Conjoined unification venoplasty for triple portal vein branches of right liver graft: a case report and technical refinement
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2243016
- DOI: http://doi.org/10.14701/kjhbps.2016.20.2.61
Abstract
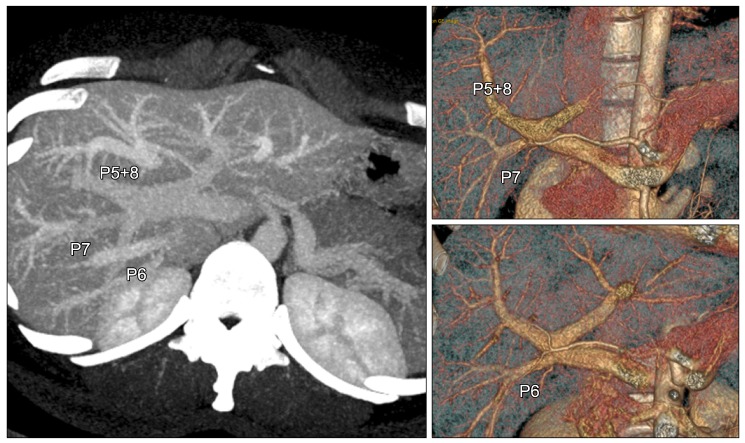
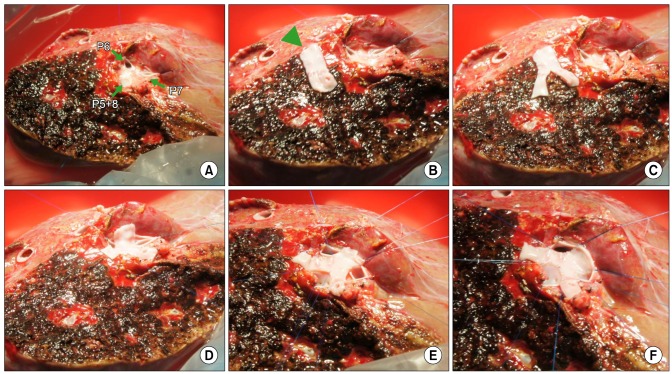
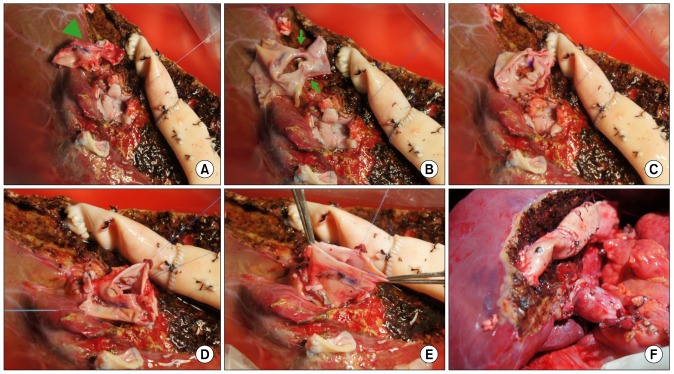
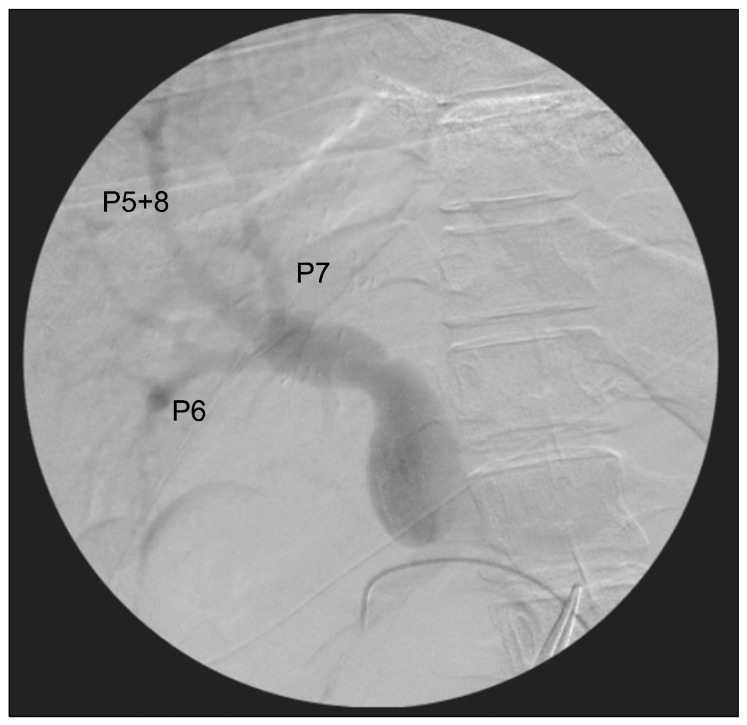
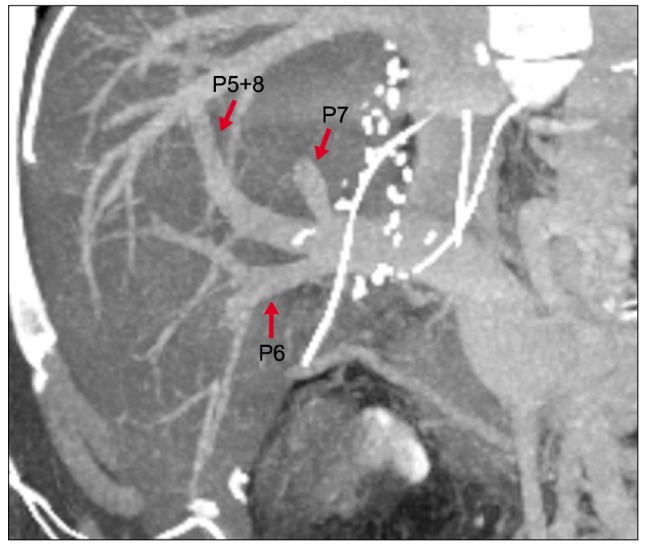
- Anomalous portal vein (PV) branching of the donor liver is uncommon and usually makes two, or rarely, more separate PV branches at the right liver graft. Autologous PV Y-graft interposition has long been regarded as the standard procedure, but is currently replaced with the newly developed technique of conjoined unification venoplasty (CUV) due to its superior results. Herein, we presented a case of CUV application to three PV openings of a right liver graft. The recipient was a 32-year-old male patient with hepatitis B virus-associated liver cirrhosis. The living liver donor was his 33-year-old sister who had a type III PV anomaly, but the right posterior PV branch was bifurcated early into separate branches of the segments VI and VII, thus three right liver PV branches were cut separately. We used the CUV technique consisting of placement of a small vein unification patch between three PV orifices, followed by overlying coverage with a crotch-opened autologous portal Y-graft. The portal Y-graft was excised and its crotches were incised to make a wide common orifice. Three bidirectional running sutures were required to attach the crotch-opened autologous portal Y-graft. After portal reperfusion, the conjoined PV portion bulged like a tennis ball, providing a wide range of alignment tolerance. The patient recovered uneventfully from the liver transplantation operation. The CUV technique enabled uneventful reconstruction of triple donor PV orifices. Thus, CUV can be a useful and effective technical option for reconstruction of right liver grafts with various anomalous PVs.
MeSH Terms
Figure
Cited by 3 articles
-
Long-term results of conjoined unification venoplasty for multiple portal vein branches of the right liver graft in living donor liver transplantations
Sung Yeon Yoo, Shin Hwang, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Chul-Soo Ahn, Deok-Bog Moon, Ki-Hun Kim, Young-In Yoon, Yo-Han Park, Hui-Dong Cho, Yong-Kyu Chung, Sang-Hyun Kang, Jin-Uk Choi, Sung-Gyu Lee
Korean J Transplant. 2019;33(4):106-111. doi: 10.4285/jkstn.2019.33.4.106.Wedged-patch venoplasty of the left liver graft portal vein for size matching in pediatric living donor liver transplantation
Sang-Hyun Kang, Jung-Man Namgoong, Shin Hwang, Dong-Hwan Jung, Kyung-Mo Kim
Ann Hepatobiliary Pancreat Surg. 2019;23(2):183-186. doi: 10.14701/ahbps.2019.23.2.183.Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion
Shin Hwang, Tae-Yong Ha, Chul-Soo Ahn, Deok-Bog Moon, Ki-Hun Kim, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Sung-Gyu Lee
Korean J Hepatobiliary Pancreat Surg. 2016;20(3):97-101. doi: 10.14701/kjhbps.2016.20.3.97.
Reference
-
1. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 2006; 12:920–927. PMID: 16721780.
Article2. Marcos A, Orloff M, Mieles L, Olzinski A, Sitzmann J. Reconstruction of double hepatic arterial and portal venous branches for right-lobe living donor liver transplantation. Liver Transpl. 2001; 7:673–679. PMID: 11510010.
Article3. Thayer WP, Claridge JA, Pelletier SJ, Oh CK, Sanfey HA, Sawyer RG, et al. Portal vein reconstruction in right lobe living-donor liver transplantation. J Am Coll Surg. 2002; 194:96–98. PMID: 11800348.4. Lee SG, Hwang S, Kim KH, Ahn CS, Park KM, Lee YJ, et al. Approach to anatomic variations of the graft portal vein in right lobe living-donor liver transplantation. Transplantation. 2003; 75(3 Suppl):S28–S32. PMID: 12589136.
Article5. Hwang S, Lee SG, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Technique and outcome of autologous portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Liver Transpl. 2009; 15:427–434. PMID: 19326410.
Article6. Lee HJ, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Long-term outcomes of portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Transplant Proc. 2012; 44:454–456. PMID: 22410042.
Article7. Ha TY, Hwang S, Moon DB, Ahn CS, Kim KH, Song GW, et al. Conjoined unification venoplasty for graft double portal vein branches as a modification of autologous Y-graft interposition. Liver Transpl. 2015; 21:707–710. PMID: 25762169.
Article8. Hwang S, Ha TY, Song GW, Jung DH, Moon DB, Ahn CS, et al. Conjoined unification venoplasty for double portal vein branches of right liver graft: 1-year experience at a high-volume living donor liver transplantation center. J Gastrointest Surg. 2016; 20:199–205. PMID: 26497191.
Article9. Song GW, Lee SG, Hwang S, Kim KH, Ahn CS, Moon DB, et al. ABO-incompatible adult living donor liver transplantation under the desensitization protocol with rituximab. Am J Transplant. 2016; 16:157–170. PMID: 26372830.
Article10. Hwang S, Ha TY, Ahn CS, Moon DB, Song GW, Kim KH, et al. Hemodynamics-compliant reconstruction of the right hepatic vein for adult living donor liver transplantation with a right liver graft. Liver Transpl. 2012; 18:858–866. PMID: 22422708.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft
- Side-to-side portal vein reconstruction for infant-to-infant deceased donor whole liver transplantation: Report of 2 cases with video
- Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion
- Long-term results of conjoined unification venoplasty for multiple portal vein branches of the right liver graft in living donor liver transplantations
- Portal vein reconstruction using side-to-side unification technique for infant-to-infant deceased donor whole liver transplantation