Healthc Inform Res.
2013 Dec;19(4):286-292. 10.4258/hir.2013.19.4.286.
Contribution of Clinical Archetypes, and the Challenges, towards Achieving Semantic Interoperability for EHRs
- Affiliations
-
- 1Centre for Health Informatics and Multiprofessional Education, University College London, London, UK. a.tapuria@ucl.ac.uk
- 2Department of Bioregulatory Medicine, Ehime University Graduate School of Medicine, Ehime, Japan.
- KMID: 2229504
- DOI: http://doi.org/10.4258/hir.2013.19.4.286
Abstract
OBJECTIVES
The objective is to introduce 'clinical archetype' which is a formal and agreed way of representing clinical information to ensure interoperability across and within Electronic Health Records (EHRs). The paper also aims at presenting the challenges building quality labeled clinical archetypes and the challenges towards achieving semantic interoperability between EHRs.
METHODS
Twenty years of international research, various European healthcare informatics projects and the pioneering work of the openEHR Foundation have led to the following results.
RESULTS
The requirements for EHR information architectures have been consolidated within ISO 18308 and adopted within the ISO 13606 EHR interoperability standard. However, a generic EHR architecture cannot ensure that the clinical meaning of information from heterogeneous sources can be reliably interpreted by receiving systems and services. Therefore, clinical models called 'clinical archetypes' are required to formalize the representation of clinical information within the EHR. Part 2 of ISO 13606 defines how archetypes should be formally represented. The current challenge is to grow clinical communities to build a library of clinical archetypes and to identify how evidence of best practice and multi-professional clinical consensus should best be combined to define archetypes at the optimal level of granularity and specificity and quality label them for wide adoption. Standardizing clinical terms within EHRs using clinical terminology like Systematized Nomenclature of Medicine Clinical Terms is also a challenge.
CONCLUSIONS
Clinical archetypes would play an important role in achieving semantic interoperability within EHRs. Attempts are being made in exploring the design and adoption challenges for clinical archetypes.
MeSH Terms
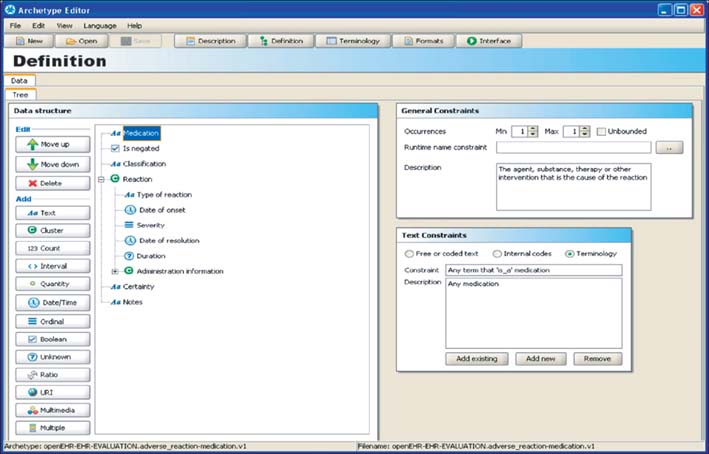
Figure
Reference
-
1. Kalra D. ISO/DIS 18308 Requirements for an Electronic Health Record reference architecture. Geneva, Switzerland: International Organization for Standardization;2010.2. Kalra D, Lloyd D. ISO 13606 Electronic Health Record communication. Part 1: Reference Model. Geneva, Switzerland: International Organization for Standardization;2008.3. Kalra D. ISO 13606 Electronic Health Record communication. Part 3: Reference archetypes and term lists. Geneva, Switzerland: International Organization for Standardization;2009.4. Kalra D. ISO/TS 13606 Electronic Health Record Communication. Part 4: Security. Geneva, Switzerland: International Organization for Standardization;2009.5. Kalra D. ISO/EN 13606 Electronic Health Record communication. Part 5: Interface specification. Geneva, Switzerland: International Organization for Standardization;2010.6. Kalra D, Beale T, Lloyd D, Heard S. ISO 13606 Electronic Health Record communication. Part 2: Archetype interchange specification. Geneva, Switzerland: International Organization for Standardization;2008.7. openEHR [Internet]. London: openEHR Foundation;2013. cited at 2013 Dec 1. Available from: http://www.openehr.org.8. SemanticHealthNet [Internet]. [unknown]: SemanticHealthNet;2013. cited at 2013 Dec 1. Available from: http://www.semantichealthnet.eu.9. Kalra D. Clinical foundations and information architecture for the implementation of a federated health record service [dissertation]. London: University College London;2002.10. Smith R. What clinical information do doctors need? BMJ. 1996; 313(7064):1062–1068.
Article11. Patterson D, Ingram D, Kalra D. Information for clinical governance. In : Lugon M, Secker-Walker J, editors. Clinical governance: making it happen. London: The Royal Society of Medicine Press;1999.12. Waegemann CP. Medical Record Institute's survey of electronic health record trends and usage. In : Proceedings of Toward an Electronic Health Record Europe '99; 1999 Nov 14-17; London, UK. p. 147–158.13. Audit Commission for Local Authorities and the National Health Service in England and Wales. A spoonful of sugar: medicines management in NHS hospitals. London: Audit Commission;2001.14. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington (DC): National Academies Press;2000.15. Hammond WE, Pollard DL, Straube MJ. Managing healthcare: a view of tomorrow. Stud Health Technol Inform. 1998; 52(Pt 1):26–30.16. Rothschild AS, Dietrich L, Ball MJ, Wurtz H, Farish-Hunt H, Cortes-Comerer N. Leveraging systems thinking to design patient-centered clinical documentation systems. Int J Med Inform. 2005; 74(5):395–398.
Article17. Martinez-Costa C, Menarguez-Tortosa M, Fernandez-Breis JT. An approach for the semantic interoperability of ISO EN 13606 and OpenEHR archetypes. J Biomed Inform. 2010; 43(5):736–746.
Article18. Rector AL, Nowlan WA, Kay S. Foundations for an electronic medical record. Methods Inf Med. 1991; 30(3):179–186.
Article19. Lopez DM, Blobel BG. A development framework for semantically interoperable health information systems. Int J Med Inform. 2009; 78(2):83–103.
Article20. Health Level Seven International. Using SNOMED CT in HL7 Version 3: Implementation Guide, Release 1.5 [Internet]. Ann Arbor (MI): Health Level Seven International;2009. cited 2013 Dec 1. Available from: http://wiki.hl7.org/index.php?title=Using_SNOMED_CT_in_HL7_Version_3;_Implementation_Guide,_Release_1.5.21. Nightingale PG, Adu D, Richards NT, Peters M. Implementation of rules based computerised bedside prescribing and administration: intervention study. BMJ. 2000; 320(7237):750–753.
Article22. Bates DW. Using information technology to reduce rates of medication errors in hospitals. BMJ. 2000; 320(7237):788–791.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Validation of Archetypes for Nursing Problems in Breast Cancer Patients
- Clinical Terminologies: A Solution for Semantic Interoperability
- Use of clinical terminology for semantic interoperability of electronic health records
- Challenges in and Opportunities for Electronic Health Record-Based Data Analysis and Interpretation
- Establishing semantic interoperability in the course of clinical document exchange using international standard for metadata registry