Korean J Crit Care Med.
2014 Nov;29(4):257-265. 10.4266/kjccm.2014.29.4.257.
Extended-Spectrum beta-Lactamase and Multidrug Resistance in Urinary Sepsis Patients Admitted to the Intensive Care Unit
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea. f2000tj@gmail.com
- 2Division of Nephrology, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 3Division of Infectious disease, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 4Department of Laboratory Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- KMID: 2227732
- DOI: http://doi.org/10.4266/kjccm.2014.29.4.257
Abstract
- BACKGROUND
The role of extended-spectrum beta-lactamase (ESBL)-producing or multidrug-resistant (MDR) organisms in patients with sepsis secondary to urinary traction infection (UTI) has not been investigated extensively in the intensive care unit (ICU) setting.
METHODS
Patients with UTI sepsis admitted to the ICU were retrospectively enrolled in this study (January 2009-December 2012). We investigated the impact of ESBL-producing and ESBL-negative MDR organisms on hospital outcome.
RESULTS
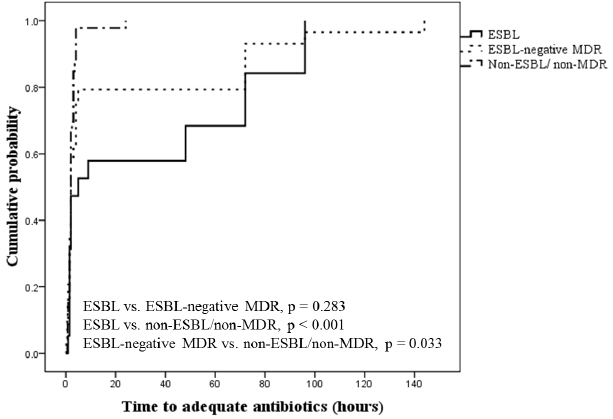
In total, 94 patients were enrolled (median age, 73.0 years; female, 81.9%), and ESBL-producing and ESBL-negative MDR organisms accounted for 20.2% (n = 19) and 30.9% (n = 29), respectively. Both patients with ESBL-producing and ESBL-negative MDR organisms were more likely to experience a delay in adequate antibiotic therapy than those with non-ESBL/non-MDR organisms (p < 0.001 and p = 0.032, respectively). However, only patients with ESBL-producing organisms showed a higher mortality rate (ESBL vs. ESBL-negative MDR vs. non-ESBL/non-MDR, 31.6% vs. 10.3%.vs. 10.9%, respectively). In multivariate analyses, ESBL production was significantly associated with hospital mortality (odds ratio, 11.547; 95micro confidence interval, 1.047-127.373), and prior admission was a significant predictor of ESBL production.
CONCLUSIONS
Although both ESBL-producing and ESBL-negative MDR organisms are associated with delayed administration of appropriate antibiotics, only ESBL production is a significant predictor of hospital mortality among patients with UTI sepsis in the ICU setting.
Keyword
MeSH Terms
Figure
Reference
-
References
1). Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348:1546–54.
Article2). Brun-Buisson C, Meshaka P, Pinton P, Vallet B; EPISEPSIS Study Group. EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004; 30:580–8.3). Rosser CJ, Bare RL, Meredith JW. Urinary tract infections in the critically ill patient with a urinary catheter. Am J Surg. 1999; 177:287–90.
Article4). Lu PL, Liu YC, Toh HS, Lee YL, Liu YM, Ho CM, et al. Epidemiology and antimicrobial susceptibility profiles of gram-negative bacteria causing urinary tract infections in the Asia-Pacific region: 2009–2010 results from the study for monitoring antimicrobial resistance trends (SMART). Int J Antimicrob Agents. 2012; 40:S37–43.
Article5). Hawser SP, Bouchillon SK, Hoban DJ, Badal RE, Hsueh PR, Paterson DL. Emergence of high levels of extended-spectrum-beta-lactamase-producing gram-negative bacilli in the Asia-Pacific region: data from the study for monitoring antimicrobial resistance trends (SMART) program, 2007. Antimicrob Agents Chemother. 2009; 53:3280–4.6). Frakking FN, Rottier WC, Dorigo-Zetsma JW, van Hattem JM, van Hees BC, Kluytmans JA, et al. Appropriateness of empirical treatment and outcome in bacteremia caused by extended-spectrum-β -lactamase-producing bacteria. Antimicrob Agents Chemother. 2013; 57:3092–9.7). Lin HC, Lai LA, Wu JY, Su YM, Chang SP, Hsueh YM. Risk factors for acquiring extended-spectrum β -lactamase-producing Enterobacteriaceae in geriatric patients with multiple comorbidities in respiratory care wards. Geriatr Gerontol Int. 2013; 13:663–71.8). Park SH, Choi SM, Lee DG, Kim J, Choi JH, Kim SH, et al. Emergence of extended-spectrum β -lactamase-producing escherichia coli as a cause of community-onset bacteremia in South Korea: risk factors and clinical outcomes. Microb Drug Resist. 2011; 17:537–44.9). Rodríguez-Baño J, Picón E, Gijón P, Hernández JR, Ruíz M, Peña C, et al. Community-onset bacteremia due to extended-spectrum beta-lactamase-producing Escherichia coli: risk factors and prognosis. Clin Infect Dis. 2010; 50:40–8.10). Ku NS, Kim YC, Kim MH, Song JE, Oh DH, Ahn JY, et al. Risk factors for 28-day mortality in elderly patients with extended-spectrum β -lactamase (ESBL)-producing Escherichia coli and Klebsiella pneumoniae bacteremia. Arch Gerontol Geriatr. 2014; 58:105–9.11). Nicolle LE. Urinary tract infection. Crit Care Clin. 2013; 29:699–715.
Article12). Hayakawa K, Gattu S, Marchaim D, Bhargava A, Palla M, Alshabani K, et al. Epidemiology and risk factors for isolation of Escherichia coli producing CTX-M-type extended-spectrum β -lactamase in a large U.S. medical center. Antimicrob Agents Chemother. 2013; 57:4010–8.13). Linhares I, Raposo T, Rodrigues A, Almeida A. Frequency and antimicrobial resistance patterns of bacteria implicated in community urinary tract infections: a ten-year surveillance study (2000–2009). BMC Infect Dis. 2013; 13:19.
Article14). Calandra T, Cohen J. International Sepsis Forum Definition of Infection in the ICU Consensus Conference: The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med. 2005; 33:1538–48.15). Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013; 39:165–228.
Article16). Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Healthcare--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002; 137:791–7.17). Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: seventeenth informational supplement M100-S17. Wayne, PA: CLSI;2007.18). The Korean Society of Infectious Diseases; The Korean Society for Chemotherapy; Korean Association of Urogenital Tract Infection and Inflammation; The Korean Society of Clinical Microbiology. Clinical guideline for the diagnosis and treatment of urinary tract infections: asymptomatic bacteriuria, uncomplicated & complicated urinary tract infections, bacterial prostatitis. Infect Chemother. 2011; 43:1–25.19). Briongos-Figuero LS, Gómez-Traveso T, Bachiller-Luque P, Domínguez-Gil González M, Gómez-Nieto A, Palacios-Martín T, et al. Epidemiology, risk factors and comorbidity for urinary tract infections caused by extended-spectrum beta-lactamase (ESBL)-producing enterobacteria. Int J Clin Pract. 2012; 66:891–6.
Article20). Sader HS, Flamm RK, Jones RN. Frequency of occurrence and antimicrobial susceptibility of gram-negative bacteremia isolates in patients with urinary tract infection: results from United States and European hospitals (2009–2011). J Chemother. 2014; 26:133–8.
Article21). Zilberberg MD, Shorr AF. Secular trends in gram-negative resistance among urinary tract infection hospitalizations in the United States, 2000–2009. Infect Control Hosp Epidemiol. 2013; 34:940–6.
Article22). Lin JN, Chen YH, Chang LL, Lai CH, Lin HL, Lin HH. Clinical characteristics and outcomes of patients with extended-spectrum β -lactamase-producing bacteremias in the emergency department. Intern Emerg Med. 2011; 6:547–55.23). Lye DC, Earnest A, Ling ML, Lee TE, Yong HC, Fisher DA, et al. The impact of multidrug resistance in healthcare-associated and nosocomial gram-negative bacteraemia on mortality and length of stay: cohort study. Clin Microbiol Infect. 2012; 18:502–8.
Article24). Hoban DJ, Nicolle LE, Hawser S, Bouchillon S, Badal R. Antimicrobial susceptibility of global inpatient urinary tract isolates of Escherichia coli: results from the study for monitoring antimicrobial resistance trends (SMART) program: 2009–2010. Diagn Microbiol Infect Dis. 2011; 70:507–11.
Article25). Jean SS, Hsueh PR, Lee WS, Chang HT, Chou MY, Chen IS, et al. Nationwide surveillance of antimicrobial resistance among Enterobacteriaceae in intensive care units in Taiwan. Eur J Clin Microbiol Infect Dis. 2009; 28:215–20.
Article26). Azap OK, Arslan H, Serefhanoğlu K, Colakoğlu S, Erdoğan H, Timurkaynak F, et al. Risk factors for extended-spectrum beta-lactamase positivity in uropathogenic Escherichia coli isolated from community-acquired urinary tract infections. Clin Microbiol Infect. 2010; 16:147–51.27). Lee DS, Lee CB, Lee SJ. Prevalence and risk factors for extended spectrum beta-lactamase-producing uropathogens in patients with urinary tract infection. Korean J Urol. 2010; 51:492–7.
Article28). Rottier WC, Ammerlaan HS, Bonten MJ. Effects of confounders and intermediates on the association of bacteraemia caused by extended-spectrum β -lactamase-producing Enterobacteriaceae and patient outcome: a meta-analysis. J Antimicrob Chemother. 2012; 67:1311–20.29). Rodríguez-Baño J, Pascual A. Clinical significance of extended-spectrum beta-lactamases. Expert Rev Anti Infect Ther. 2008; 6:671–83.30). Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, et al. Bloodstream infections due to extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae: risk factors for mortality and treatment outcome, with special emphasis on antimicrobial therapy. Antimicrob Agents Chemother. 2004; 48:4574–81.31). Kang CI, Kim SH, Bang JW, Kim HB, Park SW, Choe YJ, et al. Risk factors for infection and treatment outcome of bloodstream infections due to extended spectrum beta-lactamases producing Klebsiella pneumoniae. Infect Chemother. 2003; 35:61–70.32). Park SH, Choi SM, Chang YK, Lee DG, Cho SY, Lee HJ, et al. The efficacy of non-carbapenem antibiotics for the treatment of community-onset acute pyelonephritis due to extended-spectrum β -lactamase-producing Escherichia coli. J Antimicrob Chemother. 2014; 69:2848–56.33). Chang R, Greene MT, Chenoweth CE, Kuhn L, Shuman E, Rogers MA, et al. Epidemiology of hospital-acquired urinary tract-related bloodstream infection at a university hospital. Infect Control Hosp Epidemiol. 2011; 32:1127–9.
Article34). Menashe G, Borer A, Yagupsky P, Peled N, Gilad J, Fraser D, et al. Clinical significance and impact on mortality of extended-spectrum beta-lactamase-producing Enterobacteriaceae isolates in nosocomial bacteremia. Scand J Infect Dis. 2001; 33:188–93.35). Kim BN, Woo JH, Kim MN, Ryu J, Kim YS. Clinical implications of extended-spectrum beta-lactamase-producing Klebsiella pneumoniae bacteraemia. J Hosp Infect. 2002; 52:99–106.36). Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012; 16:R74.
Article37). Hur M, Kim H, Lee S, Cristofano F, Magrini L, Marino R, et al. Diagnostic and prognostic utilities of multimarkers approach using procalcitonin, B-type natriuretic peptide, and neutrophil gelatinase-associated lipocalin in critically ill patients with suspected sepsis. BMC Infect Dis. 2014; 14:224.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Neonatal Osteomyelitis due to Extended Spectrum beta-lactamase Producing Klebsiella pneumoniae
- A Case Report of Sepsis by Extended-Spectrum beta-Lactamase Producing Escherichia Coli
- Clinical Significance of Extended-spectrum β-lactamase-producing Bacteria in First Pediatric Febrile Urinary Tract Infections and Differences between Age Groups
- Analyses of Clinical Characteristics and Hematologic Studies of Confirmed Infants by Extended Spectrum beta-lactamase Producing Escherichia coli or Klebsiella pneumonia in Neonatal Intensive Care Unit
- Characterization of Antimicrobial Susceptibility, Extended-Spectrum β-Lactamase Genes and Phylogenetic Groups of Enteropathogenic Escherichia coli Isolated from Patients with Diarrhea