Korean Circ J.
2007 Dec;37(12):616-622. 10.4070/kcj.2007.37.12.616.
Epicardial Conduction Properties and Electrocardiographic Characteristics of Premature Ventricular Complexes or Ventricular Tachycardias That Originate at the Aortic Cusp
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Korea University Medical Center, Anam Hospital, Seoul, Korea. yhkmd@unitel.co.kr
- KMID: 2227036
- DOI: http://doi.org/10.4070/kcj.2007.37.12.616
Abstract
-
BACKGROUND AND OBJECTIVES: Premature ventricular contraction (PVC) or ventricular tachycardia (VT) that originates from the aortic cusp (AC) has a similar left bundle branch block (LBBB) pattern with a inferior axis as those LBBB patterns originating from the right ventricular outflow tract, but the electrocardiogram (ECG) characteristics are distinct. We sought to characterize the ECG morphology of PVCs or VTs from the AC and to assess whether these foci exit out to the surrounding epicardium by preferential conduction, resulting in an ECG with epicardial foci.
SUBJECTS AND METHODS
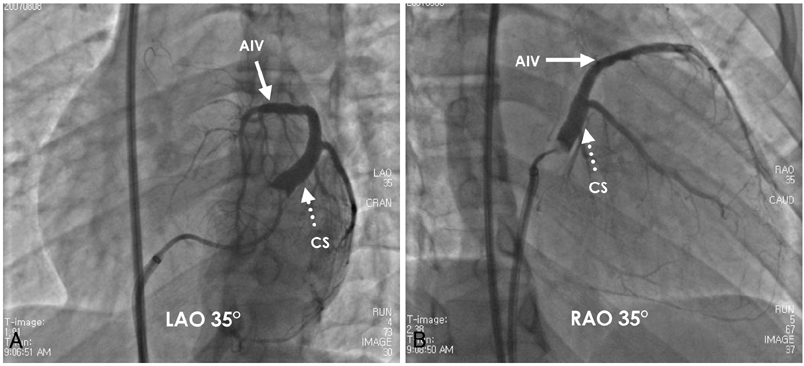
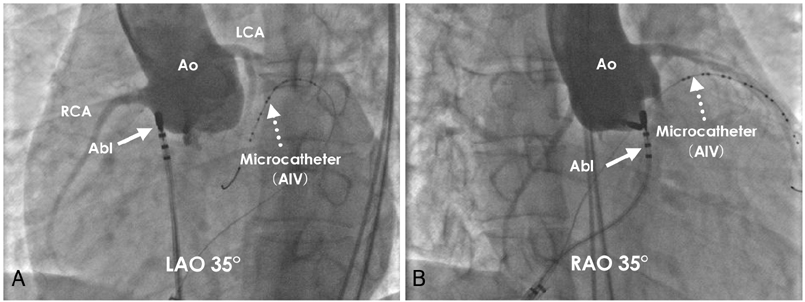
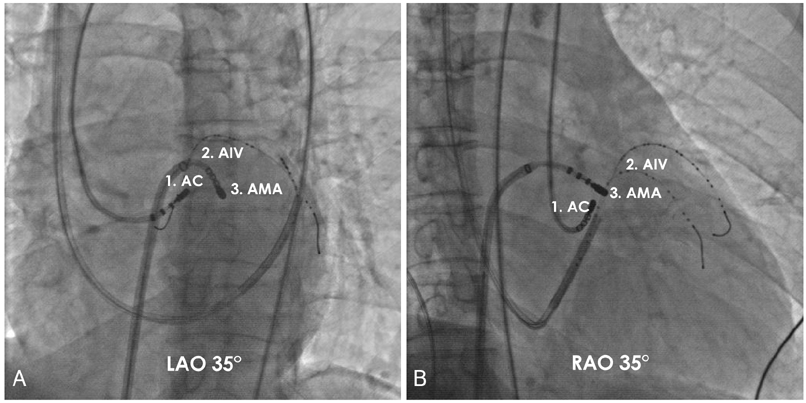
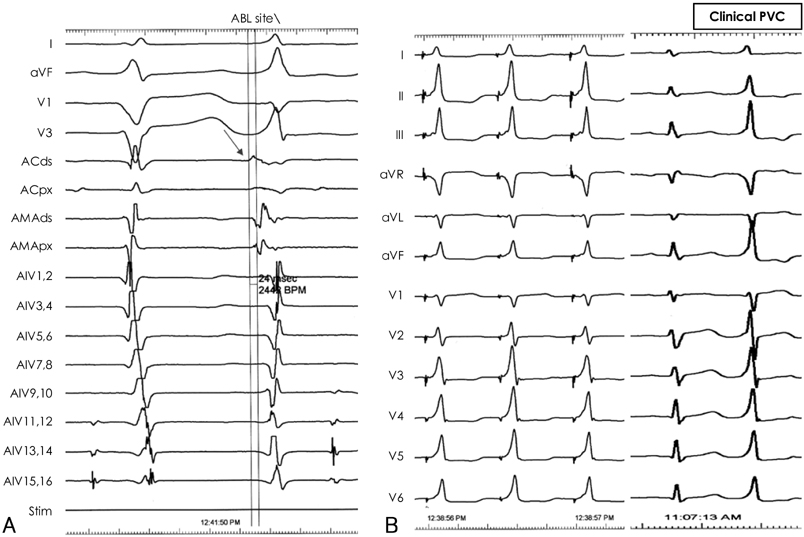
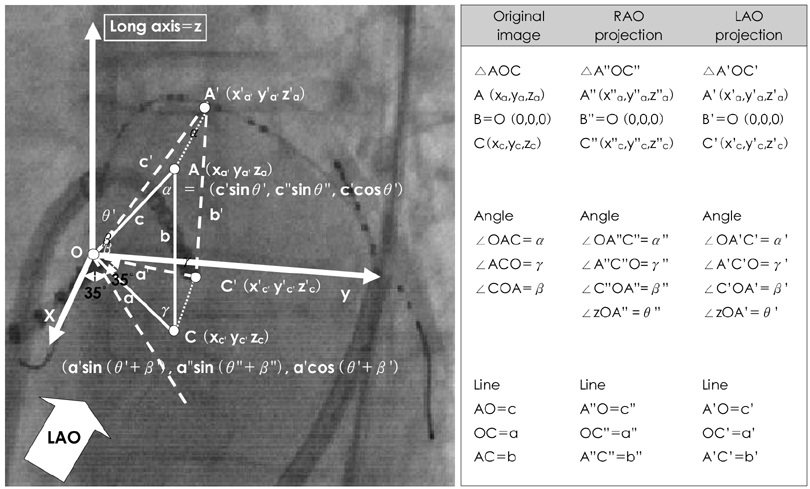
The study subjects were ten patients (M:F=6:4, 40.9+/-11.6 years old) with VTs or PVCs that originated from the AC and they underwent radiofrequency catheter ablation (RFCA). We performed simultaneous activation mapping at the AC, the anterior interventricular vein (AIV) and the anterior mitral annulus (AMA). The conduction velocities (CV) between the successful ablation site to the epicardium in the AIV, and the endocardial earliest activation (EA) site at the AMA were calculated by triangular algebra at right anterior oblique (RAO) 35degrees and left anterior oblique (LAO) 35degrees, respectively.
RESULTS
Successful ablation sites were above the left coronary cusp (LCC) in 7 patients, above and beneath the right coronary cusp (RCC) in 1 patient each, respectively, and beneath the LCC in 1 patient. The QRS width was 149.2+/-19.9 ms, the maximal depolarization time (MDT) was 88.9+/-14.9 ms and the ratio of the MDT to the QRS was 59.5+/-5.7%. The PVC from the LCC had rS or S waves in lead I and R or RS waves in V1, whereas those from the RCC had R waves in lead I and an rS wave in V1. The CV between the successful ablation site at the AC to the epicardial EA site (1.7+/-0.8 m/s) was faster than that to the endocardial EA site (0.8+/-0.4 m/s, p<0.05). CONCLUSION: Most of the PVC/VTs from the AC originated from the above LCC and they displayed a faster CV to the epicardial side of the AIV than that to the endocardial side of the AMA. This suggests the existence of preferential conduction from the AC to the left ventricle (LV) epicardium.
MeSH Terms
Figure
Reference
-
1. Morady F, Kadish AH, DiCarlo L, et al. Long-term results of catheter ablation of idiopathic right ventricular tachycardia. Circulation. 1990. 82:2093–2099.2. Klein LS, Shih HT, Hackett FK, Zipes DP, Miles WM. Radiofrequency catheter ablation of ventricular tachycardia in patients without structural heart disease. Circulation. 1992. 85:1666–1674.3. Coggins DL, Lee RJ, Sweeney J, et al. Radiofrequency catheter ablation as a cure for idiopathic tachycardia of both left and right ventricular origin. J Am Coll Cardiol. 1994. 23:1333–1341.4. Movsowitz C, Schwartzman D, Callans DJ, et al. Idiopathic right ventricular outflow tract tachycardia: narrowing the anatomic location for successful ablation. Am Heart J. 1996. 131:930–936.5. Lee MY, Rho TH, Jin SW, et al. Electrocardiographic predictors for successful radiofrequency catheter ablation in patients with idiopathic ventricular tachycardia showing left bundle branch block and inferior axis. Korean Circ J. 2001. 31:884–893.6. Ouyang F, Fotuhi P, Ho SY, et al. Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp: electrocardiographic characterization for guiding catheter ablation. J Am Coll Cardiol. 2002. 39:500–508.7. Daniels DV, Lu YY, Morton JB, et al. Idiopathic epicardial left ventricular tachycardia originating remote from the sinus of valsalva: electrophysiological characteristics, catheter ablation, and identification from the 12-lead electrocardiogram. Circulation. 2006. 113:1659–1666.8. Kanagaratnam L, Tomassoni G, Schweikert R, et al. Ventricular tachycardias arising from the aortic sinus of valsalva: an underrecognized variant of left outflow tract ventricular tachycardia. J Am Coll Cardiol. 2001. 37:1408–1414.9. Callans DJ, Menz V, Schwartzman D, Gottlieb CD, Marchlinski FE. Repetitive monomorphic tachycardia from the left ventricular outflow tract: electrocardiographic patterns consistent with a left ventricular site of origin. J Am Coll Cardiol. 1997. 29:1023–1027.10. Hachiya H, Aonuma K, Yamauchi Y, Igawa M, Nogami A, Iesaka Y. How to diagnose, locate, and ablate coronary cusp ventricular tachycardia. J Cardiovasc Electrophysiol. 2002. 13:551–556.11. Srivathsan K, Lester SJ, Appleton CP, Scott LR, Munger TM. Ventricular tachycardia in the absence of structural heart disease. Indian Pacing Electrophysiol J. 2005. 5:106–121.12. Lee SR, Cho JG, Park OY, et al. Clinical characteristics of ventricular tachycardia. Korean Circ J. 2001. 31:894–899.13. Miles WM. Idiopathic ventricular outflow tract tachycardia: where does it originate? J Cardiovasc Electrophysiol. 2001. 12:536–537.14. Tada H, Nogami A, Naito S, et al. Left ventricular epicardial outflow tract tachycardia: a new distinct subgroup of outflow tract tachycardia. Jpn Circ J. 2001. 65:723–730.15. Obel OA, d'Avila A, Neuzil P, Saad EB, Ruskin JN, Reddy VY. Ablation of left ventricular epicardial outflow tract tachycardia from the distal great cardiac vein. J Am Coll Cardiol. 2006. 48:1813–1817.16. Timmermans C, Rodriguez LM, Crijns HJ, Moorman AF, Wellens HJ. Idiopathic left bundle-branch block-shaped ventricular tachycardia may originate above the pulmonary valve. Circulation. 2003. 108:1960–1967.17. Lerman BB, Stein KM, Markowitz SM, Mittal S, Slotwiner DJ. Ventricular arrhythmias in normal hearts. Cardiol Clin. 2000. 18:265–291.18. Tanner H, Hindricks G, Schirdewahn P, et al. Outflow tract tachycardia with R/S transition in lead V3: six different anatomic approaches for successful ablation. J Am Coll Cardiol. 2005. 45:418–423.19. Hachiya H, Aonuma K, Yamauchi Y, et al. Electrocardiographic characteristics of left ventricular outflow tract tachycardia. Pacing Clin Electrophysiol. 2000. 23:1930–1934.20. Moorman AF, Christoffels VM. Cardiac chamber formation: development, genes, and evolution. Physiol Rev. 2003. 83:1223–1267.21. Hasdemir C, Aktas S, Govsa F, et al. Demonstration of ventricular myocardial extensions into the pulmonary artery and aorta beyond the ventriculo-arterial junction. Pacing Clin Electrophysiol. 2007. 30:534–539.22. Volkmer M, Antz M, Hebe J, Kuck KH. Focal atrial tachycardia originating from the musculature of the coronary sinus. J Cardiovasc Electrophysiol. 2002. 13:68–71.23. Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998. 339:659–666.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventricular premature complexes and associated factors in the early postinfarction period
- The Effect of Oral Mexiletine on Ventricular Arrhythmias Evaluation by Holter Monitoring
- Risperidone-induced Ventricular Premature C omplexes: A Case Report
- Electrocardiographic Predictors for Successful Radiofrequency Catheter Ablation in Patients with Idiopathic Ventricular Tachycardia showing Left Bundle Branch Block and Inferior Axis
- Radiofrequency Ablation of Recurrent Ventricular Premature Complex Originating from near Left Ventricular Summit Guided by Intracardiac Echocardiography