Allergy Asthma Respir Dis.
2014 Jul;2(3):222-226. 10.4168/aard.2014.2.3.222.
Eosinophilic cholecystitis: A rare manifestation of hypereosinophilic syndrome
- Affiliations
-
- 1Department of Internal Medicine, Hallym University College of Medicine, Chuncheon, Korea. mdqueen@hallym.or.kr
- 2Lung Research Institute, Hallym University College of Medicine, Chuncheon, Korea.
- KMID: 2262524
- DOI: http://doi.org/10.4168/aard.2014.2.3.222
Abstract
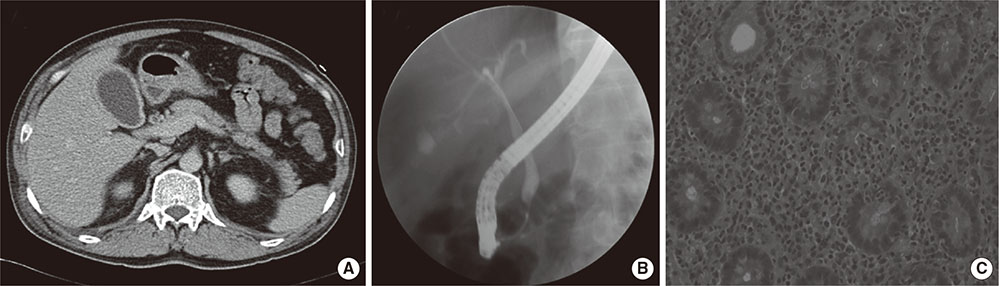
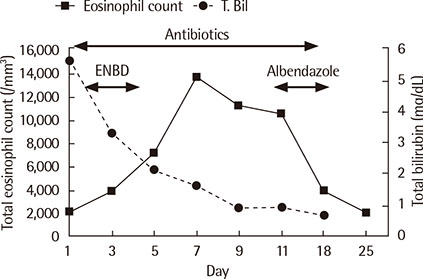
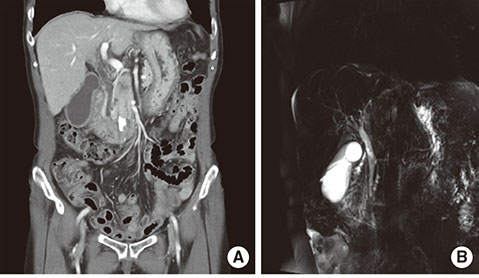
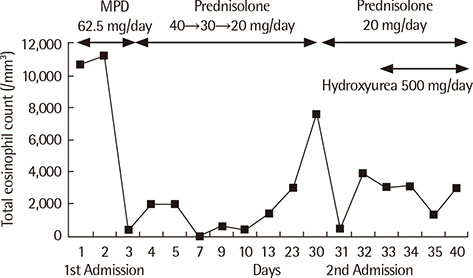
- Eosinophilic cholecystitis (EC) is a rare form of acute cholecystitis, of which diagnosis is based on classical symptoms of cholecystitis with a presence of >90% eosinophilic infiltration within the gall bladder. EC rarely manifests in idiopathic hypereosinophilic syndrome (IHES). Here, we report two cases of EC with IHES. One is a 57-year-old male who presented with acute right upper quadrant (RUQ) pain, jaundice and fever. The initial peripheral blood eosinophil count was 2,070/mm3, and further elevated to 12,590/mm3. Acute acalculous cholecystitis with cholangitis was confirmed by computed tomography (CT). He improved with endocopic nasobiliary drainage and antibiotic therapy. The other is a 64-year-old female who presented with acute RUQ pain. She also complained of dyspnea and tingling sensation of both hands and feet. The initial peripheral blood eosinophil count was 10,400/mm3. Abdominal CT revealed findings suggestive of acute acalculous cholecystitis. She improved with systemic glucocorticosteroid therapy. No other causes of hypereosinophilia were found in either patients. Thus, cholecystectomy may not be mandatory for the treatment of EC with IHES.
MeSH Terms
Figure
Reference
-
1. Fox H, Mainwaring AR. Eosinophilic infiltration of the gallbladder. Gastroenterology. 1972; 63:1049–1052.
Article2. Kerstein MD, Sheahan DG, Gudjonsson B, Lewis J. Eosinophilic cholecystitis. Am J Gastroenterol. 1976; 66:349–352.3. Dabbs DJ. Eosinophilic and lymphoeosinophilic cholecystitis. Am J Surg Pathol. 1993; 17:497–501.
Article4. Felman RH, Sutherland DB, Conklin JL, Mitros FA. Eosinophilic cholecystitis, appendiceal inflammation, pericarditis, and cephalosporin-associated eosinophilia. Dig Dis Sci. 1994; 39:418–422.
Article5. Kim YM, Lee DY, Lee JS. A case of eosinophilic cholecystitis associated with eosinophilic cholangitis and pancreatitis. Korean J Gastroenterol. 2000; 35:664–670.6. Shakov R, Simoni G, Villacin A, Baddoura W. Eosinophilic cholecystitis, with a review of the literature. Ann Clin Lab Sci. 2007; 37:182–185.7. Chusid MJ, Dale DC, West BC, Wolff SM. The hypereosinophilic syndrome: analysis of fourteen cases with review of the literature. Medicine (Baltimore). 1975; 54:1–27.8. Weller PF, Bubley GJ. The idiopathic hypereosinophilic syndrome. Blood. 1994; 83:2759–2779.
Article9. Tefferi A, Patnaik MM, Pardanani A. Eosinophilia: secondary, clonal and idiopathic. Br J Haematol. 2006; 133:468–492.
Article10. Choi DC. Eosinophilia. Korean J Asthma Allergy Clin Immunol. 2011; 31:237–245.11. Yeom SS, Kim HH, Kim JC, Hur YH, Koh YS, Cho CK, et al. Peripheral eosinophilia - is it a predictable factor associated with eosinophilic cholecystitis? Korean J Hepatobiliary Pancreat Surg. 2012; 16:65–69.
Article12. Rosengart TK, Rotterdam H, Ranson JH. Eosinophilic cholangitis: a self-limited cause of extrahepatic biliary obstruction. Am J Gastroenterol. 1990; 85:582–585.13. Simon HU, Rothenberg ME, Bochner BS, Weller PF, Wardlaw AJ, Wechsler ME, et al. Refining the definition of hypereosinophilic syndrome. J Allergy Clin Immunol. 2010; 126:45–49.
Article14. Simon HU, Klion A. Therapeutic approaches to patients with hypereosinophilic syndromes. Semin Hematol. 2012; 49:160–170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Eosinophilic Cholecystitis associated with Eosinophilic Cholangitis and Pancreatitis
- A Case of Eosinophilic Meningitis Associated with Idiopathic Hypereosinophilic Syndrome
- Hypereosinophilic Syndrome Presenting as Eosinophilic Cholangiopathy and Cystitis
- Eosinophilic Endomyocarditis Combined With Pericardial and Pleural Effusion
- Eosinophilic Annular Erythema in a Patient with Eosinophilic Granulomatosis with Polyangiitis (Churg-Strauss Syndrome)