Korean Circ J.
2007 Jul;37(7):318-326. 10.4070/kcj.2007.37.7.318.
A Novel Index of Microcirculatory Resistance for Invasively Assessing Myocardial Viability after Primary Angioplasty for Treating Acute Myocardial Infarction: Comparison with FDG-PET Imaging
- Affiliations
-
- 1Department of Cardiology, School of Medicine, Ajou University, Suwon, Korea. sjtahk@ajou.ac.kr
- KMID: 2227059
- DOI: http://doi.org/10.4070/kcj.2007.37.7.318
Abstract
-
BACKGROUND AND OBJECTIVES: The state of the coronary microcirculation is an important determinant of the myocardial viability and clinical outcomes for patients suffering with acute myocardial infarction (AMI). However, there are scant comparative studies on the most reliable invasive, on-site measurement for assessing the microvascular integrity and myocardial viability in AMI patients. The aim of this study is to evaluate the usefulness of a novel index of microcirculatory resistance (IMR) and the coronary physiologic parameters for predicting the myocardial viability after primary percutaneous coronary intervention (PCI) in AMI patients.
SUBJECTS AND METHODS
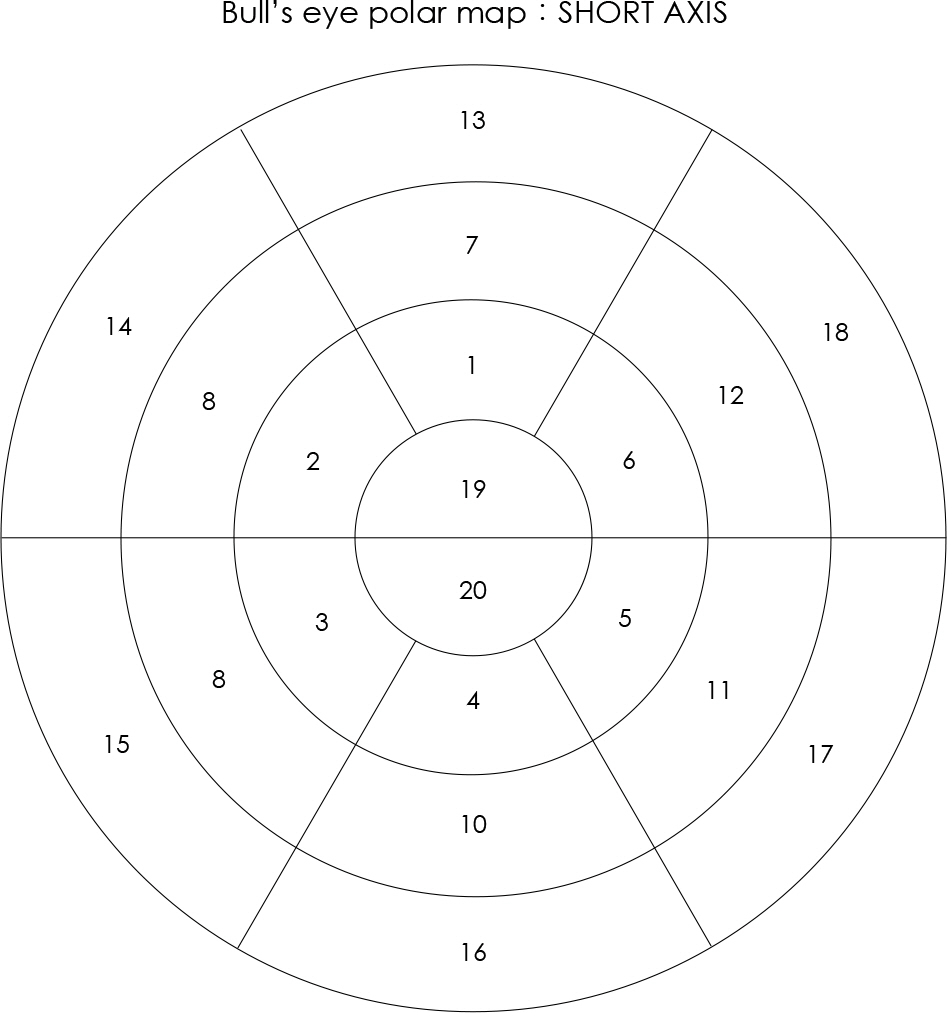
Twenty-four patients (21 males, mean age: 55+/-11 years) underwent primary PCI for AMI (LAD: 17, RCA: 6, LCX: 1) were enrolled. After successful PCI, using a pressure-temperature sensor-tipped coronary wire, the thermodilution-derived CFR (CFRthermo) and coronary wedge pressure (Pcw) were measured and the ratio of the Pcw and the mean aortic pressure (Pcw/Pa) was calculated, along with the IMR, which was defined as the distal coronary pressure divided by the inverse of the hyperemic mean transit time. 18F-fluorodeoxyglucose (FDG) PET was performed after primary PCI at 7 days post-AMI to evaluate the myocardial viability by the regional percentage of FDG uptake in the infarct-related segments.
RESULTS
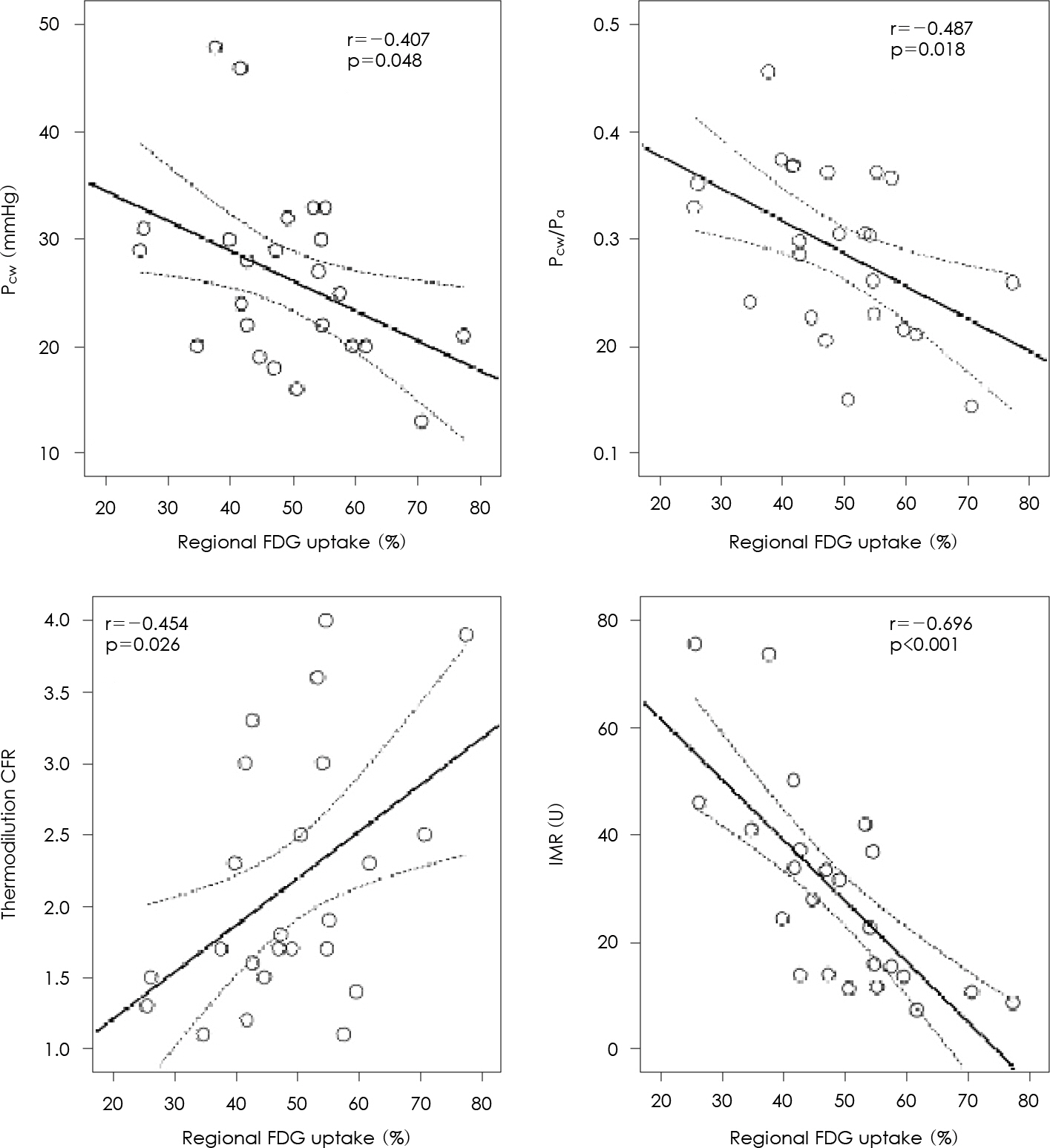
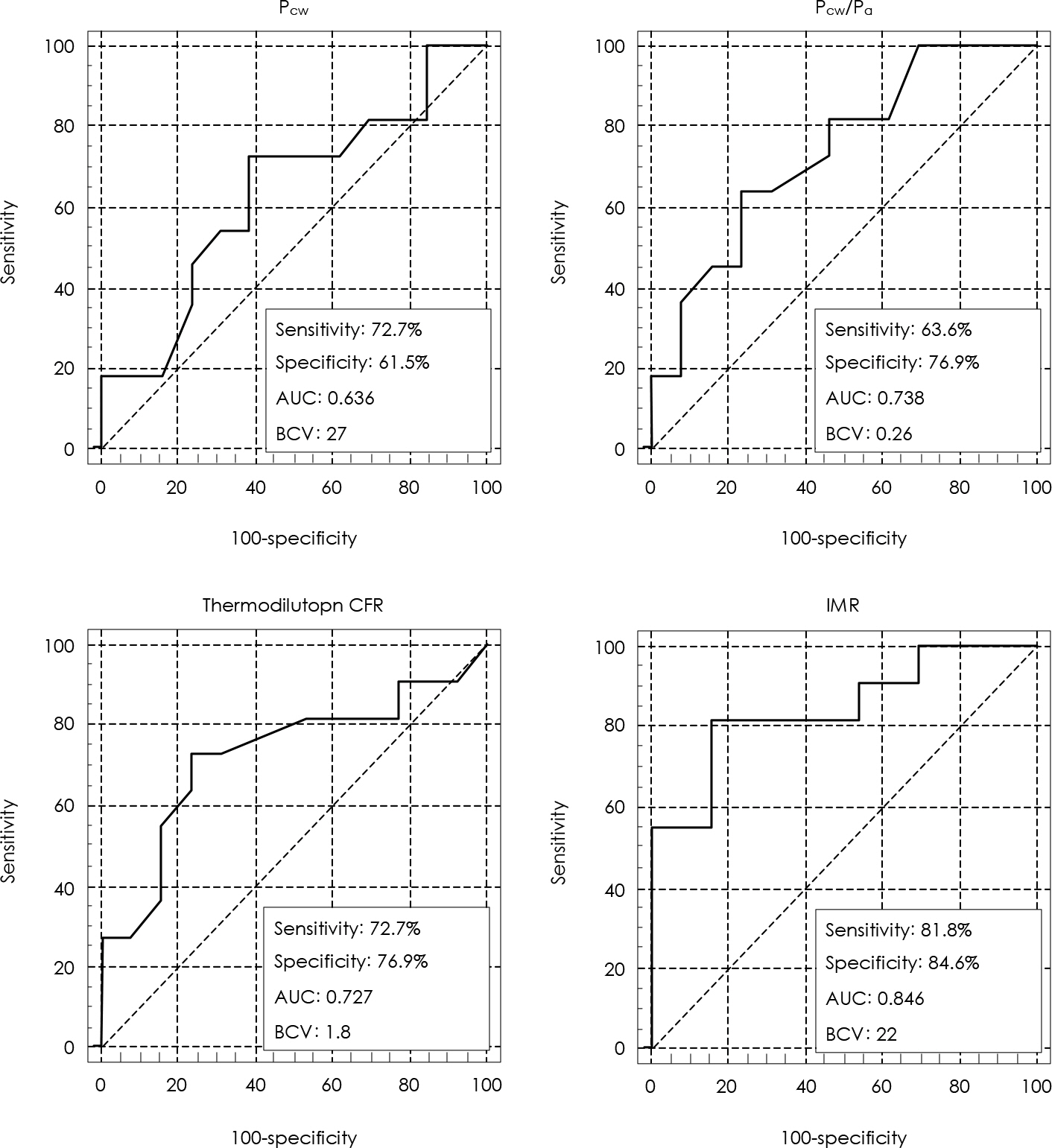
There were good correlations between all the coronary pressure measurements and the regional FDG uptake (CFRthermo, r=0.454, p=0.026; Pcw, r=-0.407, p=0.048; Pcw/Pa, r=-0.480, p=0.018; IMR, r=-0.696, p<0.001, respectively). Multiple logistic regression analysis demonstrated that the IMR was an adjusted predictor for myocardial viability as defined by the 50% FDG-PET threshold value among all the coronary pressure measurements (OR=0.884, p=0.021). The cut-off value of IMR for predicting myocardial viability was 22 U (a sensitivity of 82%, a specificity of 85% and an accuracy of 85%).
CONCLUSIONS
Intracoronary pressure wire-based indexes are useful for on-site assessment of myocardial viability after primary PCI. IMR is a novel index that represents the microvascular integrity, and it is a better predictor of myocardial damage than the current techniques for evaluating the microvasculature after primary PCI.
MeSH Terms
Figure
Reference
-
References
1. Bonow RO. Identification of viable myocardium. Circulation. 1996; 94:2674–80.
Article2. Ito H, Tomooka T, Sakai N, et al. Lack of myocardial reperfusion immediately after successful thrombolysis: a predictor of poor recovery of left ventricular function in anterior myocardial infarction. Circulation. 1992; 85:1699–705.3. Maes A, van de Werf F, Nuyts J, Bormans G, Desmet W, Morte-mans L. Impaired myocardial tissue perfusion early after successful thrombolysis: impact on myocardial flow, metabolism, and function at late follow-up. Circulation. 1995; 92:2072–8.4. Yoon MH, Tahk SJ, Choi SY, et al. Microvascular integrity and ventricular function according to early ST-segment resolution in acute myocardial infarction. Korean Circ J. 2003; 33:183–95.
Article5. Choi SY, Tahk SJ, Yoon MH, et al. Comparison of TIMI myocardial perfusion grade with coronary flow reserve for prediction of recovery of LV function and LV remodeling in acute myocardial infarction. Korean Circ J. 2004; 34:247–57.
Article6. Yoon MH, Tahk SJ, Choi SY, et al. Effect of distal protection device on the microvascular integrity during primary stenting in acute myocardial infarction: distal protection device in acute myocardial infarction. Korean Circ J. 2005; 35:106–14.
Article7. Topol EJ, Ellis SG, Cosgrove DM, et al. Analysis of coronary angioplasty practice in the United States with an insurance-claims data base. Circulation. 1993; 87:1489–97.
Article8. Gibson CM, Cannon CP, Murphy SA, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation. 2000; 101:125–30.
Article9. Kern MJ. Coronary physiology revisited: practical insights from the cardiac catheterization laboratory. Circulation. 2000; 101:1344–51.10. De Bruyne B, Pijls NH, Smith L, Wievegg M, Heyndrickx GR. Coronary thermodilution to assess flow reserve: experimental validation. Circulation. 2001; 104:2003–6.11. Pijls NH, De Bruyne B, Smith L, et al. Coronary thermodilution to assess flow reserve: validation in humans. Circulation. 2002; 105:2482–6.12. Fearon WF, Farouque HM, Balsam LB, et al. Comparison of coronary thermodilution and Doppler velocity for assessing coronary flow reserve. Circulation. 2003; 108:2198–200.
Article13. Fearon WF, Balsam LB, Farouque HM, et al. Novel index for invasively assessing the coronary microcirculation. Circulation. 2003; 107:3129–32.
Article14. Yamamoto K, Ito H, Iwakura K, et al. Pressure-derived collateral flow index as a parameter of microvascular dysfunction in acute myocardial infarction. J Am Coll Cardiol. 2001; 38:1383–9.
Article15. Yoon MH, Tahk SJ, Choi SY, et al. Comparison between microvascular integrity indexes assessed by pressure/doppler wire and %FDG uptake in AMI following primary PCI. Korean Circ J. 2006; 36:701–9.
Article16. Saha GB, MacIntyre WJ, Brunken RC, et al. Present assessment of myocardial viability by nuclear imaging. Semin Nucl Med. 1996; 26:315–35.
Article17. Udelson JE. Steps forward in the assessment of myocardial viability in left ventricular dysfunction. Circulation. 1998; 97:833–8.
Article18. Topol EJ. Textbook of Interventional Cardiology. 4th ed.Philadelphia: Saunders;2003. p. 832–3.19. Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985; 5:587–92.20. Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998; 97:535–43.21. Segall G. Assessment of myocardial viability by positron emission tomography. Nucl Med Commun. 2002; 23:323–30.
Article22. Teiger E, Garot J, Aptecar E, et al. Coronary blood flow reserve and wall motion recovery in patients undergoing angioplasty after myocardial infarction. Eur Heart J. 1999; 20:285–92.23. Lepper W, Hoffmann R, Kamp O, et al. Assessment of myocardial reperfusion by intravenous myocardial contrast echocardiography and coronary flow reserve after primary percutaneous transluminal coronary angiography in patients with acute myocardial infarction. Circulation. 2000; 101:2368–74.
Article24. Bax M, de Winter RJ, Schotborgh CE, et al. Short- and long-term recovery of left ventricular function predicted at the time of primary percutaneous coronary intervention in anterior myocardial infarction. J Am Coll Cardiol. 2004; 43:534–41.
Article25. de Bruyne B, Bartunek J, Sys SU, Pijls NH, Heyndrickx GR, Wijns W. Simultaneous coronary pressure and flow velocity measurements in humans: feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation. 1996; 94:1842–9.26. Ng MK, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation. 2006; 113:2054–61.27. Chamuleau SA, Siebes M, Meuwissen M, Koch KT, Spaan JA, Piek JJ. Association between coronary lesion severity and distal microvascular resistance in patients with coronary artery disease. Am J Physiol Heart Circ Physiol. 2003; 285:H2194–200.
Article28. Aarnoudse W, Fearon WF, Manoharan G, et al. Epicardial stenosis severity does not affect minimal microcirculatory resistance. Circulation. 2004; 110:2137–42.
Article29. Fearon WF, Aarnoudse W, Pijls NH, et al. Microvascular resistance is not influenced by epicardial coronary artery stenosis severity: experimental validation. Circulation. 2004; 109:2269–72.30. Shimada K, Saknoue Y, Kobayashi Y, et al. Assessment of myocardial viability using coronary zero flow pressure after successful angioplasty in patients with acute anterior myocardial infarction. Heart. 2003; 89:71–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Myocardial Viability Using PET
- Defect of 18F-FDG Uptake Observed in Infarcted Myocardium Showing Reverse Redistribution on Rest / 24-Hour Delayed 201Tl Myocardial SPECT after Acute Myocardial Infarction
- A Case of Acute Myocardial Infarction Associated with Myocardial Bridge Treated by Primary Coronary Stenting
- Index of Microcirculatory Resistance as Predictor for Microvascular Functional Recovery in Patients with Anterior Myocardial Infarction
- Correlation between Thrombolysis in Myocardial Infarction, the Myocardial Perfusion Grade and the Myocardial Viability Indices after Primary Percutaneous Coronary Intervention in ST Segment Elevation Myocardial Infarction