Korean J Hepatobiliary Pancreat Surg.
2015 May;19(2):66-70. 10.14701/kjhbps.2015.19.2.66.
Balloon dilation of jejunal afferent loop functional stenosis following left hepatectomy and hepaticojejunostomy long time after pylorus-preserving pancreaticoduodenectomy: a case report
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Department of Diagnostic Imaging, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2243051
- DOI: http://doi.org/10.14701/kjhbps.2015.19.2.66
Abstract
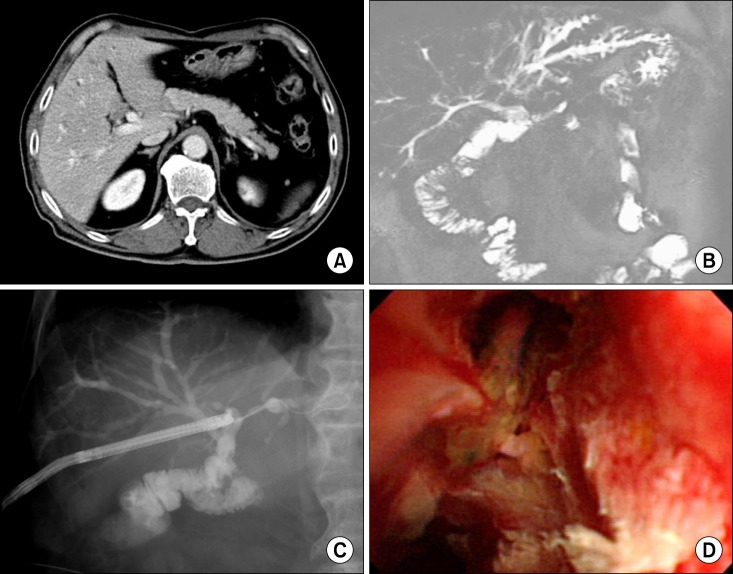
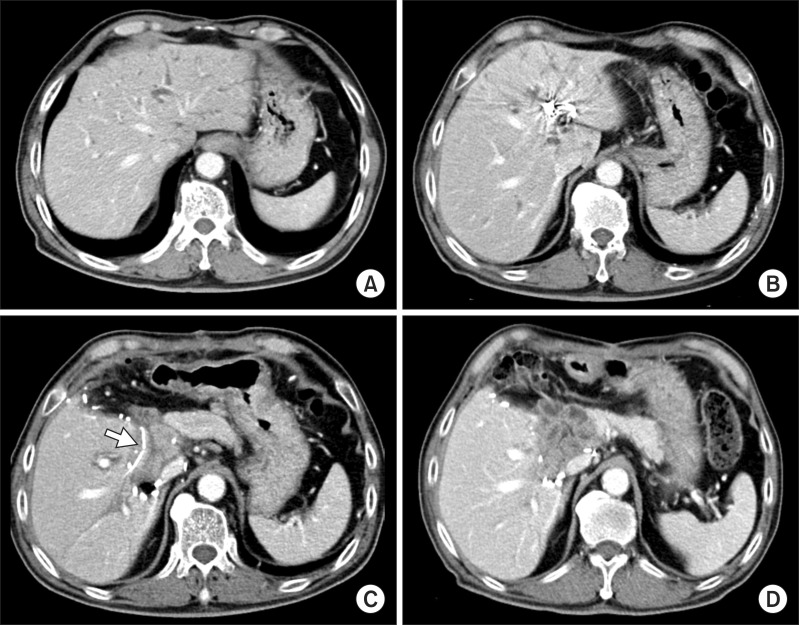
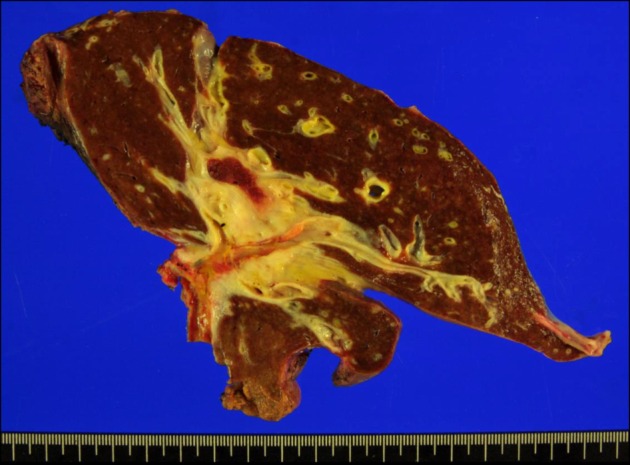
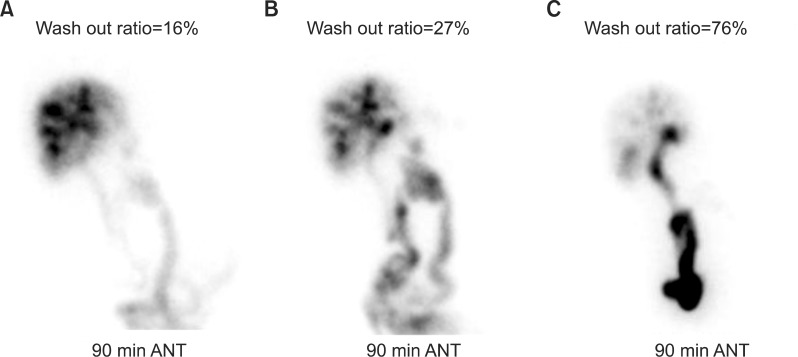
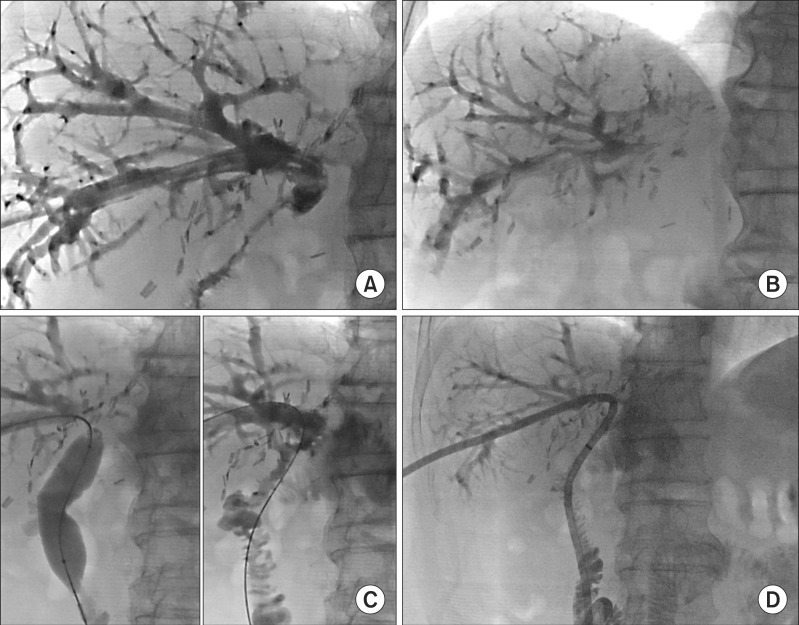
- We present a rare case of functional stenosis of the jejunal loop following left hepatectomy and hepaticojejunostomy long after pylorus-preserving pancreaticoduodenectomy (PPPD), which was successfully managed by balloon dilation. A 70-year-old Korean man had undergone PPPD 6 years before due to 1.8 cm-sized distal bile duct cancer. Sudden onset of obstructive jaundice led to diagnosis of recurrent bile duct cancer mimicking perihilar cholangiocarcinoma of type IIIb. After left portal vein embolization, the patient underwent resection of the left liver and caudate lobe and remnant extrahepatic bile duct. The pre-existing jejunal loop and choledochojejunostomy site were used again for new hepaticojejunostomy. The patient recovered uneventfully, but clamping of the percutaneous transhepatic biliary drainage (PTBD) tube resulted in cholangitis. Biliary imaging studies revealed that biliary passage into the afferent jejunal limb was significantly impaired. We performed balloon dilation of the afferent jejunal loop by using a 20 mm-wide balloon. Follow-up hepatobiliary scintigraphy showed gradual improvement in biliary excretion and the PTBD tube was removed at 1 month after balloon dilation. This very unusual condition was regarded as disuse atrophy of the jejunal loop, which was successfully managed by balloon dilation and intraluminal keeping of a large-bore PTBD tube for 1 month.
MeSH Terms
-
Aged
Bile Duct Neoplasms
Bile Ducts, Extrahepatic
Cholangiocarcinoma
Cholangitis
Choledochostomy
Constriction
Constriction, Pathologic*
Diagnosis
Drainage
Extremities
Follow-Up Studies
Hepatectomy*
Humans
Jaundice, Obstructive
Liver
Muscular Disorders, Atrophic
Pancreaticoduodenectomy*
Portal Vein
Radionuclide Imaging
Figure
Cited by 1 articles
-
Percutaneous trans-hepatic rescue and neo-creation of a post-surgical complete hepaticojejunostomy dehiscence
Umberto Geremia Rossi, Andrea DeCensi, Gian Andrea Rollandi, Marco Filauro
Ann Hepatobiliary Pancreat Surg. 2021;25(3):386-389. doi: 10.14701/ahbps.2021.25.3.386.
Reference
-
1. Hwang S, Lee SG, Lee YJ, Ahn CS, Kim KH, Moon DB, et al. Treatment of recurrent bile duct stricture after primary reconstruction for laparoscopic cholecystectomy-induced injury. Surg Laparosc Endosc Percutan Tech. 2008; 18:445–448. PMID: 18936662.
Article2. Hwang S, Yu YD, Park GC, Choi YI, Park PJ, Jung SW, et al. Pancreatoduodenectomy for local intrapancreatic recurrence after bile duct resection of mid bile duct carcinoma. Hepatogastroenterology. 2010; 57:1040–1045. PMID: 21410028.3. Zach S, Wilhelm TJ, Rückert F, Herrle F, Niedergethmann M. Redo surgery after duodenum-preserving pancreatic head resection for chronic pancreatitis: high incidence in long-term follow-up. J Gastrointest Surg. 2015; 19:1078–1085. PMID: 25903850.
Article4. Mason GR. Perspectives a century later on the "Ansa en Y" of César Roux. Am J Surg. 1991; 161:262–265. PMID: 1990880.
Article5. Shoshany G, Diamond E, Mordechovitz D, Bar-Maor JA. Jejunal mucosal function of the isolated bowel segment created by omentoenteropexy in dogs: a study by in situ luminal perfusion. J Pediatr Surg. 1995; 30:402–405. PMID: 7760229.
Article6. Remillard RL, Guerino F, Dudgeon DL, Yardley JH. Intravenous glutamine or limited enteral feedings in piglets: amelioration of small intestinal disuse atrophy. J Nutr. 1998; 128(12 Suppl):2723S–2726S. PMID: 9868251.
Article7. Hwang S, Ha TY, Ko GY, Kwon DI, Song GW, Jung DH. Reappraisal of preoperative sequential portal and hepatic vein embolization in patients with hepatobiliary malignancy: single institution experience with 42 patients. World J Surg. 2015; [in press].
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Management of Afferent Loop Syndrome after a Pylorus Preserving Pancreatoduodenecotomy Presenting with Obstructive Jaundice and Ascending Cholangitis
- Jejunal varix bleeding with extrahepatic portal vein obstruction after pylorus-preserving pancreatoduodenectomy: report of two cases
- Percutaneous Cholangioscopic Lithotripsy for Afferent Loop Syndrome Caused by Enterolith Development after Roux-en-Y Hepaticojejunostomy: A Case Report
- Gallstone ileus inducing obstructive jaundice at the afferent loop of Roux-en-Y hepaticojejunostomy after bile duct cancer surgery: a case report
- Risk factors for recurrent stenosis after balloon dilation for benign hepaticojejunostomy anastomotic stricture