Ann Dermatol.
2010 Aug;22(3):341-345. 10.5021/ad.2010.22.3.341.
Three Cases of Primary Inoculation Tuberculosis as a Result of Illegal Acupuncture
- Affiliations
-
- 1Department of Dermatology, CHA Bundang Medical Center, CHA University, Seongnam, Korea. msch11@hanmail.net
- KMID: 2265373
- DOI: http://doi.org/10.5021/ad.2010.22.3.341
Abstract
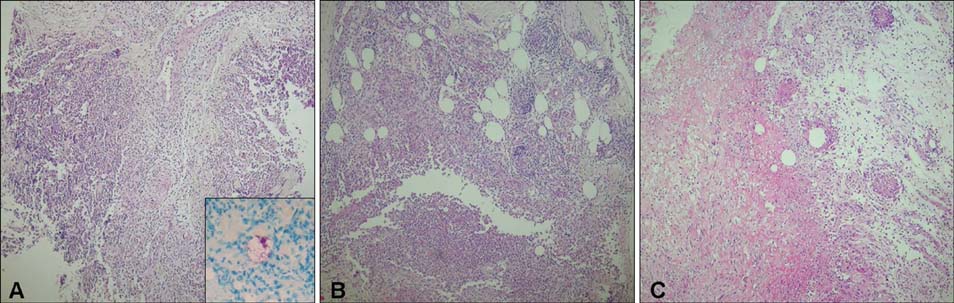
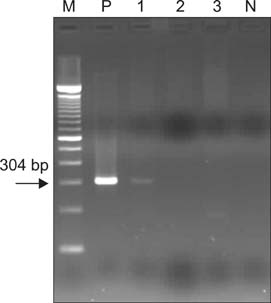
- Primary inoculation tuberculosis results from the direct inoculation of Mycobacterium tuberculosis into the skin of a person who has no natural or artificially acquired immunity to the organism. The pathogenesis requires a break in the skin from an abrasion or injury that allows entry of the tubercle bacilli. We report 3 cases of primary inoculation tuberculosis resulting from illegal acupuncture. Three patients over 70 years old presented with erythematous, ulcerative, indurated plaques on the back. Skin lesions had developed at the acupuncture sites 1 or 2 weeks after a session of acupuncture, which was intended to relieve back pain. An unlicensed, non-medically trained person conducted each session. The patients' past medical and family histories were unremarkable. Granulomatous inflammatory infiltration and acid-fast bacilli were observed histologically. M. tuberculosis was identified by mycobacterial culture and polymerase chain reaction. Nine months after the initiation of antituberculosis medication, skin lesions improved, and no evidence of recurrence or other organ involvement was observed at the 1-year follow-up visit.
MeSH Terms
Figure
Cited by 1 articles
-
Hemoperitoneum Resulting From Injuries to Liver with a Benign Vascular Tumor During Acupuncture: A Case Report
Sohyung Park, Han Young Lee
Korean J Leg Med. 2012;36(1):107-110. doi: 10.7580/KoreanJLegMed.2012.36.1.107.
Reference
-
1. Kim SW, Kim HU, Lee CJ. Korean Dermatological Association. Tuberculosis of the skin. Dermatology. 2001. 4th ed. Seoul: Yeomungak;292–293.2. Wong HW, Tay YK, Sim CS. Papular eruption on a tattoo: a case of primary inoculation tuberculosis. Australas J Dermatol. 2005. 46:84–87.
Article3. Lew W, Kim SM, Lee KH. Unusual skin tuberculosis following BCG vaccination. Korean J Dermatol. 1990. 28:349–352.4. Kim JC, Park YM, Choi JS, Kim KH. A case of primary inoculation tuberculosis developed after intralesional injection of corticosteroid. Korean J Dermatol. 1991. 29:827–831.5. You DO, Youn NH, Park SD. A case of primary inoculation tuberculosis. Korean J Dermatol. 2002. 40:1139–1141.6. Kim MG, Kim JA, Kim WS, Lee DY, Lee ES. A case of primary inoculation tuberculosis. Korean J Dermatol. 2006. 44:94–96.7. Woo PC, Lau SK, Wong SS, Yuen KY. Staphylococcus aureus subcutaneous abscess complicating acupuncture: need for implementation of proper infection control guidelines. New Microbiol. 2003. 26:169–174.8. Woo PC, Leung KW, Wong SS, Chong KT, Cheung EY, Yuen KY. Relatively alcohol-resistant mycobacteria are emerging pathogens in patients receiving acupuncture treatment. J Clin Microbiol. 2002. 40:1219–1224.
Article9. Ho CK, Ho MH, Chong LY. Cutaneous tuberculosis in Hong Kong: an update. Hong Kong Med J. 2006. 12:272–277.10. Tapias L, Tapias-Vargas LF, Tapias-Vargas L. Primary cutaneous inoculation tuberculosis in a healthcare worker as a result of a surgical accident. Int J Dermatol. 2008. 47:833–835.
Article11. Tappeiner G. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Tuberculosis and infection with atypical mycobacteria. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1768–1778.12. Bhambri S, Bhambri A, Del Rosso JQ. Atypical mycobacterial cutaneous infections. Dermatol Clin. 2009. 27:63–73.
Article13. Cheng VC, Yew WW, Yuen KY. Molecular diagnostics in tuberculosis. Eur J Clin Microbiol Infect Dis. 2005. 24:711–720.
Article14. Gawkrodger DJ. Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Mycobacterial infections. Rook/Wilkinson/Ebling textbook of dermatology. 1998. 6th ed. Oxford: Blackwell Science;1181–1214.