Ann Dermatol.
2010 May;22(2):241-244. 10.5021/ad.2010.22.2.241.
Chemical Leukoderma Improved by Low-dose Steroid Pulse Therapy
- Affiliations
-
- 1Department of Dermatology, Seoul National University College of Medicine, Seoul, Korea. hceun@snu.ac.kr
- KMID: 2265407
- DOI: http://doi.org/10.5021/ad.2010.22.2.241
Abstract
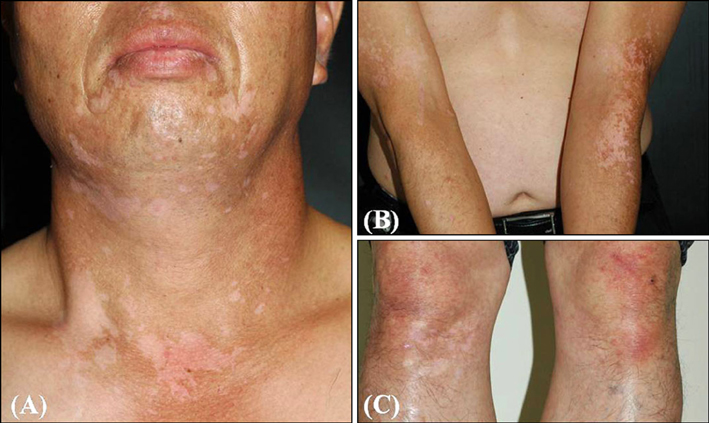
- Chemical leukoderma occurs due to the toxic effect of a specific chemical preceding allergic contact dermatitis. The mechanism is either destruction or inhibition of melanocytes by the offending substance. Clinicohistopathologically, no absolute criteria can differentiate chemical leukoderma from vitiligo. However, chemical leukoderma can be diagnosed clinically by a history of repeated exposure to a known or suspected depigmenting agent at the primary site. There is no agreed treatment guideline for chemical leukoderma. We report a healthy 51-year-old man who had multiple hypopigmented macules and patches on his face, neck, arms and legs after exposure to occupationally related chemicals. The lesions were recalcitrant to topical corticosteroids, but they showed much improvement after 3 cycles of systemic steroid pulse therapy. We suggest this therapy may be a good treatment option for chemical leukoderma.
Keyword
MeSH Terms
Figure
Reference
-
1. Ghosh S, Mukhopadhyay S. Chemical leucoderma: a clinicoaetiological study of 864 cases in the perspective of a developing country. Br J Dermatol. 2009. 160:40–47.
Article2. Boissy RE, Manga P. On the etiology of contact/occupational vitiligo. Pigment Cell Res. 2004. 17:208–214.
Article3. Oliver EA, Schwartz L, Warren LH. Occupational leukoderma: preliminary report. J Am Med Assoc. 1939. 113:927–928.4. Gellin GA, Possick PA, Davis IH. Occupational depigmentation due to 4-tertiarybutyl catechol (TBC). J Occup Med. 1970. 12:386–389.5. Kahn G. Depigmentation caused by phenolic detergent germicides. Arch Dermatol. 1970. 102:177–187.
Article6. Malten KE, Seutter E, Hara I, Nakajima T. Occupational vitiligo due to paratertiary butylphenol and homologues. Trans St Johns Hosp Dermatol Soc. 1971. 57:115–134.7. Ahn YS, Kim DH, Lee JY, Kim HO. Characteristics of occupational skin diseases compensated with the industrial accident compensation insurance from 1999 to 2003. Korean J Dermatol. 2005. 43:331–341.8. Kumar A, Freeman S. Leukoderma following occupational allergic contact dermatitis. Contact Dermatitis. 1999. 41:94–98.
Article9. Dell'anna ML, Picardo M. A review and a new hypothesis for non-immunological pathogenetic mechanisms in vitiligo. Pigment Cell Res. 2006. 19:406–411.10. Gauthier Y, Cario Andre M, Taieb A. A critical appraisal of vitiligo etiologic theories. Is melanocyte loss a melanocytorrhagy? Pigment Cell Res. 2003. 16:322–332.
Article11. Gawkrodger DJ, Ormerod AD, Shaw L, Mauri-Sole I, Whitton ME, Watts MJ, et al. Guideline for the diagnosis and management of vitiligo. Br J Dermatol. 2008. 159:1051–1076.
Article12. Lee Y, Seo YJ, Lee JH, Park JK. Therapeutic effect of the combination of high-dose methylprednisolone pulse therapy and PUVA in vitiligo patients. Korean J Dermatol. 2006. 44:288–294.13. Radakovic-Fijan S, Furnsinn-Friedl AM, Honigsmann H, Tanew A. Oral dexamethasone pulse treatment for vitiligo. J Am Acad Dermatol. 2001. 44:814–817.
Article14. Kim SM, Lee HS, Hann SK. The efficacy of low-dose oral corticosteroids in the treatment of vitiligo patients. Int J Dermatol. 1999. 38:546–550.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Chemical Leukoderma (Occupational Vitiligo) Caused by p-tert-butylphenol (PTBP)
- Steroid Psychosis
- 13 Cases of Leukoderma Punctata after Narrowband UVB Therapy in Vitiligo Patients
- Treatment of Laser Therapy-Induced Punctate Leukoderma Using a 308-nm Excimer Laser
- Methylprednisolone pulse therapy for critically ill patients with COVID-19: a cohort study