Ann Dermatol.
2010 Aug;22(3):362-366. 10.5021/ad.2010.22.3.362.
Chromoblastomycosis Caused by Phialophora richardsiae
- Affiliations
-
- 1Department of Dermatology, Gachon University of Medicine and Science, Gil Medical Center, Incheon, Korea. jyroh1@gilhospital.com
- 2Department of Laboratory Medicine, Gachon University of Medicine and Science, Gil Medical Center, Incheon, Korea.
- KMID: 2265378
- DOI: http://doi.org/10.5021/ad.2010.22.3.362
Abstract
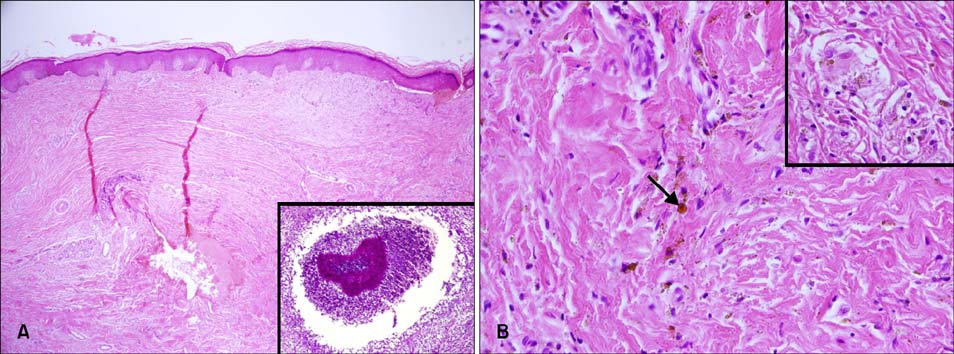
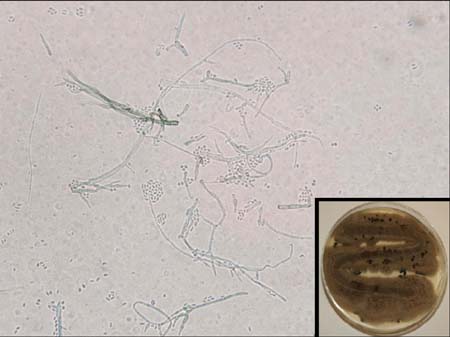
- Chromoblastomycosis is a chronic fungal disease of the skin and subcutaneous tissues caused by a group of dematiaceous (black) fungi. The most common etiologic agents are Fonsecaea pedrosoi and Cladophialophora carrionii, both of which can be isolated from plant debris. The infection usually follows traumatic inoculation by a penetrating thorn or splinter wound. Several months after the injury, painless papules or nodules appear on the affected area; these papules then progress to scaly and verrucose plaques. We report a case of chromoblastomycosis caused by Phialophora richardsiae, which has been rarely associated with chromoblastomycosis. The case involved a 43-year-old male, who for the past 2 months had noted an erythematous, pustulous plaque that was somewhat dark brown in color on his right shin; the plaque also had intermittent purulent discharge and crust formation. On histopathological examination, chronic granulomatous inflammation and sclerotic cells were seen. The tissue fungus culture grew out the typical black fungi of P. richardsiae, which was confirmed by polymerase chain reaction. The patient has been treated with a combination of terbinafine and itraconazole for 3 months with a good clinical response.
MeSH Terms
Figure
Reference
-
1. Hay RJ. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Deep fungal infections. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1833–1834.
Article2. James WD, Berger TG, Elston DM. Andrews' diseases of the skin: clinical dermatology. 2006. 10th ed. Philadelphia: Saunders Elsevier;323–324.3. Elder DE, Elenitsas R, Johnson BL Jr, Murphy GF, Xu X. Lever's histopathology of the skin. 2009. 10th ed. Philadelphia: Lippincott-Raven;607–608.4. Kim HU, Son GY, Ihm CW. A case of chromoblastomycosis showing a good response to itraconazole. Ann Dermatol. 1997. 9:51–54.
Article5. Suh MK, Sung YO, Yoon KS, Ha GY, Kim JR. A case of chromoblastomycosis caused by Fonsecaea pedrosoi. Korean J Dermatol. 1996. 34:832–836.6. López Martínez R, Méndez Tovar LJ. Chromoblastomycosis. Clin Dermatol. 2007. 25:188–194.
Article7. Minotto R, Bernardi CD, Mallmann LF, Edelweiss MI, Scroferneker ML. Chromoblastomycosis: a review of 100 cases in the state of Rio Grande do Sul, Brazil. J Am Acad Dermatol. 2001. 44:585–592.
Article8. Salgado CG, da Silva MB, Yamano SS, Salgado UI, Diniz JA, da Silva JP. Cutaneous localized annular chromoblastomycosis. J Cutan Pathol. 2009. 36:257–261.
Article9. Brandt ME, Warnock DW. Epidemiology, clinical manifestations, and therapy of infections caused by dematiaceous fungi. J Chemother. 2003. 15:Suppl 2. 36–47.
Article10. De Hoog GS, Queiroz-Telles F, Haase G, Fernandez-Zeppenfeldt G, Attili Angelis D, Gerrits Van Den Ende AH, et al. Black fungi: clinical and pathogenic approaches. Med Mycol. 2000. 38:Suppl 1. 243–250.
Article11. Vicente VA, Attili-Angelis D, Pie MR, Queiroz-Telles F, Cruz LM, Najafzadeh MJ, et al. Environmental isolation of black yeast-like fungi involved in human infection. Stud Mycol. 2008. 61:137–144.
Article12. Kimura M, Goto A, Furuta T, Satou T, Hashimoto S, Nishimura K. Multifocal subcutaneous phaeohyphomycosis caused by Phialophora verrucosa. Arch Pathol Lab Med. 2003. 127:91–93.
Article13. Pitrak DL, Koneman EW, Estupinan RC, Jackson J. Phialophora richardsiae infection in humans. Rev Infect Dis. 1988. 10:1195–1203.
Article14. Ikai K, Tomono H, Watanabe S. Phaeohyphomycosis caused by Phialophora richardsiae. J Am Acad Dermatol. 1988. 19:478–481.
Article15. Lieb DF, Smiddy WE, Miller D, Cooperman EW. Case report: Fungal endophthalmitis caused by Phialophora richardsiae. Retina. 2003. 23:406–407.16. Guého E, Bonnefoy A, Luboinski J, Petit JC, de Hoog GS. Subcutaneous granuloma caused by Phialophora richardsiae: case report and review of the literature. Mycoses. 1989. 32:219–223.
Article17. Ranawaka RR, Amarasinghe N, Hewage D. Chromoblastomycosis: combined treatment with pulsed itraconazole therapy and liquid nitrogen cryotherapy. Int J Dermatol. 2009. 48:397–400.
Article18. Bonifaz A, Saúl A, Paredes-Solis V, Araiza J, Fierro-Arias L. Treatment of chromoblastomycosis with terbinafine: experience with four cases. J Dermatolog Treat. 2005. 16:47–51.
Article19. Xibao Z, Changxing L, Quan L, Yuqing H. Treatment of chromoblastomycosis with terbinafine: a report of four cases. J Dermatolog Treat. 2005. 16:121–124.
Article20. Kumarasinghe SP, Kumarasinghe MP. Itraconazole pulse therapy in chromoblastomycosis. Eur J Dermatol. 2000. 10:220–222.