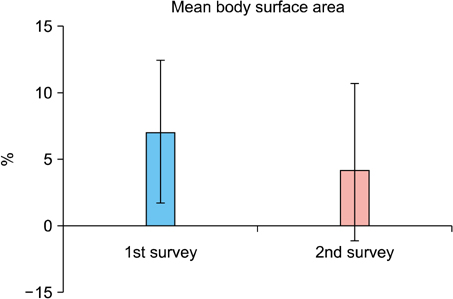
The study population consisted of 425 children from 9 kindergartens, Korea. The authors surveyed the prevalence of AD and evaluated disease severity by the eczema area and severity index (EASI) score and investigator's global assessment (IGA). After measuring indoor air pollution, a program to improve indoor air quality was conducted in 9 kindergartens. Seven months later, the prevalence and disease severity were evaluated.
RESULTS
The initial prevalence of AD was 8% and the mean EASI score was 2.37. The levels of particulate material 10 (PM10) and carbon dioxide (CO2) were higher in some kindergartens compared to the normal values. Subsequent to the completion of the indoor air quality improvement program, the mean PM10 level was significantly decreased from 182.7 to 73.4 microg/m3. After the completion of the program, the prevalence of AD and the mean EASI were decreased, and the changes were both statistically significant. The mean number of hospital visits decreased from 1.3 per month during the first survey to 0.7 per month during the second survey, which was statistically significant.
CONCLUSION
Indoor air pollution could be related to AD. The reduction of PM10 through improving indoor air quality should be considered in kindergartens and schools in order to prevent and relieve AD in children.
MeSH Terms
Figure
Cited by 2 articles
-
Association between green areas and allergic disease in Korean adults: a cross-sectional study
Hyun-Jin Kim, Jin-young Min, Hye-Jin Kim, Kyoung-bok Min
Ann Occup Environ Med. 2020;32(1):. doi: 10.35371/aoem.2020.32.e5.Indoor air pollutants and atopic dermatitis in socioeconomically disadvantaged children
Sung Chul Seo, In Soon Kang, Soo Gil Lim, Ji Tae Choung, Young Yoo
Allergy Asthma Respir Dis. 2015;3(3):206-212. doi: 10.4168/aard.2015.3.3.206.
Reference
-
1. Kay J, Gawkrodger DJ, Mortimer MJ, Jaron AG. The prevalence of childhood atopic eczema in a general population. J Am Acad Dermatol. 1994; 30:35–39.
Article2. Aberg N, Engström I, Lindberg U. Allergic diseases in Swedish school children. Acta Paediatr Scand. 1989; 78:246–252.
Article3. Kilpeläinen M, Terho EO, Helenius H, Koskenvuo M. Farm environment in childhood prevents the development of allergies. Clin Exp Allergy. 2000; 30:201–208.
Article4. McNally NJ, Williams HC, Phillips DR, Strachan DP. Is there a geographical variation in eczema prevalence in the UK? Evidence from the 1958 British Birth Cohort Study. Br J Dermatol. 2000; 142:712–720.
Article5. Riedler J, Eder W, Oberfeld G, Schreuer M. Austrian children living on a farm have less hay fever, asthma and allergic sensitization. Clin Exp Allergy. 2000; 30:194–200.
Article6. Wen HJ, Chen PC, Chiang TL, Lin SJ, Chuang YL, Guo YL. Predicting risk for early infantile atopic dermatitis by hereditary and environmental factors. Br J Dermatol. 2009; 161:1166–1172.
Article7. Arnedo-Pena A, García-Marcos L, Carvajal Urueña I, Busquets Monge R, Morales Suárez-Varela M, Miner Canflanca I, et al. Air pollution and recent symptoms of asthma, allergic rhinitis, and atopic eczema in schoolchildren aged between 6 and 7 years. Arch Bronconeumol. 2009; 45:224–229.
Article8. Park YL, Kim HD, Kim KH, Kim MN, Kim JW, Ro YS, et al. A study on the diagnostic criteria of Korean atopic dermatitis. Korean J Dermatol. 2006; 44:659–663.9. Gelmetti C, Colonna C. The value of SCORAD and beyond. Towards a standardized evaluation of severity? Allergy. 2004; 59:Suppl 78. 61–65.
Article10. Kim JH, Lee KM, Koh SB, Kim SH, Choi EH. Effect of polyurushiol paint on indoor air quality and atopic dermatitis. Korean J Dermatol. 2010; 48:198–205.11. Moon KW, Byeon SH, Choi DW, Lee EI, Oh EH, Kim YW. Risk assessment of aldehydes in some residential indoor air included atopy patient's homes. Korean J Environ Toxicol. 2006; 32:19–26.12. Hägerhed-Engman L, Sigsgaard T, Samuelson I, Sundell J, Janson S, Bornehag CG. Low home ventilation rate in combination with moldy odor from the building structure increase the risk for allergic symptoms in children. Indoor Air. 2009; 19:184–192.
Article13. Dockery DW, Pope CA 3rd, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993; 329:1753–1759.
Article14. Logan WP. Mortality in the London fog incident, 1952. Lancet. 1953; 1:336–338.
Article15. Dockery DW, Pope CA 3rd. Acute respiratory effects of particulate air pollution. Annu Rev Public Health. 1994; 15:107–132.
Article16. Schwartz J, Slater D, Larson TV, Pierson WE, Koenig JQ. Particulate air pollution and hospital emergency room visits for asthma in Seattle. Am Rev Respir Dis. 1993; 147:826–831.
Article17. Kim JH, Jeon HK, Kim MK, Kyung SY, An CH, Lee SP, et al. Particulate matter from Asian dust storms induces the expression of proinflammatory cytokine in A549 epithelial cells. Tuberc Respir Dis. 2006; 60:663–672.
Article18. Li TZ, Lee SJ, Park SJ, Chang BJ, Lee JH, Kim KS, et al. The effects of air-borne particulate matters on the alveolar macrophages for the TNF-α and IL-1β secretion. Tuberc Respir Dis. 2006; 60:554–563.
Article19. Sharma HP, Hansel NN, Matsui E, Diette GB, Eggleston P, Breysse P. Indoor environmental influences on children's asthma. Pediatr Clin North Am. 2007; 54:103–120.
Article20. Annesi-Maesano I, Moreau D, Caillaud D, Lavaud F, Le Moullec Y, Taytard A, et al. Residential proximity fine particles related to allergic sensitisation and asthma in primary school children. Respir Med. 2007; 101:1721–1729.
Article21. Salvi S. Health effects of ambient air pollution in children. Paediatr Respir Rev. 2007; 8:275–280.
Article22. Persily AK. Relationship between indoor air quality and carbon dioxide. In : Proceeding of the Indoor Air Quality and Climate, 7th International Conference; 1996 Jul 21-26; Nagoya, Japan. 1996.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of air purifier on indoor air quality and atopic dermatitis
- Indoor air pollutants and atopic dermatitis in socioeconomically disadvantaged children
- The Effect of Environmentally Friendly Wallpaper and Flooring Material on Indoor Air Quality and Atopic Dermatitis: A Pilot Study
- The clinical effects of hospitalization in a low pollutant room on atopic dermatitis
- Effect of the indoor environment on atopic dermatitis in children