J Gynecol Oncol.
2009 Jun;20(2):107-112. 10.3802/jgo.2009.20.2.107.
Surgical practice patterns in endometrial cancer: results of the Korean Gynecologic Oncology Group survey
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul Metropolitan Boramae Hospital, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Seoul National University Hospital, Seoul, Korea. kjwksh@snu.ac.kr
- 3Department of Obstetrics and Gynecology, Severance Hospital, Seoul, Korea.
- 4Department of Obstetrics and Gynecology, Kangnam Cha Medical Center, Seoul, Korea.
- 5Department of Obstetrics and Gynecology, Inha University Hospital, Incheon, Korea.
- 6Department of Obstetrics and Gynecology, Yongdong Severance Hospital, Seoul, Korea.
- 7Department of Obstetrics and Gynecology, Asan Medical Center, Seoul, Korea.
- 8Department of Obstetrics and Gynecology, Cheil General Hospital, Seoul, Korea.
- 9Department of Obstetrics and Gynecology, Korea University Ansan Hospital, Ansan, Korea.
- 10Department of Obstetrics and Gynecology, Ajou University Hospital, Suwon, Korea.
- KMID: 2245093
- DOI: http://doi.org/10.3802/jgo.2009.20.2.107
Abstract
OBJECTIVE
This study was undertaken to document current practice patterns for the surgical treatment of endometrial cancer in Korea.
METHODS
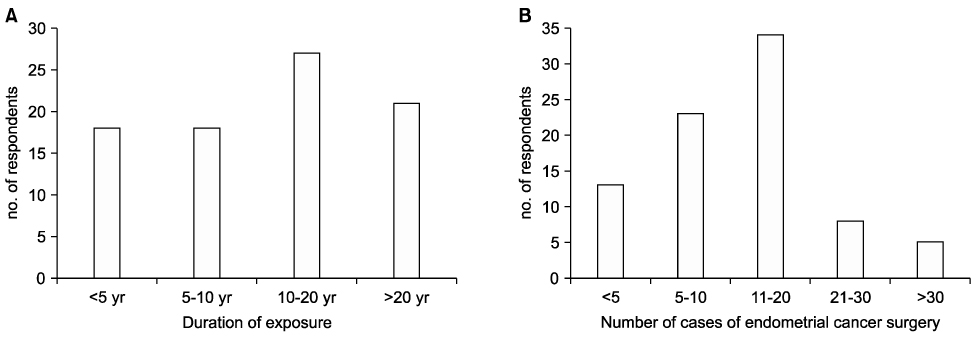
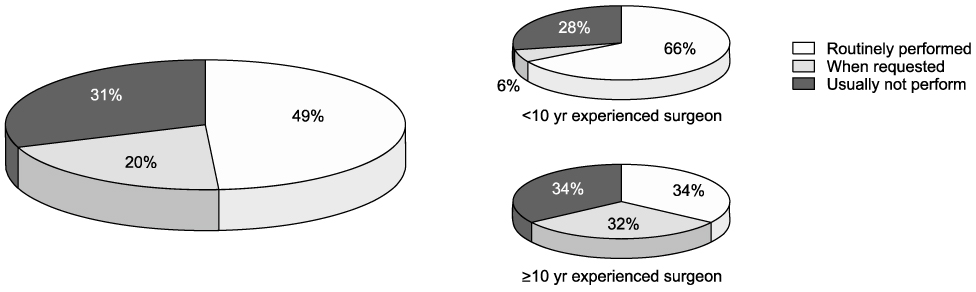
Questionnaires were distributed to 131 Korean gynecologic oncologists, all members of the Korean Gynecologic Oncology Group. Questions addressed extent of hysterectomy procedure, pelvic (PEN) or paraaortic (PAN) lymph node dissection, ovarian preservation, and omentectomy.
RESULTS
Completed questionnaires were returned by 64.1% (84/131) of the oncologists at 50 institutes. Extrafascial hysterectomy (EH) was used by 32% of respondents and modified radical hysterectomy (MRH) or radical hysterectomy (RH) by 17%. Hysterectomy procedures were selectively employed based on tumor-related factors by 51% of the respondents. Laparoscopic hysterectomy was routinely utilized by 49% and was more commonly used by younger surgeons with 10 years of experience or less. PEN dissection was routinely utilized by 67% and was used selectively based on tumor-related factors by 33%. PAN dissection/biopsy was used either routinely (43%) or selectively based on tumor-related factors (43%). PAN dissection/biopsy had never been employed by 12% of the respondents. Sixty-nine percent of respondents stated that grossly normal looking ovaries can be preserved during surgery in young aged patients with early stage disease, and 29% stated that bilateral oophorectomy should be performed irrespective of age or stage. Omentectomy was routinely performed by 11% of respondents, and was selectively performed when extrauterine spread was present by 41%.
CONCLUSION
Surgical procedures for the treatment of endometrial cancer are still not standardized among Korean gynecologic surgeons. Clinical trials to determine the benefits of the different surgical procedures should be developed.
Keyword
MeSH Terms
Figure
Reference
-
1. NCCN Clinical Practice Guidelines in Oncology [Internet]. National Comprehensive Cancer Network. c2009. cited 2009 April 22. Fort Washington: National Comprehensive Cancer Network;Available from: http://www.nccn.org.2. Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974. 44:265–272.3. Watanabe Y, Aoki D, Kitagawa R, Takeuchi S, Sagae S, Sakuragi N, et al. Status of surgical treatment procedures for endometrial cancer in Japan: results of a Japanese Gynecologic Oncology Group survey. Gynecol Oncol. 2007. 105:325–328.4. Maggino T, Romagnolo C, Landoni F, Sartori E, Zola P, Gadducci A. An analysis of approaches to the management of endometrial cancer in North America: a CTF study. Gynecol Oncol. 1998. 68:274–279.5. Yaegashi N, Ito K, Niikura H. Lymphadenectomy for endometrial cancer: is paraaortic lymphadenectomy necessary? Int J Clin Oncol. 2007. 12:176–180.6. Mariani A, Keeney GL, Aletti G, Webb MJ, Haddock MG, Podratz KC. Endometrial carcinoma: paraaortic dissemination. Gynecol Oncol. 2004. 92:833–838.7. Ozsoy M, Dilek S, Ozsoy D. Pelvic and paraaortic lymph node metastasis in clinical stage I endometrial adenocarcinoma: an analysis of 58 consecutive cases. Eur J Gynaecol Oncol. 2003. 24:398–400.8. Yenen MC, Dilek S, Dede M, Goktolga U, Deveci MS, Aydogu T. Pelvic-paraaortic lymphadenectomy in clinical Stage I endometrial adenocarcinoma: a multicenter study. Eur J Gynaecol Oncol. 2003. 24:327–329.9. Amadori A, Bucchi L, Gori G, Falcini F, Saragoni L, Amadori D. Frequency and determinants of lymphadenectomy in endometrial carcinoma: a population-based study from northern Italy. Ann Surg Oncol. 2001. 8:723–728.10. Lee TS, Jung JY, Kim JW, Park NH, Song YS, Kang SB, et al. Feasibility of ovarian preservation in patients with early stage endometrial carcinoma. Gynecol Oncol. 2007. 104:52–57.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Response to comment on: Comparison of diagnostic accuracy between endometrial curettage and aspiration biopsy in patients treated with progestin for endometrial hyperplasia: a Korean Gynecologic Oncology Group study
- Letter to editor in response to: Comparison of diagnostic accuracy between endometrial curettage and aspiration biopsy in patients treated with progestin for endometrial hyperplasia: a Korean Gynecologic Oncology Group study
- Controversies in the management of endometrial cancer: a survey of the Korean Gynecologic Oncology Group
- Present status and future direction of clinical trials in advanced endometrial carcinoma
- Sentinel lymph node mapping in endometrial and cervical cancer: a survey of practices and attitudes in gynecologic oncologists