Ann Dermatol.
2015 Apr;27(2):163-170. 10.5021/ad.2015.27.2.163.
Inflammatory Cytokine Expression and Sebum Production after Exposure of Cultured Human Sebocytes to Ultraviolet A Radiation and Light at Wavelengths of 650 nm and 830 nm
- Affiliations
-
- 1Department of Dermatology, Kyungpook National University School of Medicine, Daegu, Korea. weonju@knu.ac.kr
- 2Tuldream Hair Clinic, Seoul, Korea.
- KMID: 2264805
- DOI: http://doi.org/10.5021/ad.2015.27.2.163
Abstract
- BACKGROUND
The effectiveness of ultraviolet (UV) radiation, visible light, or infrared light therapy for the treatment of acne is the subject of ongoing scientific debate.
OBJECTIVE
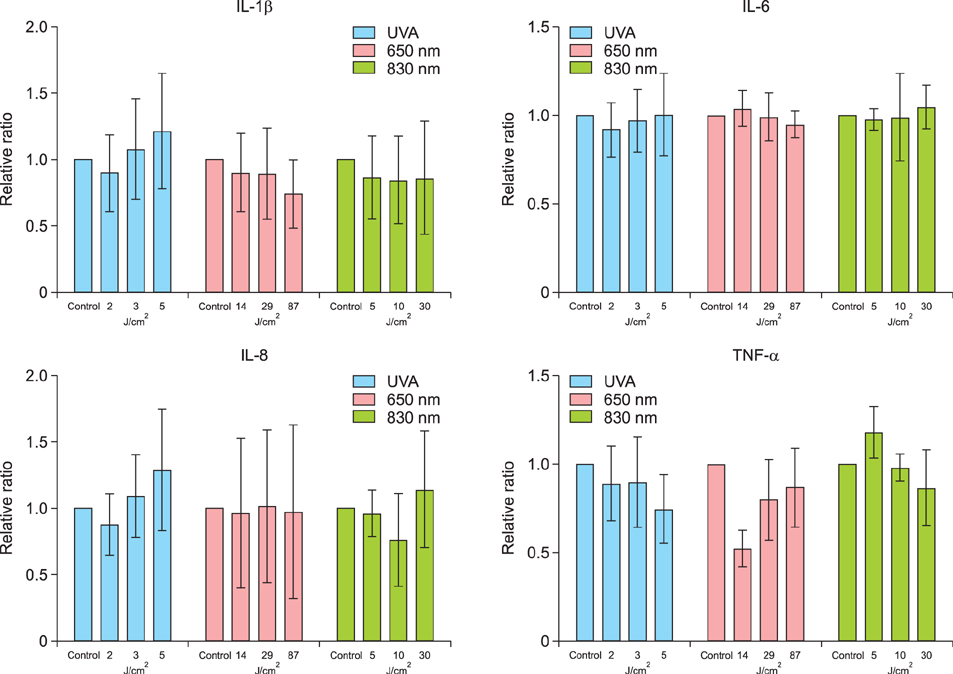
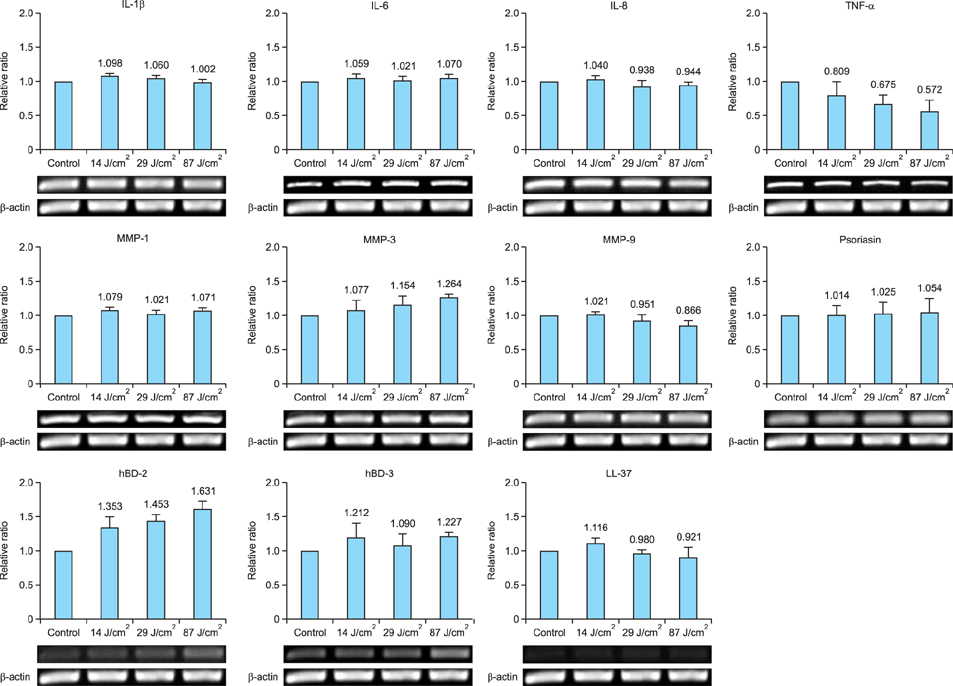
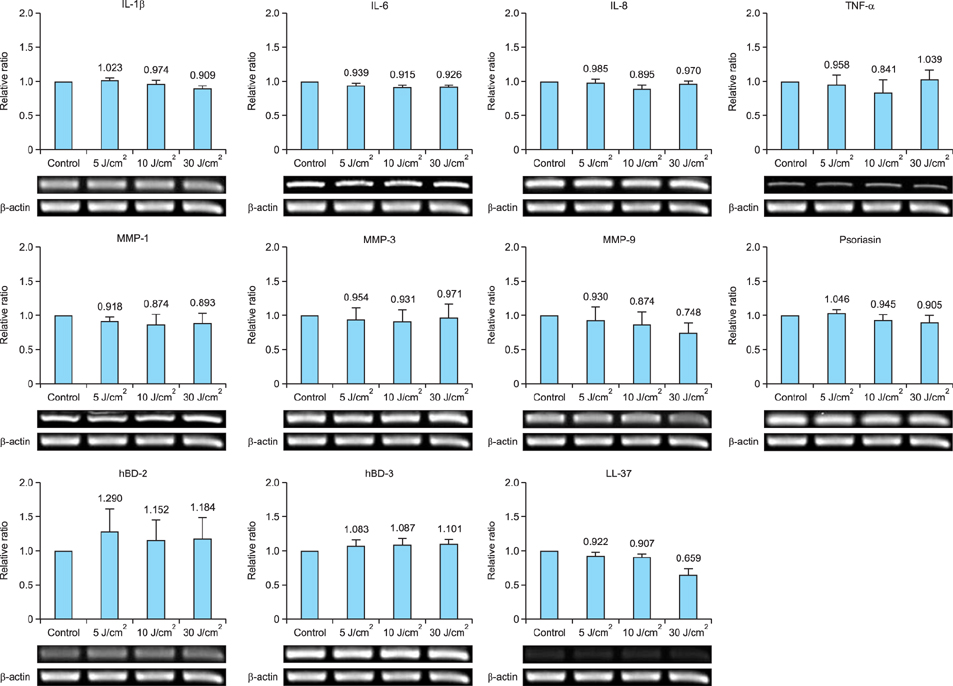
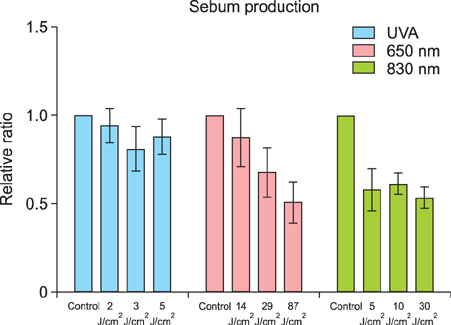
This study was conducted to investigate changes in sebum production and the expression of inflammatory cytokines, matrix metalloproteinases (MMPs), and antimicrobial peptides (AMPs), following exposure of cultured human sebocytes to UVA radiation and light at wavelengths of 650 nm and 830 nm.
METHODS
Reverse transcription polymerase chain reaction assays were performed to measure the gene expression levels of inflammatory cytokines (interleukin [IL]-1beta, IL-6, IL-8, and tumor necrosis factor-alpha), MMPs (MMP-1, MMP-3, and MMP-9), and AMPs (psoriasin, hBD-2, hBD-3, and LL-37) in cultured sebocytes after exposure to UVA radiation (2 J/cm2, 3 J/cm2, and 5 J/cm2) and light at wavelengths of 650 nm (14 J/cm2, 29 J/cm2, and 87 J/cm2) and 830 nm (5 J/cm2, 10 J/cm2, and 30 J/cm2). Expression of inflammatory cytokine proteins and sebum production were measured using enzyme-linked immunoassays and a lipid analysis kit, respectively.
RESULTS
Exposure of cultured sebocytes to UVA radiation and light at wavelengths of 650 nm and 830 nm did not show a significant increase in the expression of inflammatory cytokines, MMPs, or AMPs. Sebum production was not significantly decreased after exposure to UVA radiation and light at both wavelengths.
CONCLUSION
We propose that UVA radiation, visible light, and infrared light can be used to target Propionibacterium acnes for the treatment of acne, without an increase in the expression of inflammatory biomarkers and sebum production.
MeSH Terms
Figure
Cited by 3 articles
-
Effect of Vitamin D on the Expression of Inflammatory Biomarkers in Cultured Sebocytes Treated with Propionibacterium acnes or Ultraviolet B Irradiation
Weon Ju Lee, Min Ji Kim, Hyo Sub Ryu, Mi Yeung Sohn, Yong Hyun Jang, Seok-Jong Lee, Do Won Kim
Ann Dermatol. 2016;28(5):665-669. doi: 10.5021/ad.2016.28.5.665.Insulin-Like Growth Factor-1 Increases the Expression of Inflammatory Biomarkers and Sebum Production in Cultured Sebocytes
Hyojin Kim, Sun Young Moon, Mi Yeung Sohn, Weon Ju Lee
Ann Dermatol. 2017;29(1):20-25. doi: 10.5021/ad.2017.29.1.20.Analysis of Serum Cytokine Profile in Pemphigus
Sang Hee Lee, Won Jin Hong, Soo-Chan Kim
Ann Dermatol. 2017;29(4):438-445. doi: 10.5021/ad.2017.29.4.438.
Reference
-
1. Mills OH, Porte M, Kligman AM. Enhancement of comedogenic substances by ultraviolet radiation. Br J Dermatol. 1978; 98:145–150.
Article2. Mills OH, Kligman AM. Ultraviolet phototherapy and photochemotherapy of acne vulgaris. Arch Dermatol. 1978; 114:221–223.
Article3. Papageorgiou P, Katsambas A, Chu A. Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris. Br J Dermatol. 2000; 142:973–978.
Article4. Ammad S, Edwards C, Gonzalez M, Mills CM. The effect of blue light phototherapy on mild to moderate acne. Br J Dermatol. 2002; 147:Suppl 62. 95.5. Kawada A, Aragane Y, Kameyama H, Sangen Y, Tezuka T. Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: an open study and in vitro investigation. J Dermatol Sci. 2002; 30:129–135.
Article6. Sigurdsson V, Knulst AC, van Weelden H. Phototherapy of acne vulgaris with visible light. Dermatology. 1997; 194:256–260.
Article7. Hamilton FL, Car J, Lyons C, Car M, Layton A, Majeed A. Laser and other light therapies for the treatment of acne vulgaris: systematic review. Br J Dermatol. 2009; 160:1273–1285.
Article8. Jeong E, Hong JW, Min JA, Lee DW, Sohn MY, Lee WJ, et al. Topical ALA-Photodynamic therapy for acne can induce apoptosis of sebocytes and down-regulate their TLR-2 and TLR-4 expression. Ann Dermatol. 2011; 23:23–32.
Article9. Magin P, Pond D, Smith W, Watson A. A systematic review of the evidence for 'myths and misconceptions' in acne management: diet, face-washing and sunlight. Fam Pract. 2005; 22:62–70.
Article10. Winston MH, Shalita AR. Acne vulgaris. Pathogenesis and treatment. Pediatr Clin North Am. 1991; 38:889–903.
Article11. Fujie T, Shikiji T, Uchida N, Urano Y, Nagae H, Arase S. Culture of cells derived from the human sebaceous gland under serum-free conditions without a biological feeder layer or specific matrices. Arch Dermatol Res. 1996; 288:703–708.
Article12. Zouboulis CC. Acne and sebaceous gland function. Clin Dermatol. 2004; 22:360–366.
Article13. Suh DH, Kwon TE, Youn JI. Changes of comedonal cytokines and sebum secretion after UV irradiation in acne patients. Eur J Dermatol. 2002; 12:139–144.14. Lesnik RH, Kligman LH, Kligman AM. Agents that cause enlargement of sebaceous glands in hairless mice. II. Ultraviolet radiation. Arch Dermatol Res. 1992; 284:106–108.
Article15. Akitomo Y, Akamatsu H, Okano Y, Masaki H, Horio T. Effects of UV irradiation on the sebaceous gland and sebum secretion in hamsters. J Dermatol Sci. 2003; 31:151–159.
Article16. Lee WJ, Park KH, Sohn MY, Lee WC, Lee SJ, Kim DW. Ultraviolet B irradiation increases the expression of inflammatory cytokines in cultured sebocytes. J Dermatol. 2013; 40:993–997.
Article17. Skiba B, Neill B, Piva TJ. Gene expression profiles of TNF-alpha, TACE, furin, IL-1beta and matrilysin in UVA- and UVB-irradiated HaCat cells. Photodermatol Photoimmunol Photomed. 2005; 21:173–182.
Article18. Scordi IA, Vincek V. Timecourse study of UVB-induced cytokine induction in whole mouse skin. Photodermatol Photoimmunol Photomed. 2000; 16:67–73.
Article19. Murphy GM, Dowd PM, Hudspith BN, Brostoff J, Greaves MW. Local increase in interleukin-1-like activity following UVB irradiation of human skin in vivo. Photodermatol. 1989; 6:268–274.20. Zouboulis CC, Adjaye J, Akamatsu H, Moe-Behrens G, Niemann C. Human skin stem cells and the ageing process. Exp Gerontol. 2008; 43:986–997.
Article21. Shnitkind E, Yaping E, Geen S, Shalita AR, Lee WL. Anti-inflammatory properties of narrow-band blue light. J Drugs Dermatol. 2006; 5:605–610.22. Charakida A, Seaton ED, Charakida M, Mouser P, Avgerinos A, Chu AC. Phototherapy in the treatment of acne vulgaris: what is its role? Am J Clin Dermatol. 2004; 5:211–216.23. Elman M, Lebzelter J. Light therapy in the treatment of acne vulgaris. Dermatol Surg. 2004; 30:139–146.
Article24. Ross EV. Optical treatments for acne. Dermatol Ther. 2005; 18:253–266.
Article25. Young S, Bolton P, Dyson M, Harvey W, Diamantopoulos C. Macrophage responsiveness to light therapy. Lasers Surg Med. 1989; 9:497–505.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Insulin-Like Growth Factor-1 Increases the Expression of Inflammatory Biomarkers and Sebum Production in Cultured Sebocytes
- Study of the Photoinactivation Effect on Propionibacterium acnes after Light Irradiation with Variable Wavelengths
- Dieckol Inhibits the Effects of Particulate Matter 10 on Sebocytes, Outer Root Sheath Cells, and Cutibacterium Acnes−Pretreated Mice
- Effects of <10-μm Particulate Matter on Cultured Human Sebocytes and Outer Root Sheath Cells and Usefulness of Siegesbeckia Herba Extract
- Comparative Spectrophotometer Analysis of Ultraviolet-light Filtering, Blue-light Filtering, and Violet-light Filtering Intraocular Lenses