Allergy Asthma Immunol Res.
2010 Oct;2(4):254-259. 10.4168/aair.2010.2.4.254.
Effects of Smoking Cessation on Airflow Obstruction and Quality of Life in Asthmatic Smokers
- Affiliations
-
- 1Asthma and Allergy Research Group, Korea. mdcspark@unitel.co.kr
- 2Division of Allergy and Respiratory Diseases, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 3Division of Allergy and Respiratory Diseases, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 4Division of Allergy and Respiratory Diseases, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 5Division of Allergy and Respiratory Diseases, Soonchunhyang University Gumi Hospital, Gumi, Korea.
- KMID: 2260386
- DOI: http://doi.org/10.4168/aair.2010.2.4.254
Abstract
- PURPOSE
Smoking elicits airway inflammation and airflow obstruction in patients with asthma, even after smoking cessation. The aim of this study was to examine the effects of smoking cessation on lung function and quality of life (QOL) in asthmatic patients.
METHODS
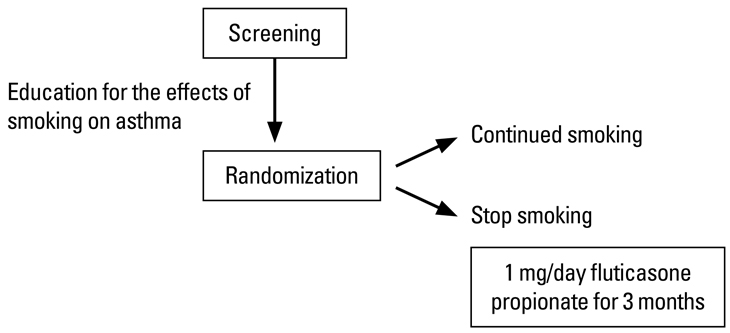
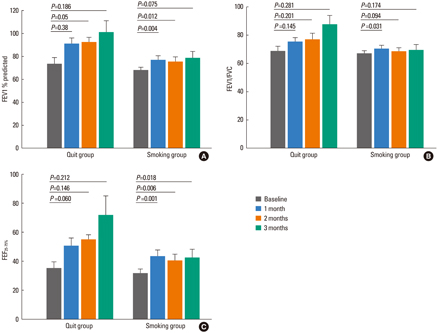
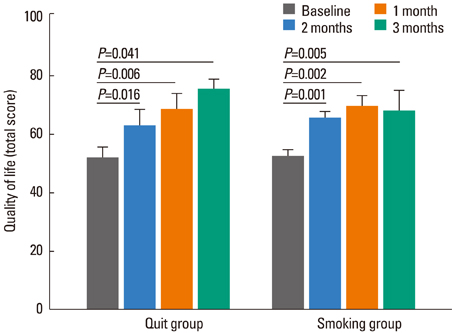
Thirty-two patients with asthma who were active smokers were recruited. After education on the effects of smoking on asthma, 22 patients continued to smoke, and 10 quit smoking. All patients were treated with inhaled fluticasone propionate (1 mg/day) for 3 months. We compared forced expiratory volume in 1 s (FEV1), FEV1/forced vital capacity (FVC), forced expiratory flow between 25 and 75% FVC (FEF(25-75%)), and scores on a QOL questionnaire at baseline, 1, 2, and 3 months.
RESULTS
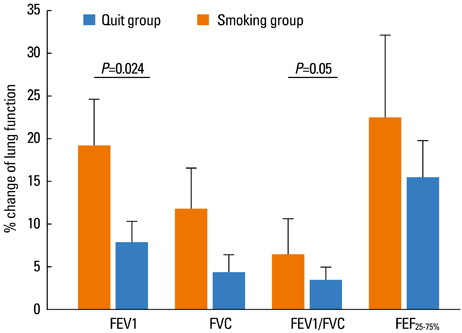
Quitters showed a greater percent change in FEV1 (19.1+/-6.3 vs. 7.9+/-2.4%, P=0.024) and FEV1/FVC (6.5+/-4.14 vs. 3.5+/-1.5%, P=0.05) than smokers. Both quitters and smokers showed improved QOL scores after 1, 2, and 3 months of fluticasone treatment.
CONCLUSIONS
Patients with asthma who quit smoking showed less airway obstruction, suggesting that smoking cessation is crucial in the management of asthma.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effects of Smoking Status on Chronic Obstructive Pulmonary Disease Prevalence in Males 40 years and Older: Findings from the Korean National Health and Nutrition Examination Survey
In Sook Jung, In-Kyung Jung
Korean J Health Promot. 2014;14(4):155-161. doi: 10.15384/kjhp.2014.14.4.155.
Reference
-
1. Thomson NC, Spears M. The influence of smoking on the treatment response in patients with asthma. Curr Opin Allergy Clin Immunol. 2005. 5:57–63.2. Chalmers GW, Macleod KJ, Little SA, Thomson LJ, McSharry CP, Thomson NC. Influence of cigarette smoking on inhaled corticosteroid treatment in mild asthma. Thorax. 2002. 57:226–230.3. Chaudhuri R, Livingston E, McMahon AD, Thomson L, Borland W, Thomson NC. Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthma. Am J Respir Crit Care Med. 2003. 168:1308–1311.4. Jang AS, Park JS, Lee JH, Park SW, Kim DJ, Uh ST, Kim YH, Park CS. The impact of smoking on clinical and therapeutic effects in asthmatics. J Korean Med Sci. 2009. 24:209–214.5. Silverman RA, Boudreaux ED, Woodruff PG, Clark S, Camargo CA Jr. Cigarette smoking among asthmatic adults presenting to 64 emergency departments. Chest. 2003. 123:1472–1479.6. Althuis MD, Sexton M, Prybylski D. Cigarette smoking and asthma symptom severity among adult asthmatics. J Asthma. 1999. 36:257–264.7. Siroux V, Pin I, Oryszczyn MP, Le Moual N, Kauffmann F. Relationships of active smoking to asthma and asthma severity in the EGEA study. Epidemiological study on the Genetics and Environment of Asthma. Eur Respir J. 2000. 15:470–477.8. Living in Britain: results from the 2002 General Household Survey [Internet]. UK Gov., Office for National Statistics. Available from: http://www.statistics.gov.uk/lib.9. Apostol GG, Jacobs DR Jr, Tsai AW, Crow RS, Williams OD, Townsend MC, Beckett WS. Early life factors contribute to the decrease in lung function between ages 18 and 40: the Coronary Artery Risk Development in Young Adults study. Am J Respir Crit Care Med. 2002. 166:166–172.10. Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med. 1998. 339:1194–1200.11. Marquette CH, Saulnier F, Leroy O, Wallaert B, Chopin C, Demarcq JM, Durocher A, Tonnel AB. Long-term prognosis of near-fatal asthma. A 6-year follow-up study of 145 asthmatic patients who underwent mechanical ventilation for a near-fatal attack of asthma. Am Rev Respir Dis. 1992. 146:76–81.12. Gallefoss F, Bakke PS. Does smoking affect the outcome of patient education and self-management in asthmatics? Patient Educ Couns. 2003. 49:91–97.13. Sippel JM, Pedula KL, Vollmer WM, Buist AS, Osborne ML. Associations of smoking with hospital-based care and quality of life in patients with obstructive airway disease. Chest. 1999. 115:691–696.14. Chalmers GW, MacLeod KJ, Thomson L, Little SA, McSharry C, Thomson NC. Smoking and airway inflammation in patients with mild asthma. Chest. 2001. 120:1917–1922.15. McKay A, Komai-Koma M, MacLeod KJ, Campbell CC, Kitson SM, Chaudhuri R, Thomson L, McSharry C, Liew FY, Thomson NC. Interleukin-18 levels in induced sputum are reduced in asthmatic and normal smokers. Clin Exp Allergy. 2004. 34:904–910.16. Van Hove CL, Moerloose K, Maes T, Joos GF, Tournoy KG. Cigarette smoke enhances Th-2 driven airway inflammation and delays inhalational tolerance. Respir Res. 2008. 9:42.17. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, November 1986. Am Rev Respir Dis. 1987. 136:225–244.18. National Asthma Education and Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma Update on Selected Topics--2002. J Allergy Clin Immunol. 2002. 110:S141–S219.19. American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991. 144:1202–1218.20. Junifer EF, Cockcroft DW, Hargreave FE. Histamine and methacholine inhalation tests: a laboratory tidal breathing protocol. 1994. 2nd ed. Lund: Astra Draco.21. Park CS, Kim YY, Kang SY. Collection between RAST and skin test for inhalant offending allergens. Korean J Allergy. 1983. 3:1–9.22. Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol. 1994. 47:81–87.23. Higenbottam TW, Feyeraband C, Clark TJ. Cigarette smoking in asthma. Br J Dis Chest. 1980. 74:279–284.24. Jensen EJ, Dahl R, Steffensen F. Bronchial reactivity to cigarette smoke; relation to lung function, respiratory symptoms, serum-immunoglobulin E and blood eosinophil and leukocyte counts. Respir Med. 2000. 94:119–127.25. Cassino C, Ito K, Bader I, Ciotoli C, Thurston G, Reibman J. Cigarette smoking and ozone-associated emergency department use for asthma by adults in New York City. Am J Respir Crit Care Med. 1999. 159:1773–1779.26. Prescott E, Lange P, Vestbo J. Effect of gender on hospital admissions for asthma and prevalence of self-reported asthma: a prospective study based on a sample of the general population. Thorax. 1997. 52:287–289.27. Rasmussen F, Taylor DR, Flannery EM, Cowan JO, Greene JM, Herbison GP, Sears MR. Risk factors for hospital admission for asthma from childhood to young adulthood: a longitudinal population study. J Allergy Clin Immunol. 2002. 110:220–227.28. Turner MO, Noertjojo K, Vedal S, Bai T, Crump S, Fitzgerald JM. Risk factors for near-fatal asthma. A case-control study in hospitalized patients with asthma. Am J Respir Crit Care Med. 1998. 157:1804–1809.29. Chaudhuri R, Livingston E, McMahon AD, Lafferty J, Fraser I, Spears M, McSharry CP, Thomson NC. Effects of smoking cessation on lung function and airway inflammation in smokers with asthma. Am J Respir Crit Care Med. 2006. 174:127–133.30. Polosa R, Knoke JD, Russo C, Piccillo G, Caponnetto P, Sarva M, Proietti L, Al-Delaimy WK. Cigarette smoking is associated with a greater risk of incident asthma in allergic rhinitis. J Allergy Clin Immunol. 2008. 121:1428–1434.31. Oosterhoff Y, Jansen MA, Postma DS, Koeter GH. Airway responsiveness to adenosine 5'-monophosphate in smokers and nonsmokers with atopic asthma. J Allergy Clin Immunol. 1993. 92:773–776.32. Saetta M, Turato G, Maestrelli P, Mapp CE, Fabbri LM. Cellular and structural bases of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001. 163:1304–1309.33. Roth MD, Arora A, Barsky SH, Kleerup EC, Simmons M, Tashkin DP. Airway inflammation in young marijuana and tobacco smokers. Am J Respir Crit Care Med. 1998. 157:928–937.34. Blaiss MS. Outcomes analysis in asthma. JAMA. 1997. 278:1874–1880.35. Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993. 118:622–629.36. Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax. 1992. 47:76–83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on Health-related Quality of Life, Smoking Knowledge, Smoking Attitude, and Smoking Cessation Intention in Male Smokers
- Effects of Family Support and Quality of Life in Relation to Smoking Cessation in Male Patient with Coronary Artery Disease
- Testing of the Theory of Planned Behavior in the Prediction of Smoking Cessation Intention and Smoking Cessation Behavior among Adolescent Smokers
- Effects of a Smoking Cessation Program on Amount of Smoking and Nicotine Dependence and Self-efficacy of Smoking Cessation for Smoking Workers
- Pharmacotherapy for Smoking Cessation in Patients with Schizophrenia